Abstract
Background
We evaluated the clinical and radiological results of one-stage correction for cerebral palsy patients.
Methods
We reviewed clinical outcomes and radiologic indices of 32 dysplastic hips in 23 children with cerebral palsy (13 males, 10 females; mean age, 8.6 years). Ten hips had dislocation, while 22 had subluxation. Preoperative Gross Motor Function Classification System (GMFCS) scores of the patients were as follows; level V (13 patients), level IV (9), and level III (1). Acetabular deficiency was anterior in 5 hips, superolateral in 7, posterior in 11 and mixed in 9, according to 3 dimensional computed tomography. The combined surgery included open reduction of the femoral head, release of contracted muscles, femoral shortening varus derotation osteotomy and the modified Dega osteotomy. Hip range of motion, GMFCS level, acetabular index, center-edge angle and migration percentage were measured before and after surgery. The mean follow-up period was 28.1 months.
Subluxation and dislocation of the hip is a major source of disability for children with cerebral palsy, with the incidence ranging between 3% and 75%.1-4) Hip dislocation and subluxation are caused by multiple factors including contraction of muscles, a deformed proximal femur and acetabular deficiency.5,6) Contraction of the adductor and flexor muscles leads to disturbances of the muscular balance of the hip joint region, to deformation of the acetabulum and proximal femur such as coxa valga,7) increase of anteversion and to subsequent hip dislocation and subluxation.8) These issues gradually worsen the acetabular deformity and deficiency, aggravating the hip dislocation and subluxation. Dislocation of the hip is associated with poor sitting balance, pelvic obliquity, scoliosis and difficulty in perineal care.1,9-12) Therefore, preventive treatment for dislocation of the hip is important, and if the hip is dislocated, treatment of the cause and stable reduction of the dislocated femoral head are necessary.1,11,13) It has been suggested that all these problems can be improved with one-stage correction.9,10)
We evaluated the results of single event multilevel surgery for cerebral palsy patients with spastic hip dislocation or subluxation which included soft tissue release, femoral osteotomy and the modified Dega osteotomy.9,10)
From October 2006 to March 2010, we performed single event multilevel surgery for subluxation and dislocation of 32 hips in 23 patients. The mean age at the time of surgery was 8.6 years (range, 2 to 13 years) and the mean follow-up period was 28.1 months (range, 12 to 45 months). There were 13 males and 10 females; 21 of these patients had quadriplegia and 2 had diplegia. 10 hips had dislocation, while 22 had subluxation. Eight cases were bilateral. Using 3 dimensional (3D) computed tomography (CT), we checked the location of the acetabular deficiency preoperatively: deficiencies were posterior in 11, superolateral in 7, anterior in 5, and mixed in 9 (Table 1, Fig. 1). Preoperative Gross Motor Function Classification System (GMFCS) was level V in 13 patients, level IV in 9, and level III in 1. One patient with level III could walk for short distances with hip pain with a hand-held mobility device. Nine patients who were scored at GMFCS level IV could walk for short distances with a walker before onset of hip problems, but all these patients had difficulty in walking after hip subluxation and dislocation. All of the other patients (13 in level V) were unable to walk because of muscle contracture and hip discomfort associated with instability, and had difficulty in maintaining a seated position.
All patients were treated with single event multilevel surgery including open reduction of the dislocated femoral head, release of contracted muscles, varus-derotation-shortening femoral osteotomy and the modified Dega osteotomy. For the patients with bilateral involvement, the more unstable side was treated first, except that release of contracted muscles was performed for both legs in the first operation. After application of a hip spica cast for 6 weeks and rehabilitation with physical therapy for 2-4 weeks, surgery was then performed on the contralateral hips.
Following surgery, a hip spica cast and physical therapy, we evaluated the improvement in hip range of motion (ROM), the degree of pain, comfort while sitting and complications such as postoperative infection at the last follow-up. For assessing comfort while sitting, we checked whether patients could maintain a seated position without body support; for estimating discomfort or pain, the patients' parents were asked whether the pain had decreased worsened or remained about the same. We also evaluated changes in the acetabular index, center-edge angle, migration percentage, redislocation, resubluxation and nonunion on a postoperative anteroposterior radiograph of the pelvis and CT.
After the assessment of contracture in the adductors, iliopsoas, rectus femoris, hamstrings, and Achilles tendon during preoperative physical examinations, lengthening procedures for contracted soft tissues were performed selectively. Among the adductors, tenotomy was first performed in the adductor longus, next in the adductor brevis and finally in the gracilis in sequence until the hip could be abducted normally. Recession of the tendinous portion of the iliopsoas at the pelvic brim, distal transfer of the rectus femoris from the upper pole of the patella to the gracilis and fractional lengthening of the distal hamstring muscles in the musculotendinous junction were performed. For the Achilles tendon, Z-plasty or a Vulpius procedure was conducted based on the result of a Silfverskiold test.14)
With a lateral approach to the proximal femur, femoral shortening and a closing wedge varus derotational osteotomy (VDRO) was performed and fixed with 90° AO blade plate. The amount of femoral shortening was equivalent to the overlapped distance of the proximal and distal portions of the osteotomized femur during slight traction of the leg. The femoral neck-shaft angle was corrected to 115-120° and the anteversion was corrected to 15-20°. The distal fragment of the femur was medialized by about 1 cm.
With an anterior approach, bicortical cuts were made anteriorly over the anterior inferior iliac spine and posteriorly at the greater sciatic notch with either the osteotome or the Kerrison rongeur. A unicortical cut was then made through the outer cortex of the ilium between these two points passing approximately 1-2 cm above the lateral margin of the acetabulum. Under image-intensifier control, the curved osteotome was directed halfway between the inner and outer iliac cortices. Care was taken to stop the osteotome above the triradiate cartilage. Then the acetabulum was rotated laterally and downward using a lamina spreader, hinging on the triradiate cartilage to correct the dysplasia until the acetabular angle was decreased to 15°. The bone graft (usually obtained from the femoral shortening osteotomy or from the iliac bone, of a size slightly larger than that measured from the distracted gap of the osteotomy) was then placed into the osteotomy site. The placement of the bone graft corresponded to where the major acetabular deficiency was found in the 3D CT. In this manner, we could decrease the acetabular angle, increase the coverage of the femoral head and reshape a trough-like deformed acetabulum (Fig. 2).
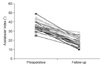
The median postoperative range of abduction of the hip improved from 21.8° (range, 5° to 35°) to 40.0° (range, 30° to 50°) (Fig. 3). Following surgery, 12 (75%) out of the 16 patients who could not maintain a seated position preoperatively were able to sit without a body supporter. Nineteen patients (83%) reported a decrease in pain, 4 (17%) experienced about the same level of pain pre- and postoperatively, and none reported a worsening of pain following treatment. The 6 (26%) patients who were scored at GMFCS level V preoperatively almost improved to level 4 postoperatively. The GMFCS levels of the other 17 patients stayed the same (Table 1). There was no infection or wound problems after surgery.
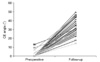
The median acetabular index improved from 35.7° before surgery to 19.0° postoperatively; the median center-edge angle changed from 1.1° to 31.5°; and the migration percentage improved from 74.2% to 10.6% after surgery (Table 1, Figs. 4, 5, 6, 7, 8, 9). All radiologic results improved significantly (p < 0.05). No cases of hip redislocation or resubluxation, in addition to nonunion of the osteotomy site were observed. Even though avascular necrosis (AVN) of the femoral head was observed in 2 cases (6%), these presented no clinical problems.
Early acetabuloplasty, in addition to soft tissue lengthening and VDRO of the proximal femur greatly improves the chances for prolonged hip stability for patients with spastic dislocated hips.6,9,15-18) Many acetabular indices are difficult to measure in cerebral palsy due to hip flexion contracture and the resulting increases in pelvic tilting. Therefore, many authors believe the migration percentage is the most accurate way to monitor hip instability in such patients. It has been recommended that acetabular correction should be performed when the migration percentage is over 50-70%, because the more serious the dislocation of the femoral head, the more likely it is accompanied by acetabular deficiency.19,20) To compare the changes in the acetabulum before and after surgery, we used the coronal image of CT in the measurement of acetabular indices in cases where this had not been taken in the correct position. Analysis of 3D CT of the acetabulum with subtraction of the proximal femur enhanced understanding of the pathology.
Apart from the Dega osteotomy, pelvic osteotomies for the treatment of the dysplastic hip in cerebral palsy include the Salter innominate osteotomy,21) Pemberton acetabuloplasty,17) Chiari osteotomy22,23) and the shelf procedure.18) However, the Salter innominate osteotomy and Pemberton acetabuloplasty are not suitable for all dysplastic hips in cerebral palsy because they are designed mainly to correct anterolateral acetabular deficiency,9) while acetabular deficiency in cerebral palsy exists in various locations. With 3D CT, Kim and Wenger5) demonstrated the variable locations of acetabular deficiency in cerebral palsy: anterior in 29%, superolateral in 15%, posterior in 37%, and mixed in 19%. They reported that the acetabulum showed a trough-like elongated deformity. The Chiari osteotomy and shelf procedure do not use the articular cartilage of the acetabulum to cover the femoral head,9,10) and do not correct the elongated, trough-like deformity of the acetabulum. The modified Dega osteotomy is ideal for these hips by providing selectively improved coverage based on the main area of deficiency (anterior, superiolateral, or posterior) and by reshaping the elongated acetabulum directly.
Since the Dega osteotomy24,25) was first introduced in 1969, many studies have been conducted using this technique.25-27) However, the procedure as originally described did not sufficiently increase coverage of the femoral head, because the posteromedial cortex of the ilium and the greater sciatic notch were not cut (Fig. 10).25-27) To produce better results, Mubarak et al.9) and McNerney et al.10) described the modified Dega osteotomy in which bicortical cuts were made in the anterior inferior iliac spine and the greater sciatic notch. With this modified procedure, posterior coverage of the femoral head is increased by placing a larger bone graft in the posterior part of the osteotomy (Fig. 11). Moreover, while other pelvic osteotomies require internal fixation, more stability is obtained without internal fixation by inserting autologous bone fragments from the ilium or from the proximal femoral shortening osteotomy into the osteotomy site. Elasticity of the osteotomized iliac bone with a hinge at the triradiate cartilage enhances the stability of the bone graft. Chung et al.28) demonstrated the morphometric changes in the acetabulum after Dega osteotomy which is similar to the osteotomy we used. They reported that the anterosuperior, superolateral and posterosuperior covers had improved significantly and the mean acetabular volume increased after the osteotomy.
Although the varization of the proximal femur itself naturally introduces a shortening component and relieves tension around the hip in many cases of subluxation, we added a shortening osteotomy in cases of severe subluxation or dislocation in order to avoid excessive varization of the femur and to reduce the pressure caused by the Dega osteotomy. Harvested material from the shortening procedure was used for the bone graft in the Dega pelvic osteotomy. Additionally, open reduction with capsulorrhaphy was performed at the discretion of the surgeon. Not all patients required open reduction; it was omitted in the less severe cases. In all cases, the hamstrings were lengthened because the soft tissue procedure was conducted before the proximal femoral procedure, although femoral shortening and varization also have a lengthening effect on the hamstrings. Plus, we performed the rectus transfer in some patients since knee flexion was regarded as absolutely necessary for comfort and stability in the seated position in a wheel chair.
The current concept in correction of unstable hips in cerebral palsy maintains bilateral procedures, especially including the contralateral femoral side, to prevent eventual contralateral hip instability and swing-swept hip. With our approach, usually involving no more than soft tissue correction in the less severely affected hip, we have not observed significant suluxation on the contralateral side to date. When further subluxation occurs, a femoral side procedure may be required without delay. All patients in this study showed a coxa valga deformity and increased anteversion of the proximal femur by soft tissue contracture from the first visit. All of them were treated with single event multilevel surgery. Simultaneous correction of multiple problems could extend the operation time, increasing the likelihood of complications. However, if the surgeons are experienced, patients would benefit from the shortened hospitalization and rehabilitation times.
In our patients, stable reduction of the femoral head was followed by a remarkable improvement in abduction. Furthermore, this was achieved without increased pain because of the release of contracted muscles and the increased stability of the hip joint as well as improved comfort in the seated position. The four patients who failed to achieve comfortable sitting experienced the same degree of pain as they had preoperatively. However, all of them were GMFCS level V and were considered to have an abnormal sense of balance caused by the cerebral palsy apart from the problems in their hips. Some of them had scoliosis with fixed pelvic obliquity. The patients who could not maintain a stable seated position solely due to contracted muscles and hip pain, were able to sit comfortably after the operation. As it was difficult to determine the degree of pain or discomfort quantitatively (for example with a VAS score) for our young patients, we interviewed parents about the patients' pain (decreased, maintained or increased). The pain that patients complained of in this study may be considered to be irritability caused by hip motion when the hip is unstable. We believe that this irritability and the contracted soft tissues are the major causes preventing ambulation and of comfort in the seated position. After stable reduction of the hip joint, some of the patients were able to walk again with a walker for short distances, and most could sit comfortably.
We noted AVN of the femoral head in two (6%) hips. This may have been due to occult injury of the vessels supplying the femoral head during open reduction of the femoral head, or during the proximal femoral osteotomy and blade plate insertion. Excessive pressure on the femoral head may be caused by inadequate femoral shortening and/or overly aggressive acetabuloplasty with excessive downward movement of the acetabulum with medial hinging. Despite the AVN of the femoral head, these 2 patients were pain-free, had satisfactory motion of the hip and could sit comfortably. To prevent this complication, careful attention to surgical detail is necessary.
Figures and Tables
Fig. 1
Acetabular deficiency: anterior (A), superolateral (B), posterior (C) and mixed (D), according to 3 dimensional computed tomography.

Fig. 2
A modified Dega acetabuloplasty is performed by cutting bicortically, not only the anterior inferior iliac spine, but also the sciatic notch. The osteotomy includes outer cortices of the ilium of the anterior, middle and posterior portions. It enables a larger graft to be placed posteriorly.

Fig. 7
Radiographs of case 12 (Table 1). This child had spastic quadriplegic cerebral palsy and bilateral hip dislocation. Radiographs were taken preoperatively (A), two (B), and three (C) years after surgery. Improved radiologic indices and a stable hip are evident.

Fig. 8
Two dimensional computed tomography (CT) scans of the same patient (case 12). Coronal CT scans show improved superolateral (A, preoperation; B, postoperation) and posterior (C, preoperation; D, postoperation) coverage of the hip.

Fig. 9
Three dimensional computed tomography images (of the same hip as Fig. 4) show improved superolateral and posterior coverage (A, preoperation; B, postoperation).
Fig. 10
The osteotomy of original Dega acetabuloplasty involves the anterior and middle portions of the inner cortex of the ilium, leaving an intact hinge posteriorly consisting of the intact posteromedial iliac cortex and sciatic notch.2)

References
1. Samilson RL, Tsou P, Aamoth G, Green WM. Dislocation and subluxation of the hip in cerebral palsy: pathogenesis, natural history and management. J Bone Joint Surg Am. 1972. 54(4):863–873.

2. Boldingh EJ, Jacobs-van der Bruggen MA, Bos CF, Lankhorst GJ, Bouter LM. Determinants of hip pain in adult patients with severe cerebral palsy. J Pediatr Orthop B. 2005. 14(2):120–125.

3. Hodgkinson I, Jindrich ML, Duhaut P, Vadot JP, Metton G, Berard C. Hip pain in 234 non-ambulatory adolescents and young adults with cerebral palsy: a cross-sectional multicentre study. Dev Med Child Neurol. 2001. 43(12):806–808.

4. Noonan KJ, Jones J, Pierson J, Honkamp NJ, Leverson G. Hip function in adults with severe cerebral palsy. J Bone Joint Surg Am. 2004. 86(12):2607–2613.

5. Kim HT, Wenger DR. Location of acetabular deficiency and associated hip dislocation in neuromuscular hip dysplasia: three-dimensional computed tomographic analysis. J Pediatr Orthop. 1997. 17(2):143–151.

6. Gamble JG, Rinsky LA, Bleck EE. Established hip dislocations in children with cerebral palsy. Clin Orthop Relat Res. 1990. (253):90–99.

7. Minear WL, Tachdjian MO. Hip dislocation in cerebral palsy. J Bone Joint Surg Am. 1956. 38(6):1358–1364.

8. Fabry G, MacEwen GD, Shands AR Jr. Torsion of the femur: a follow-up study in normal and abnormal conditions. J Bone Joint Surg Am. 1973. 55(8):1726–1738.

9. Mubarak SJ, Valencia FG, Wenger DR. One-stage correction of the spastic dislocated hip: use of pericapsular acetabuloplasty to improve coverage. J Bone Joint Surg Am. 1992. 74(9):1347–1357.

10. McNerney NP, Mubarak SJ, Wenger DR. One-stage correction of the dysplastic hip in cerebral palsy with the San Diego acetabuloplasty: results and complications in 104 hips. J Pediatr Orthop. 2000. 20(1):93–103.

11. Pritchett JW. The untreated unstable hip in severe cerebral palsy. Clin Orthop Relat Res. 1983. (173):169–172.

13. Baker LD, Dodelin R, Bassett FH 2nd. Pathological changes in the hip in cerebral palsy: incidence, pathogenesis, and treatment: a preliminary report. J Bone Joint Surg Am. 1962. 44(7):1331–1411.

14. Kay RM, Rethlefsen SA, Ryan JA, Wren TA. Outcome of gastrocnemius recession and tendo-achilles lengthening in ambulatory children with cerebral palsy. J Pediatr Orthop B. 2004. 13(2):92–98.

15. Gordon JE, Capelli AM, Strecker WB, Delgado ED, Schoenecker PL. Pemberton pelvic osteotomy and varus rotational osteotomy in the treatment of acetabular dysplasia in patients who have static encephalopathy. J Bone Joint Surg Am. 1996. 78(12):1863–1871.

16. Root L, Laplaza FJ, Brourman SN, Angel DH. The severely unstable hip in cerebral palsy: treatment with open reduction, pelvic osteotomy, and femoral osteotomy with shortening. J Bone Joint Surg Am. 1995. 77(5):703–712.

17. Shea KG, Coleman SS, Carroll K, Stevens P, Van Boerum DH. Pemberton pericapsular osteotomy to treat a dysplastic hip in cerebral palsy. J Bone Joint Surg Am. 1997. 79(9):1342–1351.

18. Zuckerman JD, Staheli LT, McLaughlin JF. Acetabular augmentation for progressive hip subluxation in cerebral palsy. J Pediatr Orthop. 1984. 4(4):436–442.

19. Noonan KJ, Walker TL, Kayes KJ, Feinberg J. Varus derotation osteotomy for the treatment of hip subluxation and dislocation in cerebral palsy: statistical analysis in 73 hips. J Pediatr Orthop B. 2001. 10(4):279–286.
20. Song HR, Carroll NC. Femoral varus derotation osteotomy with or without acetabuloplasty for unstable hips in cerebral palsy. J Pediatr Orthop. 1998. 18(1):62–68.
21. Salter RB. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. J Bone Joint Surg Br. 1961. 43(3):518–539.

22. Dietz FR, Knutson LM. Chiari pelvic osteotomy in cerebral palsy. J Pediatr Orthop. 1995. 15(3):372–380.

23. Osterkamp J, Caillouette JT, Hoffer MM. Chiari osteotomy in cerebral palsy. J Pediatr Orthop. 1988. 8(3):274–277.

24. Dega W. Selection of surgical methods in the treatment of congenital dislocation of the hip in children. Chir Narzadow Ruchu Ortop Pol. 1969. 34(3):357–366.

25. Grudziak JS, Ward WT. Dega osteotomy for the treatment of congenital dysplasia of the hip. J Bone Joint Surg Am. 2001. 83(6):845–854.

26. Jozwiak M, Marciniak W, Piontek T, Pietrzak S. Dega's transiliac osteotomy in the treatment of spastic hip subluxation and dislocation in cerebral palsy. J Pediatr Orthop B. 2000. 9(4):257–264.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download