Abstract
Background
To evaluate the clinical efficacy of three-level anterior cervical arthrodesis with polyethyletherketone (PEEK) cages and plate fixation for aged and osteoporotic patients with degenerative cervical spinal disorders.
Methods
Twenty one patients, who had undergone three-level anterior cervical arthrodesis with a cage and plate construct for degenerative cervical spinal disorder from November 2001 to April 2007 and were followed up for at least two years, were enrolled in this study. The mean age was 71.7 years and the mean T-score using the bone mineral density was -2.8 SD. The fusion rate, change in cervical lordosis, adjacent segment degeneration were analyzed by plain radiographs and computed tomography, and the complications were assessed by the medical records. The clinical outcomes were analyzed using the SF-36 physical composite score (PCS) and neck disability index (NDI).
Results
Radiological fusion was observed at a mean of 12.3 weeks (range, 10 to 15 weeks) after surgery. The average angle of cervical lordosis was 5° preoperatively, 17.6° postoperatively and 16.5° at the last follow-up. Degenerative changes in the adjacent segments occurred in 3 patients (14.3%), but revision surgery was unnecessary. In terms of instrument-related complications, there was cage subsidence in 5 patients (23.8%) with an average of 2.8 mm, and loosening of the plate and screw occurred in 3 patients (14.3%) but there were no clinical problems. The SF-36 PCS before surgery, second postoperative week and at the last follow-up was 29.5, 43.1, and 66.2, respectively. The respective NDI was 55.3, 24.6, and 15.9.
Conclusions
For aged and osteoporotic patients with degenerative cervical spinal disorders, three-level anterior cervical arthrodesis with PEEK cages and plate fixation reduced the pseudarthrosis and adjacent segment degeneration and improved the clinical outcomes. This method is considered to be a relatively safe and effective treatment modality.
Anterior cervical discectomy and fusion (ACDF) with an autogenous iliac bone graft has proven to be effective for the treatment of radiculopathy or myelopathy secondary to cervical spondylosis. However, many authors have reported donor site complications in cases of multi-level fusion.1-3) A range of alternative materials, such as, allografts,4) xenografts,3) Demineralized Bone Matrix (DBM)2) and cages,1,4-11) have been used to avoid this. The polyethyletherketone (PEEK) cage has superior biomechanical properties and a similar elastic coefficient to that of human bone, as well as a reduced stress shielding effect, which reduces the bone weakness and increases the fusion rate. Furthermore, PEEK cages make it easy to determine the status of bone union radiographically.4,6,8,10,12) ACDF with a cage has shown satisfactory clinical results for single level degenerative cervical disorders.4,6,8,10,13) However, this has not been the case with multi-level ACDF for elderly patients.2,14) Furthermore, increased cage subsidence and the loss of cervical lordosis make this method a risky procedure.2,7,15,16) Therefore, this study evaluated the clinical efficacy of the three-level anterior cervical arthrodesis with PEEK cages and plate fixation for aged and osteoporotic patients with degenerative cervical spinal disorders.
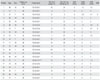
Twenty one patients, who had undergone three-level ACDF with a cage and plate construct for degenerative cervical spinal disorder from November 2001 to April 2007 and were followed-up for at least two years, were enrolled in this study (Table 1). There were 10 men and 11 women with a mean age of 71.7 years (range, 65 to 91 years). The mean follow-up period was 34.1 months (range, 25 to 70 months). Fourteen patients had radiculopathy and 7 patients had symptoms indicating accompanying myelopathy. In terms of the fusion level, there were nine C 3/4, 4/5, 5/6 cases, eight C 4/5, 5/6, 6/7 cases, three C 3/4, 5/6, 6/7 cases, and one C 5/6, 6/7, C7/T1 case. Magnetic resonance imaging (Magnetom Vision, Siemens, Erlagen, Germany) was performed on all patients and the computed tomography myelogram (Somatom Sensation 16, Siemens) was conducted selectively to accurately define the lesion. The bone mineral density was measured in all patients; their average T-score was -2.5 SD.
ACDF was performed at all levels to which the clinical signs and symptoms of the disease were referable, and at which neural element compression was demonstrated by a neuroradiographic study. Cancellous bone for cage insertion was collected using a trocar (diameter 7 mm; AO Synthes, Davos, Switzerland) in the left anterior superior iliac spine. The surgical procedure was performed using a standard anterior Smith-Robinson approach.17) For cage fusion, PEEK cages (Solis, Stryker Spine, South Allendale, NJ, USA) were used and fixed with a rigid metal plate (Peg Plate System, BK Meditech, Seoul, Korea; Cervical Spine Locking Plate, AO Synthes). The patients were advised to wear a Philadelphia cervical collar for 2-4 weeks after surgery, and a soft cervical collar for an additional 2 weeks. Plain lateral and flexion/extension lateral radiographs were used to evaluate bone union at 6 weeks, and 3, 6, 9, and 12 months postoperatively. A CT evaluation was performed if union was uncertain on the radiograph. All radiology evaluations were performed on a digital image using built-in software (Marosis 5.0 PACS viewer, Marotech, Seoul, Korea). Union was defined as less than 2° movement by lateral flexion/extension radiography, bridging bone between endplates, no signs of implant failure of the anterior plate system and < 50% radiolucency of the implant outer surface.18) Cage subsidence was defined as the difference in distance between the center points of the inferior borders of proximal vertebrae and the superior borders of the distal vertebrae at the fusion level, as determined by lateral radiographs postoperatively and at last follow-up. The incidence of cage subsidence and the frequencies at the respective fusion levels were compared. The overall cervical lordosis was defined as the angle between the extended line in the 2nd posterior cervical vertebra and that in the 7th posterior cervical vertebra. For lordosis of fusion segments, the Cobb angle where the extension line of its upper/lower margin meet was selected. Degenerative changes in the adjacent segments were deemed to be present when the degenerative cervical vertebrae were unstable, the height of a disc in the adjacent segment decreased or kyphosis had occurred based on the comparisons of the postoperative and last follow-up radiographs.19) A decrease in the disc height of an adjacent segment was deemed to have occurred when the disc height was < 25% in grade I, 25% to 50% in grade II, 50% to 75% in grade III and > 75% in grade IV.20) Cases with more than grade II were deemed to show degenerative changes in the adjacent segments. The clinical outcomes were analyzed using the SF-36 physical composite score (PCS) and neck disability index (NDI) (Table 2). In addition, the complications associated with screws, plates and cages, and neurological complications and postoperative infections were also documented.
All 21 patients showed bone union after an average of 12.3 weeks (range, 10 to 14 weeks) (Fig. 1). The mean cage subsidence was 2.8 mm (range, 1 to 4.8 mm) in 5 patients (23.8%), which was observed in the anterior and posterior regions at 2 weeks postoperatively. The subsidence observed at 3 months after surgery was similar to that observed at the final follow-up visits (Fig. 2). Subsidence at two-levels was noted in 3 patients and at one level in 2, but this did not cause any clinical problems. Cervical lordosis was 5° before surgery, 17.6° immediately after surgery and 16.5° at the final follow-up visits. Adjacent segment degeneration was detected in 3 patients (14.3%), which included 2 patients with disc space narrowing more than grade II, and 1 patient with instability. However, no clinical problems were encountered.
The SF-36 PCS before surgery, second postoperative week and at the last follow-up was 29.5, 43.1, and 66.2, respectively. The respective NDI was 55.3, 24.6 and 15.9 (Table 2).
Loosening of a plate and screw occurred in 3 patients (14.3%) (Fig. 3), in which a locking screw had not been inserted properly during surgery in 1 and the screws protruded due to cage subsidence in mainly the lower segments during the follow-up in 2. However, these 3 patients had no clinical problems, such as dysphagia or dysphonia at the last physical examination, and no neurological complications or postoperative infection were encountered.
In the case of ACDF for degenerative cervical spinal disease, it has been reported that long-level fusion fails due to complications, such as adjacent segment disease, instability and pseudarthrosis.14,21,22) However, such a result was the outcome of ACDF without plate fixation14,22,23) and the usefulness of plate fixation constructs for multi-level ACDF has been reported.19,24-26) However, complications, such as donor site morbidity, collapse of graft material and the sources of fusion materials in multilevel ACDF, have become an issue, and PEEK cages are being used more frequently as alternatives to bone graft substitutes.4,6,8,10,12) Cho et al.5) conducted a comparative study using three surgical methods, i.e., iliac bone only, iliac bone and a plate construct, and a PEEK cage only. They favored the PEEK cage because it appeared to reduce the number of complications and perioperative bleeding. Similarly, Cho et al.,6) in their comparative study on the use of iliac bone, supported the merits of the PEEK cage, which was found to better maintain physiological lordosis, have a satisfactory fusion rate, make foraminal distraction, and simplify the subsequent radiographic evaluations.
Hwang et al.27) reported that ACDF using cage and plate constructs in multi-level cervical degenerative disc disease had less donor site morbidity and complications related to metals than the multi-level ACDF with iliac strut bone and plate fixation. Nevertheless, these reports suggest that ACDF can be treated satisfactorily with a cage without a plate construct,1,4-11) and that the use of a cage alone produces similar results to conventional ACDF in terms of the fusion rate, stability and the maintenance of disc height.1,4,6,8,10) On the other hand, some reports have voiced concern that development of cage subsidence and loss of lordosis occur when cages are used without plate fixation2,7,15) and reduced contact surface between the cartilage end plates and cages lead to increased instability and related problems.1,4-11)
Few reports have been issued on ACDF and osteoporosis. Natarajan et al.28) reported in an experimental study that the holding power may be increased if graft bones are tightly fitted in an osteoporotic spine. Therefore, the authors considered that firm cage and plate fixation in multi-level ACDF in elderly patients with osteoporosis can achieve a satisfactory union rate, maintain cervical lordosis and reduce cage subsidence. Indeed, in the present study, fusion was obtained at an average of 12.3 weeks postoperatively. Although the fusion period was slower than that for ACDF with an iliac bone and plate construct, which achieved union at 6-10 weeks postoperatively, it was relatively more rapid than ACDF using a cage alone, which has been reported to have a highly variable union period ranging from 3 to 6 months.8,29)
There are some reports of a relatively high incidence of cage subsidence in degenerative cervical disc disease.7,9,15,16) In the present study, cage subsidence occurred in 5 patients (23.8%) with an average of 2.8 mm (range, 1 to 4.8 mm), and was detected in both the anterior and posterior cage region from 2 weeks postoperatively and stopped at 3 months postoperatively. All cases included the distal fusion level, which suggests that the distal portion of the fusion level is where the stress concentrates due to multi-level fusion, and that weakening of the bones due to low bone mineral densities in elderly osteoporotic patients is the main cause of subsidence. However, cervical lordosis was maintained due to plate augmentation. Therefore, cage subsidence was not yet a clinical problem in our patients, but they remain under close observation.
The precise cause of the adjacent segment disease is not known, even though it has been reported that abnormal sagittal balance after ACDF promotes adjacent segment disease.30) Therefore, ACDF with cage and plate constructs was applied to maintain the proper cervical lordosis. In the present study, adjacent segment degeneration occurred in 3 patients (14.3%) but no clinical problems were encountered. Nevertheless, all patients remain under close observation.
In terms of the clinical results after multi-level ACDF, several studies reported satisfactory results with or without plate augmentation.4,25,26) The present study showed that the clinical results through SF-36 and NDI were improved after surgery and at the final follow-up.
In conclusion, three-level anterior cervical arthrodesis with cages and a plate construct is considered an effective treatment modality for elderly patients (> 65 years) with osteoporosis and degenerative cervical spinal disorder. In the present study, the incidence of adjacent segment degeneration and cage subsidence was relatively high, but no clinical correlation was found. Accordingly, this procedure is considered to be safe and effective, and relatively free of serious surgical and implant related complications.
Figures and Tables
Fig. 1
A sixty-nine-year-old woman who had pain in the neck and radiculopathy. (A) Lateral roentgenogram showing narrowing of the disc space and posterior osteophytes from the third to the sixth cervical vertebrae. (B) Lateral roentgenogram taken one day after anterior cervical arthrodesis with a cage and plate construct at C3-4, C4-5, and C5-6. (C) Four years later, lateral roentgenogram showing a solid fusion and physiologic lordosis. (D) Four years later, computed tomogram showing a solid fusion at the C3-4, C4-5, and C5-6 fusion levels.
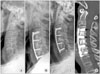
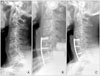
Fig. 2
A seventy-four-year-old woman who had suffered from cervical myelopathy. (A) Lateral roentgenogram showing local kyphosis and narrowing of the disc space from the fourth to the seventh cervical vertebrae. (B) Lateral roentgenogram taken one day after an anterior cervical arthrodesis with a cage and plate construct at C4-5, C5-6, and C6-7. (C) Three years later, lateral roentgenogram showing a cage subsidence at C6-7 fusion level, but showing a solid union. (D) Three years later, computed tomogram showing cage subsidence and fibrous union at the C6-7 fusion level.

Fig. 3
A sixty-six-year-old woman who had pain in the neck and radiculopathy. (A) Lateral roentgenogram showing narrowing of the disc space and posterior osteophytes from the fifth cervical vertebra to the first thoracic vertebra. (B) Lateral roentgenogram taken one day after anterior cervical arthrodesis with a cage and plate construct at the C5-6, C6-7, and C7-T1 levels. (C) Thirty-two months later, lateral roentgenogram showing loosening of a plate and screw at C5 but no neurologic complications occurred.
References
1. Celik SE, Kara A, Celik S. A comparison of changes over time in cervical foraminal height after tricortical iliac graft or polyetheretherketone cage placement following anterior discectomy. J Neurosurg Spine. 2007. 6(1):10–16.

2. Demircan MN, Kutlay AM, Colak A, et al. Multilevel cervical fusion without plates, screws or autogenous iliac crest bone graft. J Clin Neurosci. 2007. 14(8):723–728.

3. Xie Y, Chopin D, Hardouin P, Lu J. Clinical, radiological and histological study of the failure of cervical interbody fusions with bone substitutes. Eur Spine J. 2006. 15(8):1196–1203.

4. Liao JC, Niu CC, Chen WJ, Chen LH. Polyetheretherketone (PEEK) cage filled with cancellous allograft in anterior cervical discectomy and fusion. Int Orthop. 2008. 32(5):643–648.

5. Cho DY, Lee WY, Sheu PC. Treatment of multilevel cervical fusion with cages. Surg Neurol. 2004. 62(5):378–385.

6. Cho DY, Liau WR, Lee WY, Liu JT, Chiu CL, Sheu PC. Preliminary experience using a polyetheretherketone (PEEK) cage in the treatment of cervical disc disease. Neurosurgery. 2002. 51(6):1343–1349.

7. Gercek E, Arlet V, Delisle J, Marchesi D. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J. 2003. 12(5):513–516.

8. Kulkarni AG, Hee HT, Wong HK. Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J. 2007. 7(2):205–209.

9. Lee SH, Suk KS, Kim KT, Lee JH, Seo EM, Im YS. Outcome analysis of single level anterior cervical fusion using interbody PEEK cage with autologous iliac bone graft. J Korean Orthop Assoc. 2009. 44(1):93–101.

10. Mastronardi L, Ducati A, Ferrante L. Anterior cervical fusion with polyetheretherketone (PEEK) cages in the treatment of degenerative disc disease: preliminary observations in 36 consecutive cases with a minimum 12-month follow-up. Acta Neurochir (Wien). 2006. 148(3):307–312.

11. Meier U, Kemmesies D. Experiences with six different intervertebral disc spacers for spondylodesis of the cervical spine. Orthopade. 2004. 33(11):1290–1299.
12. Kim KT, Suk KS, Kim JM. Future development of interbody fusion cages. J Korean Soc Spine Surg. 2001. 8(3):386–391.

13. Song KJ, Lee KB. A preliminary study of the use of cage and plating for single-segment fusion in degenerative cervical spine disease. J Clin Neurosci. 2006. 13(2):181–187.

14. Emery SE, Fisher JR, Bohlman HH. Three-level anterior cervical discectomy and fusion: radiographic and clinical results. Spine (Phila Pa 1976). 1997. 22(22):2622–2624.
15. Barsa P, Suchomel P. Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J. 2007. 16(9):1395–1400.

16. Schmieder K, Wolzik-Grossmann M, Pechlivanis I, Engelhardt M, Scholz M, Harders A. Subsidence of the wing titanium cage after anterior cervical interbody fusion: 2-year follow-up study. J Neurosurg Spine. 2006. 4(6):447–453.

17. Robinson RA, Smith GW. Anterolateral cervical disk removal and interbody fusion for cervical disk syndrome. Bull Johns Hopkins Hosp. 1955. 96(5):223–224.
18. Kandziora F, Pflugmacher R, Scholz M, et al. Treatment of traumatic cervical spine instability with interbody fusion cages: a prospective controlled study with a 2-year follow-up. Injury. 2005. 36:Suppl 2. B27–B35.

19. Koller H, Hempfing A, Ferraris L, Maier O, Hitzl W, Metz-Stavenhagen P. 4- and 5-level anterior fusions of the cervical spine: review of literature and clinical results. Eur Spine J. 2007. 16(12):2055–2071.

20. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am. 1999. 81(4):519–528.

21. Farey ID, McAfee PC, Davis RF, Long DM. Pseudarthrosis of the cervical spine after anterior arthrodesis. Treatment by posterior nerve-root decompression, stabilization, and arthrodesis. J Bone Joint Surg Am. 1990. 72(8):1171–1177.

22. Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. J Bone Joint Surg Am. 1993. 75(9):1298–1307.

23. Bohler J, Gaudernak T. Anterior plate stabilization for fracture-dislocation of the lower cervical spine. J Trauma. 1980. 20(3):203–205.
24. Emery SE, Bolesta MJ, Banks MA, Jones PK. Robinson anterior cervical fusion comparison of the standard and modified techniques. Spine (Phila Pa 1976). 1994. 19(6):660–663.
25. Papadopoulos EC, Huang RC, Girardi FP, Synnott K, Cammisa FP Jr. Three-level anterior cervical discectomy and fusion with plate fixation: radiographic and clinical results. Spine (Phila Pa 1976). 2006. 31(8):897–902.
26. Wang JC, McDonough PW, Kanim LE, Endow KK, Delamarter RB. Increased fusion rates with cervical plating for three-level anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2001. 26(6):643–646.

27. Hwang SL, Lee KS, Su YF, et al. Anterior corpectomy with iliac bone fusion or discectomy with interbody titanium cage fusion for multilevel cervical degenerated disc disease. J Spinal Disord Tech. 2007. 20(8):565–570.

28. Natarajan RN, Chen BH, An HS, Andersson GB. Anterior cervical fusion: a finite element model study on motion segment stability including the effect of osteoporosis. Spine (Phila Pa 1976). 2000. 25(8):955–961.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download