Abstract
Background
To evaluate the radiological, clinical results in patients with open distal tibia factures, who were treated with a staged treatment protocol using the lateral minimally invasive plate osteosynthesis (MIPO) technique.
Methods
From January 2007 to June 2009, 10 patients with open distal tibia fractures (Gustilo-Anderson classification II, 3; IIIA, 1; IIIB, 6) were treated using a staged treatment protocol. The initial debridement and application of an external fixator were performed within 24 hours and the mean interval from injury to definitive surgical treatment was 15 days (range, 6 to 52 days). Eight weeks later, an additional bone graft was performed in 3 patients. The follow-up duration was more than 1 year.
Results
The mean fracture healing time was 21 weeks (range, 17 to 28 weeks), and the average Iowa ankle rating score was 84.5 points. At the last follow-up, there was no non-union, angular deformity > 5°, shortening > 10 mm or infection. In 10 patients, 2 patients had a superficial wound infection, and another 2 patients showed limitation of ankle joint motion.
Open distal tibia fractures are caused mainly by a high-energy injury. The traditional treatment for such fractures, lateral plate fixation after an open reduction, may be associated with many complications, such as skin/soft tissue necrosis, core infection, osteomyelitis and amputation.1-5)
Recent studies have reported tissue necrosis is minimized, and satisfactory bony union is achieved, with the use of a staged protocol, with application of a temporizing ankle-spanning external fixator and minimally invasive plate osteosynthesis (MIPO); this protocol is also suggested to reduce the incidence rate of complications associated with traditional treatment.3-7) When there is extensive soft tissue injury on the medial side of the tibia or open wound, it is quite difficult to process a medial MIPO in many cases, and complications, such as skin necrosis and plate exposure, could be encountered.7-11)
The authors have developed a staged protocol for treating high-energy open distal tibia fracture patients: involving wound lavage, debridement, vaccum-assisted closure (VAC) and external fixation within 24 hours after hospitalization followed by a skin graft and flap surgery for soft tissue coverage. In patients with a severe metaphyseal bone defect, 8 weeks of staged bone grafting was performed after lateral MIPO. This study evaluated the staged treatment protocol using the lateral MIPO technique in patients with an open distal tibia fracture, and analyzed the treatment results.
From January 2007 to June 2009, 10 patients with an open distal tibia fracture were treated using a staged protocol, and followed up for at least one year. The mean age was 52.4 years (aged 29 to 82) and there were six men and four women. The average follow-up period was 14.8 months (range, 12 to 23 months) and the causes of the injuries were as follows: nine cases from traffic accidents (five pedestrians, two drivers, and two motorcyclists) and the other case was a fall (25 m). In accordance with the Gustilo-Anderson classification, three cases were classified as II, one case as IIIA, and six cases as IIIB. According to the AO/OTA classification, two cases were classified as A2 and eight cases as A3. The treatment involved two or three stages, according to the skin/soft tissue condition and size of the bone defect (Table 1).
The staged treatment included thorough wound lavage, debridement, delayed lateral MIPO and an additional bone graft (in cases with a severe bone defect).
At the initial stage of treatment (stage 1), all dead soft and bone tissues were removed by definitive wound lavage and debridement, temporizing ankle-spanning external fixator intervention was performed, and a VAC device was used within 24 hours. As an external fixator (Artfix, Taeyeon Medical, Incheon, Korea), either a mono frame (six cases) or a delta frame (four cases) was used (Fig. 1). In the treatment of skin and soft tissue, delayed primary closure was performed in four cases and a VAC device (VAC ATS therapy system, Kinetic Concepts Inc., San Antonio, TX, USA) was used in six cases (in patients in whom a delayed primary suture could not be performed). Lateral malleolar fracture was accompanied in seven cases; of these, intramedullary nailing using a rush pin was performed in three cases with severe lateral soft tissue injury, and open reduction and internal fixation were performed in the other four cases (Table 2).
After the stage 1 treatment and a delay for a mean period of 15 days (range, 6 to 52 days), when the status of soft tissue was properly stabilized enough for soft tissue reconstruction, with no sign of infection, definitive surgical treatment was performed. The patient was placed under general or spinal anesthesia in the supine position, where radiation fluoroscopy could be performed, and an indirect taxis of the fracture was performed by manual traction under the support of C-arm fluoroscopy. After obtaining alignment of the metaphysis of the distal tibia, by a closed reduction through traction, using an anterolateral approach, a 2-3 cm incision was made, starting at the level of the tibial plapond, and extending proximally along the anterolateral surface of the distal tibia, and a 3-4 cm proximal skin incision was made for screw fixation. A subcutaneous tunnel was created, along the anterolateral aspect of the tibia, by blunt dissection using a large Kelly clamp, and then a plate was inserted, without periosteal stripping and exposing the tibia, between the extensor hallucis longus tendon and the tibialis anterior tendon, or the extensor hallucis long tendon and the extensor digitorum longus tendon (Fig. 2).
When the plate was inserted, it was pushed percutaneously from the distal to proximal tibia, and after checking the reduction status, the distal tibia was fixed with a cancellous screw, and the proximal tibia was fixed with a cortical screw. The relevance of the fracture reduction status and plate location was rechecked. In all cases, a plate (periarticular lateral distal tibial plate; Zimmer, Cowpens, SC, USA) was used, and more than three screws were fixed in the distal and proximal tibias of the fracture with maximum stability, and then a joint spanning external fixator was removed. A split-skin graft was only performed in four out of six cases, in patients whom delayed primary closure was not possible during lateral MIPO; an anterolateral thigh free flap and split-skin graft were performed in the remaining two cases. Plating and soft tissue reconstruction was performed at the same time in all patients (Fig. 3).
At stage 3 after plate fixation, a bone graft was performed after lateral MIPO, to obtain bone union, in three cases with a severe metaphyseal bone defect and after lack of progression of healing for > 8 weeks in the distal tibia. Autogenous iliac bone and Demineralized Bone Matrix (Grafton DBM Putty: 5 mL, Ostothch Inc., Eatontown, NJ, USA) were used in one of these three cases, and autogenous iliac bone was used in the other two cases (Fig. 4).
Postoperatively, a posterior splint was applied to the ankle joint in the neutral position for 2 days. Three days after surgery, we allowed a full range of movement of ankle joint. In patients who underwent treatment using a long-term joint spanning external fixator, continuous and adequate ROM exercises were performed. The majority of patients were encouraged to partially bear their weight, 5-7 weeks after operation. Patients were allowed to fully bear their weight when there was radiological evidence of bone union and no pain associated with the fracture site.
The union time and complications (such as nonunioin or malunion) were investigated throughout the follow-up, using the periodic radiographs. Bone union was defined as when callus maturation was closed over 3/4 of the fracture faces, according to the anteroposteior and lateral radiographs, and the fracture site showed movement or tenderness, clinically. In addition, an angular deformity was defined as angulation, when there was > 5° angulation. Shortening was defined as > 10 mm shortening compared to the unaffected side. Each angulation was evaluated using the method reported by Milner.12)
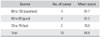
Ankle joint function was evaluated by a physical examination and survey, using the Iowa ankle rating system,13) at the last follow-up (Table 3). Four classified categories were investigated: function of the ankle joint, freedom of pain, gait and range of motion. Of a possible total score of 100; 90-100 was considered excellent, 80-89 was good, and 70-79 was considered fair. This study also examined the presence of complications, such as of skin/soft tissue necrosis and infection, reduction loss, osteomyelitis, irritative symptoms of the plate, and neuro-vascular injury during surgery.
In all cases, radiological evidence of bony union was obtained, and the average bony union time was 21 weeks (range, 16 to 28 weeks). Seven cases successfully obtained bony union after stage 2 surgery; an additional bone graft was required for three cases with a severe metaphyseal bone defect. There were no signs of angular deformity of the tibia over 5°; the average varus/valgus angulation was 2° (0-4°) / 1.7° (0-4°) and the average anterior/posterior angulation was 2.5° / 1.8° (0-4°). There were no signs of shortening of the tibia > 10 mm; the average was 3.5 mm (range, 0 to 8 mm).
The ankle joint function was evaluated during the final follow-up, and the mean was 84.4 points; four cases were excellent, four cases were good, and the other two cases were fair. Eight out of ten cases showed satisfactory results. In the two fair cases, one was accompanied with a foot fracture, and the other with a flap due to a severe open fracture. Two cases had a superficial wound infection during the treatment period and the other two cases had a mild limitation in movement of the ankle joint. The superficial wound infections were treated with antibiotics, localized wound lavage and debridement. There were no signs of other complications; such as nonunion, malunion, deep infection, osteomyelitis, breakage of the clamp screw or plate, or neuro-vascular injury (Table 4).
Because open distal tibia fractures are often caused by high-energy damage, extensive soft tissue injury and severe communition of the fracture site are usually observed. Moreover, in many cases, functional disability remains after treatment when the fracture is quite close to the ankle joint; in particular, the medial part of the distal tibia, where is little subcutaneous soft tissue, close to the periosteum. An open wound and extensive soft tissue injury is usually found on the medial side in an open distal tibia fracture; which usually precludes primary skin, and soft tissue, covering. Therefore, in the treatment of fractures, both the stability of the soft tissue covering, and anatomical reduction in the articular surface, need to be obtained. Therefore, there are many difficulties associated with treatment, which are often followed by a staged treatment.5,14-16)
In the previous method using an external fixator, conventional open reduction, and plate fixation, many cases were reported to have developed complications; such as skin/soft tissue infections, and nonunion or delayed bony union, due to microvascular damage by periosteal stripping.16-20) In addition, Borelli et al.21) discovered an extraosseous blood supply that branches around the anterior and posterior tibia, and reported severe damage in blood flow when conducting a conventional open reduction and plate fixation.
A staged protocol using MIPO, showed good clinical results, with good maintenance of blood flow and hematoma around the fracture site, and soft tissue damage was minimized by biological fixation, using a bridge plate around the anteromedial part of the tibia.5,6,22-25)
Yang et al.5) reported satisfactory bony union, on average, on the 19th week; after having conducted a staged protocol, using MIPO, on open distal tibia fracture patients. Collinge et al.3) and Borens et al.7) also reported good results after using a staged protocol, using MIPO, in open distal tibia fracture patients. Therefore, staged treatment, using MIPO, has been shown to be one of the most effective ways of treating open distal tibia patients.
However, the subcutaneous soft tissue on the medial side of the distal tibia is thin, and it is close to periosteal bone, because of this, it is likely that skin irritative symptoms would be observed during medial plating and plate removal might be needed in severe cases. In particular, medial MIPO cannot be performed, when performing on an open distal tibia fracture, where there is extensive soft tissue injury and an open wound on the medial side. Furthermore, complications, such as skin necrosis and plate exposure, can occur even when a medial plate is inserted.8,11,24,26,27)
The authors established a staged protocol for when medial MIPO is made difficult to perform by extensive soft tissue damage on the medial side in open distal tibia fracture patients. At stage 1, the initiation approach treatment, close wound lavage, debridement and the application of an ankle spanning bridging the external fixtor, was carried out within 24 hours after hospitalization. A VAC device was used for the six cases in which a primary suture for an open wound was not possible. In stage 2, lateral MIPO was conducted, after a mean delay of 15 days (range, 6 to 52 days), when the status of soft tissue was properly stabilized, with no signs of infection. In stage 3, a bone graft was performed on three cases with a severe metaphyseal bone defect. All cases achieved bony union within an average period of 21 weeks, and subjective satisfaction was good in eight cases.
The use of a bridging external fixator, in open distal tibia fracture patients, stimulated the recovery of soft tissue around the fracture site, and maintained the length and alignment of the tibia before plate fixation.27-29) Furthermore, use of a VAC device, when treating an open distal tibia fracture, stimulated the recovery of soft tissue, reduced the incidence rate of associated complications and the chance of requiring flap surgery.30)
In the stage 2 treatment, avoiding the fracture site during lateral plate fixation, the fracture was fixed with a bridge plate, on the lateral side of the distal tibia, through an indirect reduction, with a minimal incision of the anterolateral side, and the time to definitive surgery with lateral MIPO was reduced. Two types of incision methods were used: between the extensor hallucis longus tendon and tibialis anterior tendon, and between the extensor hallucis longus tendon and extensor digitorum longus tendon. When using the former, the bone was checked directly, without observing the neuro-vascular structures, to fix the fracture site after setting aside the neuro-vascular structures with the proper strength. In the latter, the soft tissues were detached carefully, and the neuro-vascular structure was checked and fixed. In all 10 cases, the fracture site was fixed without any complications related neurovascular injury.
Satisfactory bony union was achieved, without nonunion or delayed union, after conducting a staged bone graft, in three cases with a severe bone defect, during the stage 3 treatment. A bone graft was carried out when there was a severe bone defect during the eighth week after plate fixation. Gardner et al.14) reported that satisfactory bony union could be obtained, after a staged bone graft, in distal tibia fracture patients with severe bone defects.
After the final treatment, two cases exhibited limited ankle joint motion; one case had to have a long-term external fixation, and limited joint motion, due to extensive soft tissue injury, the other case was accompanied with a fracture around the foot. All other cases recovered, within normal, range of motion. During the treatment period, two cases had a superficial wound infection; infections were treated with antibiotics, and local treatments, without specific problems.
The complications related to soft tissue injury were minimized using the staged protocol with lateral MIPO. Futhermore, blood flow supplement was maintained in the fracture site because there was no periosteal stripping. Satisfactory clinical results and bony union were obtained without delayed union or nonunion. However, it is difficult to compare the results with the literature directly as many authors utilized different treatment methods and group compositions, and the overall group size used in the current study was small. Therefore, another study with a larger cohort will be needed.
Complications, such as soft tissue necrosis and infection, were minimized, using primary wound lavage, debridement, MIPO with a lateral plate fixation technique, and a staged protocol of bone grafts. Appropriate fixation was obtained using indirect taxis, and biological fixation by preserving the blood flow around the fracture site. With the exception of two cases with a mild limitation of motion, all cases showed satisfactory bony union with no complications, such as skin irritative symptoms and nonunion. This staged protocol, using lateral MIPO, is believed to be one of the most effective ways of treating open distal tibia fractures with extensive soft tissue injury.
Figures and Tables
Fig. 3
(A) A 65-year-old woman sustained a right open distal tibia fracture (AO/OTA type A2, Gustilo-Anderson classification IIIB). (B) Stage 1, irrigation & debridement was performed and ankle-spanning bridge external fixator was applied. (C) Stage 2, after 6 weeks, lateral plate fixation of the distal tibia using the minimally invasive plate osteosynthesis (MIPO) technique was performed and anterolateral. rotator free flap and skin graft were applied. (D) The last follow-up, 13 months postoperatively. AO/OTA: AO/Orthopaedic Trauma Association.

Fig. 4
(A) A 29-year-old woman sustained a right open distal tibia fracture (AO/OTA type A3, Gustilo-Anderson classification IIIB). (B) Stage 1, irrigation & debridement was performed and ankle-spanning bridge external fixator was applied. (C) Stage 2, after 8 weeks, lateral plate fixation of the distal tibia using the minimally invasive plate osteosynthesis (MIPO) technique was performed and a skin graft was applied. (D) Stage 3, 8 weeks after open reduction and internal fixation, a bone graft was performed using autogenous iliac bone. (E) Last follow-up, 21 months postoperatively. AO/OTA: AO/Orthopaedic Trauma Association.

References
1. Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma. 1999. 13(2):92–97.

2. Borg T, Larsson S, Lindsjo U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury. 2004. 35(6):608–614.
3. Collinge C, Kuper M, Larson K, Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma. 2007. 21(6):355–361.

4. Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 2004. 18:8 Suppl. S32–S38.

5. Yang JH, Kweon SH, Kim JW, Park JY, Kim HJ, Lim CM. Two-staged delayed minimally invasive percutaneous plate osteosynthesis for distal tibial open fractures. J Korean Fract Soc. 2008. 21(1):24–30.

6. Chang SA, Ahn HS, Byun YS, Kim JH, Bang HH, Kyun DY. Minimally invasive plate osteosynthesis in unstable fractures of the distal tibia. J Korean Fract Soc. 2005. 18(2):155–159.

7. Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet DL. Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases. Arch Orthop Trauma Surg. 2009. 129(5):649–659.

8. Helfet DL, Suk M. Minimally invasive percutaneous plate osteosynthesis of fractures of the distal tibia. Instr Course Lect. 2004. 53:471–475.
9. Lee YS, Chen SH, Lin JC, Chen YO, Huang CR, Cheng CY. Surgical treatment of distal tibia fractures: a comparison of medial and lateral plating. Orthopedics. 2009. 32(3):163.
10. Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004. 28(3):159–162.

11. Hong KD, Ha SS, Chung NS, Sim JC, Ahn SC. Lateral plate fixation of distal tibial metaphyseal fracture using minimally invasive plate osteosynthesis technique. J Korean Fract Soc. 2006. 19(1):24–28.

12. Milner SA. A more accurate method of measurement of angulation after fractures of the tibia. J Bone Joint Surg Br. 1997. 79(6):972–974.

13. Merchant TC, Dietz FR. Long-term follow-up after fractures of the tibial and fibular shafts. J Bone Joint Surg Am. 1989. 71(4):599–606.

14. Gardner MJ, Mehta S, Barei DP, Nork SE. Treatment protocol for open AO/OTA type C3 pilon fractures with segmental bone loss. J Orthop Trauma. 2008. 22(7):451–457.

15. Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007. 38(3):365–370.

16. Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures. Variables contributing to poor results and complications. Clin Orthop Relat Res. 1993. (292):108–117.
17. Holbrook JL, Swiontkowski MF, Sanders R. Treatment of open fractures of the tibial shaft: Ender nailing versus external fixation. A randomized, prospective comparison. J Bone Joint Surg Am. 1989. 71(8):1231–1238.
18. Manninen MJ, Lindahl J, Kankare J, Hirvensalo E. Lateral approach for fixation of the fractures of the distal tibia: outcome of 20 patients. Technical note. Arch Orthop Trauma Surg. 2007. 127(5):349–353.

19. Shepherd LE, Costigan WM, Gardocki RJ, Ghiassi AD, Patzakis MJ, Stevanovic MV. Local or free muscle flaps and unreamed interlocked nails for open tibial fractures. Clin Orthop Relat Res. 1998. (350):90–96.

20. Wolinsky P, Lee M. The distal approach for anterolateral plate fixation of the tibia: an anatomic study. J Orthop Trauma. 2008. 22(6):404–407.

21. Borrelli J Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002. 16(10):691–695.

22. Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003. (408):286–291.

23. Pai V, Coulter G. Minimally invasive plate fixation of the tibia. Int Orthop. 2007. 31(4):491–496.

24. Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004. 35(6):615–620.

25. Salton HL, Rush S, Schuberth J. Tibial plafond fractures: limited incision reduction with percutaneous fixation. J Foot Ankle Surg. 2007. 46(4):261–269.

26. Krackhardt T, Dilger J, Flesch I, Hontzsch D, Eingartner C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005. 125(2):87–94.

27. Saleh M, Shanahan MD, Fern ED. Intra-articular fractures of the distal tibia: surgical management by limited internal fixation and articulated distraction. Injury. 1993. 24(1):37–40.

28. Marsh JL, Bonar S, Nepola JV, Decoster TA, Hurwitz SR. Use of an articulated external fixator for fractures of the tibial plafond. J Bone Joint Surg Am. 1995. 77(10):1498–1509.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download