Abstract
Unlike meniscal tears and chondral defects, the mucoid degeneration of the anterior cruciate ligament (ACL) is a rare cause of knee pain and there have been no case reports of mucoid degeneration of both the ACL and the posterior cruciate ligament (PCL). A 48-year-old-male patient presented with knee pain and limitation of motion. The patient's magnetic resonance imaging, arthroscopic findings, and pathologic diagnosis confirmed a clinical diagnosis of mucoid degeneration of both the ACL and the PCL. The symptoms disappeared after arthroscopic partial excision of the ACL and PCL.
Unlike meniscal tears and chondral defects, the mucoid degeneration of the anterior cruciate ligament (ACL) is a rare cause of knee pain.1-8) There have been several reports of mucoid degeneration of the ACL alone, but to our knowledge, there has been no report of mucoid degeneration of both the ACL and posterior cruciate ligament (PCL). Therefore, we report a case of the mucoid degeneration of both the ACL and PCL that was diagnosed by magnetic resonance imaging (MRI), arthroscopy, and histology.
A 48-year-old man presented with right knee pain that had been ongoing for 10 years prior and had not been the result of trauma; He presented with difficulty in full extension or squatting. This right knee pain had been aggravated 4 years prior. The patient had received conservative treatment that included medication with non-steroidal anti-inflammatory drugs from other hospitals over the prior 2-3 years, but the symptoms had not improved. Physical examination revealed mild swelling, quadriceps atrophy, and a positive McMurray's test. There was no evidence of joint line tenderness. The Lachman test, anterior and posterior drawer and pivot shift tests, and maneuvers for rotator instability were all negative. The range of motion was a flexion contracture of 5° and a further flexion of 130° with mild pain exacerbated by full extension or full flexion at the posterior aspect of the knee joint. Plain radiograph of the right knee joint showed mild degenerative changes and the notch-width index of the femur was 0.213 (Fig. 1). Both ACL and PCL had inhomogeneous signal intensity and diffuse hypertrophic changes on the T1-weighted, proton-density and T2-weighted images of MRI (Fig. 2). The menisci were normal.
At arthroscopy, there was no meniscal pathology medially or laterally. There was no ligamentum mucosum. However, there were mild grade 1 or 2 articular surface changes in the medial tibial plateau and in the medial femoral condyle. Both ACL and PCL were intact, but which was no longer enveloped by the synovium, and showed yellowish, hypertrophic changes. The hypertrophic ACL and PCL filled the entire intercondylar notch and caused impingement. There was no gross evidence of cyst or ganglion formation within the ligament. The ligament demonstrated appropriate tension when probed and when an anterior or posterior drawer test was applied. A biopsy was performed on the hypertrophic portion of both the ACL and PCL. We performed a partial excision for normal appearing shape of ACL and PCL to avoid impingement (Fig. 3). The femoral intercondylar notch was in an unusual reverse-trapezoid shape. After the arthroscopic procedure, we examined the instability, in which tested negative. On the histological examinations of both the ACL and the PCL, faint purple-colored mucoid materials were seen between the collagen fibers, which were consistent with mucoid or myxoid degeneration of ligament (Fig. 4).
Postoperatively, the patient was allowed to bear weight and to perform knee motion as tolerated. He had full active and passive ranges of motion without pain at 2 weeks after the operation. As of the 24-month follow-up, there were no symptoms or objective findings of knee instability and he returned to full activity.
Mucoid degeneration of the ACL is a rare cause of knee pain.1-8) This lesion of the ACL was first reported by Kumar et al.3) in 1999. They reported that a biopsy indicated mucoid degeneration and a relief of symptoms could be obtained through arthroscopic partial resection of the ligament. Since their report, several authors have reported on this lesion as a cause of knee pain,1,2,4-8) and recently, a relatively high incidence has been reported.9) However, to our knowledge, there has been no report about the mucoid degeneration of both the ACL and the PCL in the English literature.
The patients who had mucoid degeneration of ACL usually complained of knee pain and an extension or flexion deficit. The origin of the knee pain in this lesion is still in question. However, previous reports have supported that the pain may originate from a mechanical cause rather than through chemical mediators.1,9) Mechanical impingement of an hypertrophic ACL might cause extension pain associated with limited extension.9) The tensioning of the diseased anteromedial bundle (or posterolateral bundle) of the ACL during flexion (or extension) may cause flexion (or extension) pain associated with flexion (or extension) deficit.1,5) Narvekar and Gajjar7) suggested that the volume of the ACL and tension within the ligament was responsible for these symptoms. Thus, it can be proposed that PCL may cause a pain and motion deficit similar to that of the ACL. In our case, the patient presented with knee pain and difficulty in both full extension and in full flexion. At arthroscopy, ACL and PCL filled the entire intercondylar notch. Thus, we performed partial excision to the normal appearing shape for ACL and PCL to avoid impingement. It was thought that this patient had knee pain due to mucoid degeneration of the PCL as well as the ACL.
MRI is the most useful examination for differentiating between mucoid degeneration of the ACL and intraligamentous ganglion, as well as other lesions in the knee joint. McIntyre et al.4) described this lesion of ACL as a "celery stalk" on MRI examination, because of the diff use high signal with subtle appearance of some linear, low-signal intensity fibers parallel to the long axis of the ligament. In our current case, both the ACL and the PCL showed similar hypertrophic patterns on MRI. In contrast, the MRI finding of ganglion cysts was hyperintense signal intensity on T2-weighted images with sharp demarcation.4)
For the treatment of mucoid degeneration of the cruciate ligament, partial excision or debridement with or without notchplasty is usually performed. According to previous reports, notchplasty depended on whether the impingement would be resolved or not after the debridement of hypertrophic mucoid materials.6,7,9) Most authors have reported satisfactory results after these procedures without instability.1-3,6,7,9) In our case, we excised both the ACL and the PCL in part, and it resulted in complete relief of pain and full range of motion without instability.
Figures and Tables
 | Fig. 1Anteroposterior, tunnel and lateral radiographs of the right knee joint show mild arthritic changes. |
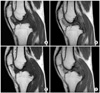 | Fig. 2Sagittal images of anterior (A, B) and posterior (C, D) cruciate ligaments on magnetic resonance imaging show inhomogeneous intensity and hypertrophy (T1-weighted [A, C] and T2-weighted [B, D], respectively). |
References
1. Fealy S, Kenter K, Dines JS, Warren RF. Mucoid degeneration of the anterior cruciate ligament. Arthroscopy. 2001. 17(9):E37.

2. Hsu CJ, Wang SC, Fong YC, Huang CY, Chiang IP, Hsu HC. Mucoid degeneration of the anterior cruciate ligament. J Chin Med Assoc. 2006. 69(9):449–452.

3. Kumar A, Bickerstaff DR, Grimwood JS, Suvarna SK. Mucoid cystic degeneration of the cruciate ligament. J Bone Joint Surg Br. 1999. 81(2):304–305.

4. McIntyre J, Moelleken S, Tirman P. Mucoid degeneration of the anterior cruciate ligament mistaken for ligamentous tears. Skeletal Radiol. 2001. 30(6):312–315.

5. Melloni P, Valls R, Yuguero M, Saez A. Mucoid degeneration of the anterior cruciate ligament with erosion of the lateral femoral condyle. Skeletal Radiol. 2004. 33(6):359–362.

6. Motmans R, Verheyden F. Mucoid degeneration of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2009. 17(7):737–740.

7. Narvekar A, Gajjar S. Mucoid degeneration of the anterior cruciate ligament. Arthroscopy. 2004. 20(2):141–146.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download