Abstract
Background
The purpose of this study was to assess the intra-articular patterns in the rotational deformities of bucket handle meniscal tears (BHMTs) based on arthroscopic findings and their clinical relevance.
Methods
From 2004 to 2009, 42 patients with a BHMT diagnosed by magnetic resonance imaging underwent arthroscopic surgery. The arthroscopic data (all procedures were recorded) were evaluated retrospectively, and BHMTs were classified according to the rotational directions of centrally displaced fragments. To assess the reliability of the agreement in this classification, 2 orthopedic surgeons re-classified BHMTs, 1 week after first trial. Intra- and interobserver reliabilities were assessed using kappa statistics. In addition, we address specific tear patterns, associated anterior cruciate ligament injury, medio-lateral difference, reducibility, chronicity, and reparability.
Results
Most of the tears could be categorized into one of 3 morphologic patterns. Of the tears, 4.8% could not be categorized. BHMTs were classified, based on the rotational directions of centrally displaced fragments, as follows; the upward rotation group (type 1), the downward rotation group (type 2) and the reverse group (type 3). The most common intra-articular pattern was type 1 (29 patients, 69%). The occurrence of the other patterns was: type 2 in 7 patients (16.7%), type 3 in 4 patients (9.5%); we were not able to make a classification of type in 2 patients (4.8%). Intra-observer reliability was 0.86 in terms of kappa statistics, which implies almost perfect agreement. Mean interobserver reliability (0.73) showed substantial agreement. Type 1 and 2 tears were easily reduced, whereas all type 3 tears (4/4) needed additional procedures to achieve reduction.
For orthopedic surgeons, bucket handle meniscal tears (BHMTs) are particularly challenging lesions, because its rarity precludes experience and arthroscopic visualization is restricted by the fragment of an intercondylar location. To reduce the displaced fragment, treatment is often composed of changing the knee position and pressing the fragment with a probe. Knowledge of the nature of the distorted geometry can simplify not only the reduction, but the procedures such as meniscectomy or meniscal repair. However, some textbooks describe these bucket handle deformities as simply centrally displaced or flipped patterns1,2) and no comprehensive study has been published on this topic. It is our hypothesis that most tears can be categorized into 3 defined patterns and that these patterns occur with a certain frequency that are associated with various tear characteristics, such as associated acute anterior cruciate ligament (ACL) injury, medio-lateral difference, reducibility, chronicity, and reparability.
On a retrospective basis, we performed this study on 61 patients with a BHMT diagnosis by magnetic resonance imaging (MRI) and who had undergone arthroscopic surgery; all the arthroscopic procedures had been recorded. We excluded the cases of discoid meniscus (16 cases). Arthroscopic videos were reevaluated with respect to the intra-articular patterns of rotational deformities. While reviewing arthroscopic findings, we excluded 3 patients due to a lack of data, in addition to the previous exclusions. Overall, 42 patients were enrolled into this study.
There were 41 male patients and 1 female patient with a mean age of 35 years (range, 17 to 65 years; standard deviation, 15 years) (Table 1). The medial meniscus was involved in 31 patients (73.8%) and the lateral meniscus in 11 (26.2%). There was an associated lesion of the ACL in 23 (54.8%). The time from injury to operation ranged from 2 days to 8 years. Fifteen patients (35.7%) with a BHMT were treated by arthroscopic meniscectomy and 27 (64.3%) underwent arthroscopic meniscal repair.
The tear patterns were categorized according to the rotational directions of centrally displaced fragments and were determined by a consensus of 3 orthopedic surgeons. To assess the reliability in classification agreement, 2 orthopedic surgeons re-classified BHMTs, 2 weeks after the first trial. The intra- and interobserver reliabilities of measurements were assessed using kappa statistics.
Reducibility was assessed subjectively as easy (A), moderate (B), or impossible (C) based on the presence of extra procedures. The extra procedures included partial release of neighboring tissues, and additional sutures to improve maneuverability for pulling of the displaced fragment. The A grade was given to those tears with a centrally displaced fragment that was maneuvered easily to the original position by a change in knee position or by use of a probe. In cases of medial meniscal tear, valgus stress was applied to push the displaced meniscal fragment using a probe. Likewise, for the lateral meniscal lesions, "figure of 4" position was applied to reduce the displaced fragment. Those displaced fragments that were getting stuck to or adherent to neighboring tissues that were only able to be relocated with extra procedures were graded as B. Tears with grade C did not require any reduction.
Acute BHMTs were defined as those that presented with a definite history of injury in the 12 weeks before surgery. Chronic tears were defined as those that presented with an onset of symptoms or a history of injury longer than 12 weeks associated with signs of healing and remodeling at the edge of the tear.3)
Intra- and interobserver reliabilities of the agreement in the classification were assessed using kappa statistics. The classic interpretation of kappa statistics is as follows: 0.00-0.20, poor agreement; 0.21-0.40, fair; 0.41-0.60, moderate; 0.61-0.80, substantial; and 0.81-1.00, almost perfect.4) The Fisher's exact test was used to find a correlation between the tear patterns with the associated ACL injury, mediolateral difference, reducibility, chronicity, and reparability.
Most of the tears could be categorized into 3 morphologic patterns. Of the tears, 2 cases could not be categorized. Three groups based on the rotational directions of intercondylar displaced fragments were, namely, the upward rotation group (type 1), the downward rotation group (type 2) and the reverse group (type 3). In type 1, the displaced sharp central margin of the fragment was facing upwards to the femoral side (Fig. 1). In type 2, the displaced sharp central margin of the fragment was facing downwards to the tibial side (Fig. 2). In type 3, the displaced central fragment is turned 180 degrees or more in which the sharp margin of the displaced fragment faces the peripheral side (Fig. 3).
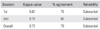
We observed various tear patterns. The most common intra-articular pattern was type 1 (29 patients, 69%). The occurrence of the other patterns was; type 2 in 7 patients (16.7%), type 3 in 4 patients (9.5%). We could not identify the tear margin in the displaced fragments due to severely deformed lesions, and could not classify the type in 2 patients (4.8%). Intra-observer reliability as determined by kappa statistics was 0.86 (Table 1), implying almost perfect agreement. Mean interobserver reliability showed substantial agreement (0.73) (Table 2).
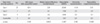
Intra-articular patterns in BHMTs were not associated with combined ACL injury, medio-lateral difference, chronicity, or reparability (p > 0.05). However, the patterns were associated with tear reducibility. Type 1 and type 2 patterns in BHMTs were more easily reducible than type 3, which required additional procedures more frequently than other types (p = 0.00000595 < 0.05) (Table 3). A case in type 1 and a case of type 2 were chronic lesions combined with severely deformed central fragments and adhesion, and were irreducible. In addition, statistical significance was not found between the reducibility and the chronicity (p = 0.142).
The most important finding made during the present study concerned the rotational nature of the deformities in BHMT. To the best of our knowledge, no other comprehensive study has been performed on the deformities in BHMT except that found in one paper.5) Most illustrations of BHMTs have described displacements of central fragments or their being flipped into the intercondylar notch.1,2) In the paper,5) the author described simply the upward and downward rotation of the deformities in BHMT, even then it did not include the reverse group (type 3). We found that the centrally displaced fragment in BHMTs can be rotated upward (type 1), downward (type 2), or reversed (type 3). Because the direction of the displacement is different, we used different methods for relocation between type 1 and 2. In type 1 lesions, we pressed the inferior border of the displaced fragments with a probe and we pressed the superior border of those in type 2 lesions. So the accurate assessment of rotational components is important to reduce the displaced fragment in BHMTs.
Management of BHMTs may entail partial meniscectomy or meniscal repair. However, a recent study showed better results for the repair.6) Preservation is increasingly favored to prevent subsequent arthrosis and to preserve joint kinematics, especially in the physically active and athletic population. Several meniscal repair techniques have been used.7-9) and all involve the repositioning of torn margins as anatomically as possible. For the 15 patients (35.7%) with a BHMT in this series, meniscectomies were performed due to irreducibility and because of degenerative nature. A BHMT extending from the posterior portion and past the middle of the meniscus to the anterior third, allows the displacement beyond the equator of the femoral condyle into the intercondylar notch.1,10) Because it is relatively difficult to assess tears arthroscopically when there is an entrapped intercondylar fragment and possibly due to the rarity of a condition, there are a few technical tips and most rely on using the arthroscopic probe by changing the knee position in order to reduce the fragment. However, good visualization of a tear and assessment of its rotational component can allow arthroscopists to relocate fragments properly.5)
With our own method, reducibility was assessed subjectively as easy (A), moderate (B), or impossible (C) based on the presence of extra procedures. As we mentioned above, the displaced fragments with getting stuck or adherent to neighboring tissues that were only able to be relocated with extra procedures were graded as B. In 4 cases of grade B, we used 3 additional procedures: 1) additional sutures to improve maneuverability for pulling of the displaced fragment in 4 cases, 2) partial release of neighboring tissues in one case. In particular, additional sutures of the vertical type were used based on the method by Yoon et al.,5) and the sutures were used for pulling the device during the reduction.
In 3 of our cases (2 of type 1 and 1 of type 2), we removed the centrally displaced fragments en bloc and we identified that surface remodeling developed in the convex side of displaced fragments. In 2 cases of type 1, the inferior surfaces of displaced fragments were deformed (Fig. 4) and in a case of type 2, the superior surface was irregular. We presumed that the contact surface of the displaced fragments with articular cartilage remained smooth. This finding might be useful for identifying deformed fragments in chronic cases of BHMT. However, additional study is required on this topic.
Some limitations to our study should be noted: first, we included all medial and lateral menisci, regardless of associated ACL injury, and the effects of these on rotational deformity is not known; second, the number of patients was comparatively small, except in tear reducibility (the power was 0.99), the mean power of the other factors was 0.12; third, intra- and interobserver errors may have influenced results, even though we tried to minimize these errors; and fourth, the exact trauma date may not be recalled, the duration between the injury and the operation may not be that accurate, hence leading to inaccuracies in chronicity. This aspect may have further bias in the correlation between the chronicity and reducibility.
In conclusion, based on arthroscopic findings, we were able to describe a comprehensive BHMT classification scheme that encompasses 95.2% of all tears. Tear type was correlated with reducibility.
Figures and Tables
Fig. 1
(A) The two-dimensional figure of "upward rotation" of the displaced fragment (type 1), (B) in arthroscopy.
Fig. 2
(A) The two-dimensional figure of "downward rotation" of the displaced fragment (type 2), (B) in arthroscopy.
Fig. 3
(A) The two-dimensional figure of the flipped fragment in which the central sharp margin of the meniscus faces the peripheral side (type 3), (B) before reduction and (C) during reduction.

References
1. Dandy DJ. The arthroscopic anatomy of symptomatic meniscal lesions. J Bone Joint Surg Br. 1990. 72(4):628–633.

2. Campbell WC, Canale ST, Beaty JH. . Campbell's operative orthopaedics. 2008. 11th ed. Philadelphia: Mosby.
3. Feng H, Hong L, Geng XS, Zhang H, Wang XS, Jiang XY. Second-look arthroscopic evaluation of bucket-handle meniscus tear repairs with anterior cruciate ligament reconstruction: 67 consecutive cases. Arthroscopy. 2008. 24(12):1358–1366.

4. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. 33(1):159–174.

5. Yoon JR, Muzaffar N, Kang JW, Lim HC, Bae JH, Nha KW. A novel technique for arthroscopic reduction and repair of a bucket-handle meniscal tear. Knee Surg Sports Traumatol Arthrosc. 2009. 17(11):1332–1335.

6. Cargill AO, Jackson JP. Bucket-handle tear of the medial meniscus: a case for conservative surgery. J Bone Joint Surg Am. 1976. 58(2):248–251.

7. Bender B, Shabat S, Mann G, Oz H, Adar E. The double-loop technique for meniscal suture. Arthroscopy. 2002. 18(8):944–947.

8. Miura H, Kawamura H, Arima J, et al. A new, all-inside technique for meniscus repair. Arthroscopy. 1999. 15(4):453–455.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download