Abstract
Background
Due to its small size, variable shape, and lack of distinct anatomical landmarks, osteoarthritic knees make a precise patellar resection extremely difficult.
Methods
We performed virtual patellar resection with digital software using three dimensional computed tomography scans of knees from 49 patients who underwent primary total knee replacement at our hospital. We compared 2 commonly used resection methods, the tendon method (TM) and the subchondral method, to determine an ideal resection plane with respect to the symmetry and thickness of the patellar remnant.
Though patellofemoral complications contribute as one of the main factors responsible for reoperation after total knee replacement (TKR), patellar resurfacing is not generally given as much importance as the femoral or tibial resections by surgeons during TKR.1-3) Due to its small size, variable shape, and lack of distinct anatomical landmarks, osteoarthritic knees in particular, a precise patellar resection is extremely difficult. Although rotational alignment and antero-posterior positioning of the femoral component influences patellofemoral mechanics, it is also significantly influenced by the accuracy of the patellar resection, with the resultant thickness and symmetry of the patella-implant composite.4-8)
Asymmetric resurfacing results in a higher incidence of anterior knee pain and abnormal patellar tracking, in comparison to knees with symmetric patellar profiles.4,9) The depth of bone resection and the bone prosthesis composite thickness significantly influence knee function following TKR. An over-resection resulting in a thin patella can increase the risk of stress fracture and antero-posterior instability.7,8,10) An under-resection on the other hand, causes overstuffing of the joint, thereby increasing contact forces and may reduce knee flexion.5,7) The shape of the resected surface of the patella has a relationship to the coverage obtained with the prosthesis.3,5,11)
In an effort to improve the symmetry of patellar resection, Anglin et al.9) had compared different radiographic definitions of desired resection lines. The fact that their study was based on two dimensional radiographs, however, has been quoted by them as a limitation of their study. Using three-dimensional computerized tomography (3D-CT) analyses, Iranpour et al.12) found that the width thickness ratio of the patella can be used to assess the premorbid patellar thickness, which they believed, has to be restored by the bone-prosthesis composite. However, they were uncertain as to whether restoring the premorbid thickness may result in overstuffing the joint in the osteoarthritic patellae. They did their study on relatively normal patellae and did not assess the symmetry of resection or the shape of the resected surface of the patella. This prompted us to perform a 3D-CT study on osteoarthritic patellae, assessing all these morphological parameters to compare 2 commonly used methods of patellar resection, i.e., the tendon method (TM),11,13,14) and the subchondral method (SCM).12,15,16) Such a quantitative comparison using 3D-CT on the diseased patellae has not been reported thus far. The purpose of our study was to compare the morphology of the resected patellae between the TM and the SCM using 3D-CT based virtual resection and assess the usefulness of these data as a guide for the surgeon in determining an ideal resection plane during patellar resurfacing.
Fifty 3D-CT scans of knees from 49 female patients, who underwent primary TKR for osteoarthritis at our hospital between March 2008 and October 2008, were evaluated. Exclusion criteria included any other pathologic condition other than primary osteoarthritis, as well as valgus aligned knees. All the patients had a preoperative CT scan of their diseased knee (Brilliance CT 64-Channel Scanner, 3rd Generation, Philips, Netherlands) in a high-resolution mode using the 512 × 512 pixel matrix. Patients were supine with the involved limb in the extended position during scanning. All consecutive slices were imported into a 3D-CT reconstruction program (Lucion, Infinitt, Seoul, Korea) (Fig. 1). All patients were older than 62 years (range, 62 to 83 years). All of the above patients had patella-femoral osteoarthritis (Skyline Kellgren and Lawrence grade ≥ 2)17) and had received patellar resurfacing during the operation. All patients with very severe osteoarthritic changes and badly deformed patellae, where the bony landmarks were grossly obscured in the 3D-CT scans were excluded from the study. The morphological parameters that were assessed were the pre-resection thickness of the whole patella, the post-resection thickness, the width and height of the resected surface of the patella, and the symmetry of resection, with both the TM and SCM.
The TM involves resection through a plane that passes through the posterior limits of the quadriceps tendon medially and laterally and the patellar tendon inferiorly.11,13,14) The SCM involves resecting the patella at the level of the subchondral bone of the lateral facet.12,15,16) After setting up the Lucion software, the patella was aligned in the sagittal plane with the median ridge inferiorly and the anterior surface superiorly. The thickness of the patella was then measured, as the vertical distance from the midpoint of the median ridge to the dorsal surface (Fig. 2). A virtual resection in the axial plane was made at this level. This image and the 3D sagittal image were used to define a plane parallel to the anterior surface and just down to the subchondral bone of the lateral facet to virtually reproduce the SCM of resection (Fig. 3). To reproduce the TM, we used the 3D axial and sagittal images and the 2D sagittal image to select 3 points, one each at the posterior limits of the quadriceps tendon medially and laterally and one at the posterior limit of patellar tendon inferiorly, where the Hounsfield units changed from fat (negative) to fasciatendon (positive), just outside the bone. These 3 points defined the plane of resection for the TM (Fig. 4). After the 3D virtual resection was made, thickness of the resected patella was measured at the midpoint of the cut surface height in the sagittal plane. The width and height of the cut surface were measured in the 2D image as shown in Fig. 3C.
Gomes et al.2) had described a method of assessing the mediolateral (ML) symmetry of the resected patella. Measuring the thickness 15 mm from the medial and lateral margins of the patella, the resection is considered asymmetric when the difference between the 2 levels is > 2 mm, and as a major asymmetry when > 4 mm.1) However, since these 2 points were too close to the center of the patella in most of our patients, we chose to assess the ML symmetry by measuring the thickness of the resected patella at the midpoints of the medial and lateral halves of the patella (Fig. 5A). The superoinferior (SI) symmetry had not been quantitatively assessed in any previous reported studies. We assessed the SI symmetry similar to the manner in which the ML symmetry was assessed, by measuring the thickness at the midpoints of the superior and inferior halves of the cut surface height in the sagittal plane (Fig. 5B).
All statistical analyses were done using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) and p-values less than 0.05 were considered statistically significant. The student t-test was employed to compare independent data. In order to achieve precision of the measurements, all measurements were done independently by a research fellow (SGN) and a 4th year resident (DYP), on 2 separate occasions with a gap of one week between measurements. The intraclass correlation coefficients for intra and inter-observer agreement were assessed. The intraclass correlation coefficient was found to be higher than 0.818 for inter-observer agreement, and was 0.967 for intra-observer agreement.
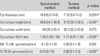
There were 27 left knees and 23 right knees in our study. The mean thickness of the patella before virtual resection with the 3D-CT was 21 mm (range, 18.3 to 23.6 mm; standard deviation [SD], 1.24), and the mean width was 40.9 mm (range, 34.5 to 48.8 mm; SD, 3.17). The mean post-resection thickness with TM was 11.6 mm (range, 9.4 to 14.5 mm; SD, 0.93) and with SCM, 10.9 mm (range, 8.6 to 14.6 mm; SD, 1.2) the mean difference being 0.7 mm (p = 0.0014). The cut surface height was 28.8 mm (range, 24.2 to 36.9 mm) for SCM and 31.8 mm (range, 28.3 to 36.5 mm) for TM and the cut surface width was 40 mm (range, 35.3 to 45.1 mm) and 38.3 mm (range, 33.3 to 43.9 mm), respectively. The mean width to height (W/H) ratio of the cut surface was 1.21 with TM, and 1.39 with the SCM (p < 0.0001). The mean difference between the medial and lateral thicknesses (representing the ML symmetry) of the resected patella was 0.68 (range, 0.1 to 1.8 mm; SD, 0.55) with TM, and 0.7 mm (range, 0.1 to 1.8 mm; SD, 0.52) with SCM. The mean difference between the superior and inferior thicknesses (representing the SI symmetry) of the resected patella was 0.88 mm (range, 0.1 to 2.5 mm; SD, 0.63) with the TM and 0.43 mm (range, 0 to 1.6 mm; SD, 0.32) with SCM (p < 0.001). Thus, both methods gave a symmetric patellar resection mediolaterally, as well as superoinferiorly, with the ML and SI thickness difference being less than 2 mm. The differences in various measurements after virtual resection with both methods are summarized in Table 1.
We found significant morphological differences of the resected patella between SCM and TM. In terms of thickness, TM resulted in a thicker patella. In addition, it resulted in a more round shape compared to SCM. Both methods, by definition, produced a symmetric SI and ML cut, yet SCM resulted in a significantly better SI symmetry.
Patellar resurfacing was not included as a part of TKR during earlier days and the incidence of anterior knee pain was reported to be as high as 50%.18,19) Later studies have shown that, resurfacing the patella has a role in reducing anterior knee pain.14,20) Patellar resurfacing, however, is associated with complications that account for up to half of all revision TKRs.11,21) Precise surgical techniques can go a long way in avoiding these complications. The depth and symmetry of patellar resection, which are often overlooked by surgeons, can significantly influence the occurrence of these complications.5-8,22)
Asymmetric patellar resection is found to be associated with anterior knee pain, bony impingement, patellar maltracking, plastic overload, and increased wear.1,4) Both the SI and ML symmetry have an important influence on the outcome following patellar resurfacing.9,21) We found that both the tendon and the SCMs gave a symmetric resection in the ML plane, since the mean ML thickness difference was 0.68 mm (range, 0.1 to 1.8 mm) with TM and 0.7 mm (range, 0.1 to 1.8 mm) with SCM, both values being less than 2 mm. We could not come across any previous study assessing the SI symmetry of patellar resection. Both methods gave a symmetric resection superoinferiorly with a mean SI thickness difference of 0.88 mm (range, 0.1 to 2.5 mm) with TM and 0.43 mm (range, 0 to 1.6 mm) with SCM, both values being less than 2 mm. However, the SI thickness difference was higher with the TM compared to the SCM (p < 0.001), the inferior thickness being lesser in all the cases. This is explained by the fact that the patellar tendon has a more anterior insertion on the patella compared to the quadriceps tendon. So, the TM gives a slightly more oblique resection compared to the SCM, where the resection is done almost parallel to the anterior surface of the patella (Fig. 6).
When resurfacing the patella, it is desirable that the surgeon makes an attempt to restore the thickness of the bone-prosthesis composite to that of the original patella.10,22) There are many studies that suggest leaving a minimum patellar thickness of 13 to 16 mm after resection.10,23) Kim et al.3) has reported a mean patellar thickness of 21.2 mm and a post-resection thickness of 12.5 mm in 713 female Korean patients. Though there is concern that a thinner resected patella may have increased strain and a higher risk of fracture, Kim et al.3) had only one case of periprosthetic fracture in their series, in a patient who sustained it following a fall. Thus, a resected patella, which is thinner than the minimum recommended value in literature (13 to 16 mm), may still be acceptable for Korean patients.
The mean pre-resection thickness measured with the 3D-CT scan in our study was 21 mm (range, 18.3 to 23.6 mm), which was lesser than the intraoperative value of 21.62 mm (range, 20 to 24 mm). This is probably explained by the fact that the articular cartilage and prepatellar soft tissue, both of which contribute to the thickness measured intraoperatively,12,24) are not included in the measurements done with the 3D-CT. Rauh et al.,24) after a cadaver study using spiked calipers to measure patellar thickness has mentioned that the intraoperative measurements, which are usually done with a smooth mouthed caliper, can result in an overestimation of the thickness due to the prepatellar soft tissue. The mean post-resection thickness in our study was 11.59 mm (range, 9.39 to 14.50 mm) with the TM and 10.85 mm (range, 8.56 to 14.64 mm) with the SCM. Thus, the TM gave a thicker resected patella with a mean difference of 0.7 mm (p = 0.0014). Intraoperative post-resection thickness was 12 mm (range, 9 to 15 mm) for the above patients.
The W/H ratio of the resected surface gives an idea about its approximate shape, which when round, has a value of 1, and tends to have higher values for more oval shapes.5) The W/H ratio of the cut surface in our study was 1.21 with the TM and 1.39 with the SCM, which means that the TM gives a less oval shape compared to the SCM (p < 0.0001). This is because the cut surface height was more (mean difference of 3 mm), and the cut surface width was less (mean difference of 1.7 mm), with the TM compared to the SCM. A less oval shape for the resected surface, as obtained with the TM in our study, in turn gives better coverage for the more commonly used domed prosthesis. Lee and Kim13) suggests that, the TM of resection may reduce surgical variations associated with patellar resurfacing using a domed prosthesis. Ledger et al.11) mentions that, in comparison to an oval patellar prosthesis, a domed prosthesis can tolerate an oblique cut better, remaining in contact with the trochlear groove even with asymmetric cuts. There are concerns about the possibility of implanting an oval prosthesis in malrotation.5)
Our study has limitations. First of all, this study was done on female subjects only. The differences between female and male patella dimensions have been reported, with males showing higher values for width, height, and W/H ratio.5) The main reason for solely using female subjects was due to the lack of male patients during the time span in which this study was undertaken. In Korea, as well as in other Asian countries, the ratio of female to male patients receiving TKR is even more lopsided than in Western countries. According to the Korean Health Insurance Review and Assessment Service data between years 2002 to 2005, among the 47,961 patients who had received TKR, 43,513 (90.7%) were female. Secondly, the preoperative 3D-CT tool described in our study may not be available to all facilities. The cost effectiveness of taking a CT on TKR subjects is unknown. Most importantly, the landmarks chosen for virtual resection with 3D-CT reconstruction need not accurately coincide with the landmarks used for resection during surgery. Intraoperatively, the subchondral junction is not as reliably identifiable as the posterior limits of the quadriceps and patellar tendon attachments. Thus, the virtual resections performed with 3D-CT may be difficult to be accurately reproduced intraoperatively. We believe, however, that 3D-CT was the most practical, as well as ethical way to compare the 2 resection methods on the above mentioned parameters.
In conclusion, our results give the surgeon an idea about the difference in resected morphology between the 2 methods. We found that when compared to SCM, the TM gives a thicker resected patella and a less oval shape to the cut surface, which gives better coverage for a domed prosthesis. Surgeons may choose the TM when a thicker resected patella is needed, or vice versa. Some surgeons may want to medialize the prosthesis for optimal patella tracking, in which case the SCM may be chosen for a more oval cut surface. ML and SI symmetry was achieved with both methods, but the SI symmetry was slightly better with the SCM. Surgeons may choose SCM in order to achieve a more symmetric superior-inferior cut surface to prevent periprosthetic fractures. Though the TM has shown a statistical edge over SCM in terms of post-resection thickness and the cut surface shape, to determine its actual clinical significance, and to determine the most appropriate patellar resection method, further prospective intraoperative studies with long-term clinical follow-up are warranted.
Figures and Tables
Fig. 1
Reconstruction of three-dimensional (3D) computed tomography images of the knee using specialized computer software. Note the corresponding coronal, sagittal and axial views (2D images) together with the 3D knee image.

Fig. 3
Subchondral method showing the plane of resection (white dotted line) in the two-dimensional (2D) axial (A) and 3D sagittal (B) images, and the cut surface in the 2D coronal image (C) showing the cut surface width (W) and height (H) (black line).

Fig. 4
Anatomic landmarks chosen (white arrows) for resection at the fat fascia-tendon junctions, for the tendon method of resection. Posterior limits of the quadriceps tendon medially (A) and laterally (B) and one at the posterior limit (C) of patellar tendon inferiorly, where the Hounsfield units changed from fat (negative) to fascia-tendon (positive), just outside the bone. These 3 points defined the plane of resection for the tendon method.
Fig. 5
A-B measurement of the medial (white arrow) and lateral thickness (dotted arrow) for mediolateral symmetry (A) and superior (white arrow) and inferior thickness (dotted arrow) for superoinferior symmetry (B).

Fig. 6
A schematic representation of the resection planes with the 2 methods. The subchondral method gives a resection surface almost parallel with the anterior surface (green oval), while the tendon method gives a more oblique resection plane (red oval), shown here slightly exaggerated (red arrows). This demonstrates why the cut surface height is more with tendon method (Ht) than with the subchondral method (Hs).

ACKNOWLEDGEMENTS
The authors gratefully acknowledge the financial support of the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (A 084120).
References
1. Baldini A, Anderson JA, Cerulli-Mariani P, Kalyvas J, Pavlov H, Sculco TP. Patellofemoral evaluation after total knee arthroplasty: validation of a new weight-bearing axial radiographic view. J Bone Joint Surg Am. 2007. 89(8):1810–1817.
2. Gomes LS, Bechtold JE, Gustilo RB. Patellar prosthesis positioning in total knee arthroplasty: a roentgenographic study. Clin Orthop Relat Res. 1988. (236):72–81.
3. Kim TK, Chung BJ, Kang YG, Chang CB, Seong SC. Clinical implications of anthropometric patellar dimensions for TKA in Asians. Clin Orthop Relat Res. 2009. 467(4):1007–1014.

4. Pagnano MW, Trousdale RT. Asymmetric patella resurfacing in total knee arthroplasty. Am J Knee Surg. 2000. 13(4):228–233.
5. Baldwin JL, House CK. Anatomic dimensions of the patella measured during total knee arthroplasty. J Arthroplasty. 2005. 20(2):250–257.

6. Bengs BC, Scott RD. The effect of patellar thickness on intraoperative knee flexion and patellar tracking in total knee arthroplasty. J Arthroplasty. 2006. 21(5):650–655.

7. Hsu HC, Luo ZP, Rand JA, An KN. Influence of patellar thickness on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty. 1996. 11(1):69–80.

8. Kurosaka M, Yoshiya S, Mizuno K, Yamamoto T. Maximizing flexion after total knee arthroplasty: the need and the pitfalls. J Arthroplasty. 2002. 17:4 Suppl 1. 59–62.

9. Anglin C, Fu C, Hodgson AJ, Helmy N, Greidanus NV, Masri BA. Finding and defining the ideal patellar resection plane in total knee arthroplasty. J Biomech. 2009. 42(14):2307–2312.

10. Levai JP. Technical aspects: the patellar side. Knee Surg Sports Traumatol Arthrosc. 2001. 9:Suppl 1. S19–S20.

11. Ledger M, Shakespeare D, Scaddan M. Accuracy of patellar resection in total knee replacement: a study using the medial pivot knee. Knee. 2005. 12(1):13–19.

12. Iranpour F, Merican AM, Amis AA, Cobb JP. The width: thickness ratio of the patella: an aid in knee arthroplasty. Clin Orthop Relat Res. 2008. 466(5):1198–1203.
13. Lee TQ, Kim WC. Anatomically based patellar resection criteria for total knee arthroplasty. Am J Knee Surg. 1998. 11(3):161–165.
14. Lombardi AV Jr, Mallory TH, Maitino PD, Herrington SM, Kefauver CA. Freehand resection of the patella in total knee arthroplasty referencing the attachments of the quadriceps tendon and patellar tendon. J Arthroplasty. 1998. 13(7):788–792.

15. Rand JA. Morrey BF, editor. Total knee arthroplasty: techniques. Joint replacement arthroplasty. 1991. New York, NY: Churchill Livingstone;1002–1003.
16. Insall JN. Insall JN, editor. Surgical techniques, instrumentation in total knee arthroplasty. Surgery of the knee. 1993. New York, NY: Churchill Livingstone;767–768.
17. Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957. 16(4):494–502.

18. Healy WL, Wasilewski SA, Takei R, Oberlander M. Patellofemoral complications following total knee arthroplasty: correlation with implant design and patient risk factors. J Arthroplasty. 1995. 10(2):197–201.
19. Koh JS, Yeo SJ, Lee BP, Lo NN, Seow KH, Tan SK. Influence of patellar thickness on results of total knee arthroplasty: does a residual bony patellar thickness of <or=12 mm lead to poorer clinical outcome and increased complication rates? J Arthroplasty. 2002. 17(1):56–61.

20. Parvizi J, Rapuri VR, Saleh KJ, Kuskowski MA, Sharkey PF, Mont MA. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res. 2005. 438:191–196.

21. Komistek RD, Dennis DA, Mabe JA, Walker SA. An in vivo determination of patellofemoral contact positions. Clin Biomech (Bristol, Avon). 2000. 15(1):29–36.

22. Kelly MA. Patellofemoral complications following total knee arthroplasty. Instr Course Lect. 2001. 50:403–407.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download