This article has been
cited by other articles in ScienceCentral.
Abstract
Background
Proximal phalangeal fractures are common fractures of the hand. The fractures are difficult to treat because of vicinity of two important joints and crossing long tendons. The purpose of this study was to evaluate the efficacy of nail traction technique in the management of proximal phalangeal fractures of the hand.
Methods
Patients (n=43) with proximal phalangeal fractures were treated by nail traction and evaluated prospectively. We assessed all the patients at the time of presentation and then followed a standard protocol for recruiting patients. After application of nail traction, the patients were initially assessed at 12th day. The outcome measures included post reduction radiographic evaluation and total active motion (TAM) in finger at the final follow-up appointment. All the patients were followed for one year.
Results
The post-reduction X-ray evaluation showed good reduction in 33 cases, fair reduction in 8 and poor reduction in 2 cases. At final assessment, 35 patients had good TAM score, six had fair and two had poor TAM score. Complications were noted in two patients and these included pressure necrosis in palm and stiffness in proximal interphalangeal joint.
Conclusions
The results of this prospective study show that with careful selection of patients, nail traction seems to be simple, safe and effective technique for managing proximal phalangeal fractures.
Keywords: Proximal phalangeal fractures, Conservative treatment, Nail traction, Hand fractures, Digital splint
Phalanges are the most common sites for fractures in the hand.
1,
2) If not managed properly, these apparently minor fractures can result in long lasting deformity due to reduction in the range of motion in the adjacent joints.
3) The annual incidence of phalangeal fractures is 2.9%.
3) They are more common in the male age group 20-29 years.
3-
7) Proximal phalangeal fractures constitute about 13% of all hand fractures.
4) Various mechanisms have been reported in literate to cause these fractures. The most common mechanisms include road traffic accidents, industrial injuries, falls and sport related injuries.
3,
4)
Proximal phalangeal fractures are difficult to treat irrespective of the mode of treatment. Surgical stabilization can result in further tissue trauma resulting in adherence of soft tissues and reduction in the range of movement in the adjacent joints.
5) In addition to that, the internal fixation devices can interfere with tendon gliding. The conservative techniques such as splints and braces on the other hand may not be able to maintain the reduced position. This can result in delayed union or malunion. Any prolonged immobilization can result in stiffness of the joints and require long-term physical therapy.
The objective of treating hand fractures is to obtain fracture union in acceptable alignment and early mobilization to prevent stiffness.
6,
7) With metacarpophalangeal (MCP) joint flexed at 90 degrees, the proximal phalangeal fractures are usually held in reduction.
5,
8) The collateral ligaments of the MCP joint in flexed position are taut with minimal chances of stiffness due to contracture. The extension of proximal interphalangeal (PIP) joints prevents volar plate contracture.
6) The longitudinal traction applied in this position makes the extensor and flexor tendons tense, which provides dorsal and volar stability.
This study reports the results of 43 proximal phalangeal fractures which were managed by a nail traction technique. Longitudinal traction was applied through the finger nail. The soft tissues around the proximal phalanx were made tense with traction to provide stability and maintain reduction.
METHODS
Study Design
In this prospective study 106 consecutive phalangeal fractures were managed in a single orthopaedic unit. A total of 70 (67%) of these fractures affected proximal phalanges, and out of these, 43 fractures were selected for nail traction. The recruitment criteria is shown in
Fig. 1. The indications for inclusion included one or more of the following:
Functionally unstable fractures. For functional stability we used criteria described earlier by Pun et al.9) They described those fractures as functionally stable in which the patients could actively move the adjacent joint (MCP and PIP joints) more than 30% of the expected range while the alignment of fracture remained within acceptable range.9) If the patient was not able to move the adjacent joint more than 30% of the expected range or the movement resulted in malalignment then the fracture was defined as functionally unstable.
Unacceptable radiographic alignment. An alignment was considered acceptable if the angulation was less than 10° in both coronal and sagittal planes.9)
Some of type 1 open fractures according to the classification described by Swanson et al.10)
Other treatment methods for proximal phalangeal fractures included: aluminium splint alone without traction for four cases, strapping and mobilization for six cases, scaphoid slab after reduction for six cases, and surgical stabilisation in 11 cases. The patients were initially assessed in the accident and emergency department by an orthopaedic resident. Informed consent was obtained for the procedure and for inclusion in the study. The protocol for including for nail traction is shown in
Fig. 1.
Technique for Applying Nail Traction
The steps for application of nail traction are shown in
Fig. 2A-C. Under aseptic conditions, a digital block was given with 2% plain lidocain to the injured finger. Using a cutting needled suture of 3-0 prolene a bite was then taken at the distal one third of the nail (non-germinal part) from distal to proximal with the needle caressing between the nail and nail bed. A second bite was then taken in the reverse direction and the ends of the suture were left free at this stage.
The aluminium splint was pre-bent before incorporating it in the below-elbow slab. The first bend measuring 90° was at one inch from the distal end. The next bend was made measuring an angle 70-80° to accommodate the MCP joint. The third bend was made measuring an angle of 45° to accommodate the wrist dorsiflexion.
Then the aluminium splint was incorporated in the below elbow plaster of Paris (POP) slab by sandwiching it in between the two sets of POP slab (
Fig. 2A). After this the surgeon held the tip of the finger and reduced the fracture and then maintained the reduction firmly. Meanwhile the assistant tied the free ends of the prolene to the distal bent part of the aluminium splint (
Fig. 2B). The knot was then firmly secured to the aluminium splint with adhesive tape to prevent it from slipping. The amount of force for traction was variable among the patients and was equivalent to the force just to maintain the fracture in reduced position without distraction.
Gauze rolled up into balls was kept in between the splint and finger at the apex of the deformity to nullify the deforming forces and bandage applied to secure the cast in place (
Fig. 2C). To prevent rotational deformity it was ascertained by the surgeon that the fingernail was parallel to horizontal before application of bandage while the MCP joint flexed at 90°. In this position the bandage was applied after medial and lateral padding to minimise the risk of rotational deformity. At this point check radiographs were taken in AP and lateral views (
Fig. 3). If reduction was not satisfactory slight manipulation was done by extending or bending the aluminium splint at its distal bend. Also altering the position of gauze balls might help with obtaining a desirable position.
Immobilization and Rehabilitation
If the alignment was acceptable (
Fig. 4) then the immobilization in the aluminium splint was continued and the patient was advised to keep the hand elevated during the first week. Clinical union was tested at 12 days by eliciting tenderness at fracture site. If there was no tenderness the splint was discarded and protected mobilization was started by the physiotherapist with adjacent finger strapping which continued for one week. Thereafter free active assisted mobilisation was initiated until full recovery was achieved. When the fracture site was tender, the traction was released but the splint was continued for a maximum of another week. The recovery times ranged from 6 to 18 weeks, but all the patients were followed up for one year.
Outcome Measures
The outcome measures we used in this study included post-reduction radiological evaluation and total active motion at final assessment.
For post-reduction radiological evaluation the following criteria were used: 1) good: anatomical reduction or angulation less than 10 degrees in both planes, 2) fair: angulation between 11 degrees and 20 degrees, and 3) poor: angulation more than 20 degrees and any degree of rotation. Based on the total active motion (TAM) the results were graded into three grades: 1) good: TAM 210° or more, 2) fair: TAM between 180° and 210°, 3) poor: TAM less than 180°.
RESULTS
Out of 70 proximal phalangeal fractures, 43 were managed by nail traction. Of the remaining 27 fractures, four were treated by aluminium splint alone without traction and six were managed by strapping and mobilization. Another six cases were managed with a scaphoid slab after reduction, and surgical stabilisation was used in 11 cases. In this study we only included the cases which had nail traction. There were 25 (58%) male and 18 (42%) female patients. In 23 of these patients the left hand was injured, the right hand in 20. The average age was 32 years (range, 13 to 69 years). Majority of the patients (n = 20) were between 25 to 50 years of age. Among the remaining patients, 17 were below 25 years of age and six were above 50 years. The mechanisms of injury included; industrial/workplace injuries (13), assault (6), road traffic accidents (7), domestic injuries (12) and sport injuries (5). Among the 43 patients, 24 were manual labourers or construction workers, 11 housewives, 3 students, and 5 office workers.
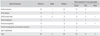
The proximal phalanx fractures were classified as open or closed. In addition they were classified depending upon the location and configuration of fracture. Different fracture patterns and post-reduction X-ray evaluation are shown in
Table 1. There were five open and 38 closed fractures. The middle finger was involved in 15 cases, the ringer finger 12 cases, the index finger in 10 cases and little finger in 6 cases. The most common location was the shaft of the proximal phalanx, which was involved in 28 fractures, followed by proximal metaphyseal fractures (11 cases), neck fractures (2 cases) and epiphyseal fractures (2 cases). Depending on fracture configuration, there were 18 transverse fractures, 15 oblique fractures and 6 comminuted fractures. The remaining four fractures also involved the proximal metaphysis but could not be classified as transverse, oblique or comminuted. Two of these fractures were type 2 epiphyseal fractures and two had intra-articular extension.
Depending upon the angulation at the fracture site the post-reduction radiographs were graded as good, fair and poor. Good reduction was achieved in 33 cases. Fair reduction was noted in eight cases while two cases had poor reduction. The patients with either fair or poor reduction had repeat reduction and a check radiograph to achieve acceptable reduction.
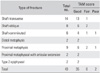
Table 2 shows the functional assessment at the final appointment. Good function was achieved in 35 patients and fair in six. Poor function (TAM less than 180°) was noted in two patients. When compared to post-reduction radiological evaluation, there was a shift of from fair to good results in two cases. This was probably achieved by early mobilization.
Complications were noted in two patients. These included pressure necrosis due to the aluminium splint at the 5th metacarpal head and stiffness in the PIP joint. We thought that the cause of pressure necrosis was inadequate padding under the aluminium splint. The patient with pressure necrosis needed flexor sheath release. The patient with stiffness and extensor lag was treated with scar massage and physiotherapy. This patient had an open wound on the dorsum of the finger at the time of injury. This patient eventually had a complete recovery.
DISCUSSION
Fractures of the proximal phalanx in the hand are difficult to treat because of the presence of an important joint on either end of this bone.
11,
12) Important flexor and extensor tendons cross this bone for distal attachment. The aim of the treating surgeon is not only to achieve timely union with good alignment but also to preserve the gliding mechanisms of these tendons. Usually in the sagittal plane, the fracture adapts a palmar apical configuration with the proximal fragment in flexion and the distal fragment in extension. This is because the intrinsic muscles flex the MCP joint, hence the proximal fragment is in flexion. The distal fragment goes into extension due to the short excursion of the extensor tendon hood and lateral bands.
5) When reduced properly, the fracture can be held by using a splint with traction and the stabilizing effect of tense soft tissues.
13)
The treatment options include open reduction and internal fixation, external fixators and conservative modalities. Open reduction and internal fixation can cause further soft tissue damage which can result in impairment of the gliding layers.
12,
14,
15) However, surgical management becomes necessary in unstable, irreducible and open fractures with soft tissue damage.
6,
16) We treated 11 cases with internal fixation. The indications for internal fixation included; unstable fractures with failed nail traction, fracture of multiple fingers, open fractures with soft tissue damage and intra-articular fractures with small fragments. Out of these 11 fractures we noted good results in 4 (36.3%) cases, fair in 4 (36.3%) and poor in 3 (27.2%).
Conservative management on the other hand avoids additional soft tissue damage and theoretically should be associated with less loss of range of motion in the adjacent joints if early mobilization is guaranteed.
5,
6) However, it is important to appreciate that the conservative treatment is only effective when intact muscle tendon units and other soft tissue can be utilised to hold the reduction.
5)
There have been previous studies on management of proximal phalangeal fractures with traction splints. Koul et al.
13) reported the results of 39 proximal phalangeal factures treated with a custom made traction splint. They used adhesive glue to fix the traction to an over nail plate and reported excellent results in 72% of the patients, good results in 22% and poor results in 6%. None of the patients in this group with transverse fractures were treated by traction splint; they suggested that internal fixation is more favourable for transverse fractures. In our series 18 (42%) cases of transverse fractures were treated by digital splint and nail traction. This shows that if good reduction is achieved under digital block and then maintained with longitudinal traction and proper splinting, then transverse fractures can be treated successfully with traction splints.
Rajesh et al.
12) used a thermoplastic MCP block splint for proximal phalangeal fractures in 32 cases. They did not apply traction on the finger. In their series they reported excellent results in 72%, good in 22% and fair to poor in 6% of the cases, similar to Koul et al.
13) However, their results for patients younger than 50 years were significantly better compared to older patients. They suggested the splint to be continued for 3 to 4 weeks while in our study the splint was removed at the 12th day in more than 80% of cases. We think early protected mobilisation is important to prevent stiffness in adjacent joints.
We recorded complications in two cases. One patient had pressure necrosis of a small area of skin over the 5th metacarpal head. This complication could have been avoided with better padding. The area of necrosis was small but the patient eventually needed flexor sheath release. The second patient had stiffness in the PIP joint. This patient had an open fracture and the wound on the dorsum of the proximal phalanx was closed before the application of nail traction. The stiffness was treated with regular physiotherapy and scar massage. There was no infection nor any other nail bed complications in this series.
All the patients were followed up to one year and no patient was lost to follow-up. All the fractures were treated by a single surgeon (ST). An orthopaedic surgeon and a radiologist assessed the post-reduction radiographs and where there was discrepancy the worst score was chosen. The treating surgeon or his team followed up the patients. Therefore, the follow-up data was not collected independently. This can be considered as weakness of this study. Additionally the study would have been more convincing if two techniques were compared.
The results from this series show that nail traction with digital splint is an effective and safe technique. It is very simple and easy to learn. The aluminium splint can be easily incorporated between layers of the POP slab. It involves a single stitch through the finger nail under local anaesthetic. Most of our cases were closed fractures but open fractures without significant soft tissue damage can be primarily closed and treated by nail traction.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download