This article has been
cited by other articles in ScienceCentral.
Abstract
Background
A second staged operation using temporary bridging external fixation (TBEF) has been widely used in patients with periarticular complex fracture, yet few papers have been published on the related complications. The purpose of this study was to report the complication rate and pitfalls directly related to TBEF through a retrospective study and to suggest some solutions.
Methods
Fifty-nine cases that were treated by using TBEF were studied among 195 periarticular complex fractures. We retrospectively collected the clinical and radiological data and then the study data was evaluated for 1) cases with unsatisfactory restoration of length, 2) cases with deep infection caused by half pins invading the zone of definitive fixation, and 3) neurovascular injuries related to half pins.
Results
Complications were observed in 7/59 cases (11%). Problems related to the achievement of length were observed in one case of distal tibia fracture and 2 cases of distal femur fracture. Half pin related infection was observed in 2 cases of distal femur fracture. Neurovascular injury (medial calcaneal nerve injury in a distal tibia fracture) was observed in 2 cases. Among 7 complications, four were related to using TBEF in distal femur fracture. This is because the abundant leg muscles have strong deforming force and infection might be increased due to frequent irritation by the half pins.
Conclusions
TBEF is a simple procedure with several advantages. However, complications might be observed if certain principles are not followed. It is thought that many complications due to TBEF can be reduced if the half pins are not inserted in the zone of injury, restoration of length is fully achieved and the neurovascular characteristics are carefully considered. In particular, much more caution is needed in the distal femur, which has abundant muscles surrounding it.
Keywords: Periarticular fractures, Bridging external fixator, Complication
There are various treatments for periarticular complex fracture and these range from minimally invasive external fixation with percutaneous pinning to invasive methods using open reduction and internal fixation. However, the most widely used treatment is presently a staged operation of open reduction and internal fixation with plating after settling down the soft tissues using a temporary bridging external fixator (TBEF).
A TBEF is the basis of a staged operation, and easy, fast and simple procedure with many advantages. TBEF provides relative stability to fractured areas while the soft tissues around the fractured area heal before performing formal open reduction and internal fixation. Such relative stability provides patients with mobility and thus this is considered as "portable traction."
1,
2) The mobility given to patients reduces the movement of the fractured areas and it subsequently reduces the pain and the following inflammatory reactions of neighboring tissues, and so it quickly helps soft tissue to heal. The nursing care also becomes easier. Early mobilization can reduce the cardiopulmonary complication in patients with periarticular complex fracture.
With these advantages, the staged operation using TBEF has been widely used and its excellent results have been reported, but there are few studies on the complication rate or pitfalls of using TBEF.
We performed a retrospective study on the patients with periarticular complex fracture (distal femur, proximal tibia, distal tibia) and who were treated with TBEF to determine the complication rate and the commonly related problems and also to suggest some solutions for these pitfalls.
METHODS
This study is not intended to report the results of staged operations, but rather, to discuss the problems observed during the definitive fixation after soft tissue healing around the fractured areas with the use of a TBEF, and the complications and problems that developed between the time of surgery and the first postoperative outpatient visit. The study was conducted on 59 cases for which definitive plating was performed with a TBEF as the initial treatment, among the 195 fractures (distal femur, 58 cases; proximal tibia, 85 cases; distal tibia, 52 cases) that were treated between January of 2003 and June of 2008.
According to the Orthopaedic Trauma Association (OTA) classification, distal femur fracture included 5 cases of C1, 4 cases of C2, and 9 cases of C3; distal tibia fracture included 2 cases of C1, 3 cases of C2, and 6 cases of C3. Proximal tibia fracture, according to Shazker's type, included 9 cases of type IV and 21 cases of type VI. The patients included 46 males and 13 females, and the average age was 48 years. The involved mechanism of injury was mostly high-energy injuries, with 35 cases of motor vehicle accidents, 16 cases of falls and 8 cases of industrial accidents. A total of 19 cases were open fractures, among which there were 2 cases of type I, 6 cases of type II, 4 cases of type IIIa and 5 cases of type IIIb. Two out of 19 cases were type IIIc fractures and both were proximal tibia Schazker type VI. Two cases of type IIIc were excluded due to the difficulties of determining the relationship between a half pin and infection. Among these 19 cases of open fracture, 9 cases were transferred from local private hospitals to our hospital after performing TBEF (3 distal femur fractures with 1 C2 and 2 C3, 4 proximal tibia fractures with 2 IV and 2 V and 2 distal tibia fractures with 1 C2 and 1 C3).
Surgical Technique
The technique of TBEF and staged treatment was applied in the cases with severe trauma to the soft tissue around the fractured area (severe swelling, ecchymosis or blistering). In cases of open fractures, debridement was performed separately from the TBEF procedure if possible. Soft tissue debridement and irrigation were performed and then a bead pouch was made.
Half pins were inserted, using the safe corridor technique, through the region with less neurovascular risk.
3) Half pin insertion was performed in a percutaneous fashion with the use of soft tissue sleeves, and pre-drilling was done to avoid thermal necrosis and soft tissue damage to the underlying bone. Half pins were inserted away from the intended site of prospective plating when converting to open reduction and internal fixation. When the patient was hemodynamically unstable, only damage control surgery was performed, and TBEF was applied by focusing on maintaining the length of the limb and fractured areas. When the patient was stable, efforts were made to provide 3-dimensional alignment of fractured areas if possible. Reduction was performed by using ligamentotaxis only, and no other procedures were performed on the fractured areas. All half pins were inserted with avoiding zones of fracture and soft tissue injury, and the prospective site of definitive surgery if possible.
The time period between TBEF and plating should be not more than 2 weeks, but there were cases with a time period of more than 2 weeks after TBEF such as for patients transferred from other hospitals, or wherever pin site infection was suspected, then the pin site debridement was performed later along with administration of antibiotics for 1 week, and then the surgery was performed.
The TBEF was kept in place until all the soft tissue envelopes stabilized, which usually took 7 to 10 days. When skin winkles and no pitting edema were observed, this was considered as an indication for converting to the definitive surgery. The TBEF was removed before the surgery depending on the alignment of the fractured area, and if the alignment was satisfactory, then the site was disinfected with 95% isopropyl alcohol, iodine prep scrub and iodine spray, and the reduction was maintained or TBEF was used as a reduction device in the surgical field.
Knee Spanning Frames
Knee spanning frames were applied for complex, unstable distal femur and proximal tibia fractures. Half pins were inserted by considering the future intended location of plates in the definitive surgery. Two half pins were inserted in the anterior femur and 2 half pins were inserted in the anteromedial tibia. Various types of external fixator devices were used, and most of which were modular type external fixators. The advantages of this device include convenient 3-dimensional reduction that can be obtained by only using bars, which were connected to the half pins inserted to each fractured area. In such cases, double-stacked anterior bars were used to increase the stability of the fractured areas. Particularly in the case of the distal femur, it is better to maintain the alignment during the TBEF procedure because of the bulky muscles in the fractured area and the characteristic displacement after injury. When a patient was hemodynamically stable, correcting the length, external rotation and flexion deformity were attempted several times under fluoroscopic guidance. It is thought that maintenance of length is a very important factor. However, if the vascularity of a limb in question was suspicious, then overdistraction could be dangerous. Therefore, the circulation was always checked after distraction.
Ankle Spanning Frames
These frames were used in cases of pilon fractures with severely compromised soft tissues. Lateral fibular plating was not performed in the same surgery along with TBEF. In most cases, a modular external fixator was used. Two half pins were inserted in the proximal tibia and for the distal part, 1 half pin was inserted in the lateral calcaneus and the other one was inserted in the 1st metatarsal base. Bars and medial calcaneus pin were applied in good order to increase the frame stability. If possible, a medial pin was inserted last because of possible damage to the medial calcaneal branch.
4) Blunt dissection and sleeves were used prior to half pin insertion.
When a patient was hemodynamically stable, reduction was performed by ligamentotaxis under fluoroscopic guidance to preferentially obtain the lengthening of the fracture sites and to achieve ankle joint stability. This is because if the ankle joint has no stability, then soft tissue healing can be very slow. When the circulation was doubtful, overdistraction was avoided and the circulation was checked after the surgery.
Evaluation
The patients were evaluated clinically and radiologically for the following three possible TBEF related problems.
Cases with unsatisfactory achievement of length. Failure of lengthening was defined as cases in which any procedure such as the push technique was performed or a femoral distractor was used to obtain lengthening, but it did not achieve the desired length.
Cases with deep infection caused by half pins invading the zone of definitive fixation without considering the plating position for definitive fixation. Delayed deep infection that developed in the fracture zone without being invaded by half pins was excluded. Also, deep infection of fractured areas related to open fracture was excluded.
Neurovascular injuries observed after TBEF fixation.
RESULTS
TBEF related problems were observed in 7 out of 59 cases (11%). Among these 7 cases, failure to achieve length was observed in 3 cases, including 1 case in distal tibia fracture and 2 cases in distal femur fracture. Neurovascular injuries were observed in 2 out of 7 cases. Both cases were medial calcaneal nerve injury. Half pin site related deep infection was observed in 2 cases, and both were cases of distal femur. Four out of the 7 cases of complications were cases of distal femur fractures. Two of the the nine were transferred from another local private hospital.
The average time for definitive plating after TBEF was 15.3 days (range, 4 to 81 days). If the cases with deep infection were excluded, then the actual time was 11.3 days.
Table 1 summarizes the complications. Two cases among the cases with lengthening related problems were distal femur fractures. Achieving the lengthening in the management of distal femur fracture is easier than that for other deformities. When surgeons see just the AP image of C-arm fluoroscopy during the procedures, they make mistakes such as shortening because of flexion deformity of the distal femur.
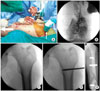
Fig. 1 showed a 45-year male patient who was transferred from a local private hospital after the application of initial TBEF for severe soft tissue compromise. Proximal half pins were involved not only in the zone of definitive surgery, but also in the zone of soft tissue injury. In addition, a distal femur articular fragment showed typical deformity such as internal rotation, flexion and shortening. Fortunately, no infection was observed in the proximal half pin site and the second surgery could be done at the 12th day after surgery without debridement of the pin site, and no specific infection was observed.
Neurovascular injury was observed in 2 out of 7 cases and both were medial calcaneal nerve injuries.
Fig. 2 showed a 40-year male patient who received TBEF for soft tissue swelling and blister formation after pilon fracture. The patient did complain about continuous paresthesia in the heel area.
All the TBEF related deep infections on the half pins sites developed in distal femur fractures. A 60-year patient who had a tibia open fracture, including a distal femur fracture, from a traffic accident was transferred from a local hospital after 4 weeks of treatment (
Fig. 3). Infection was found in the tibia, but this was controlled by performing radical debridement and muscle transfer, and proximal half pin was re-applied. after debridement. At that time of the initial debridement, there was no infection observed at the external fixator half pin site in the distal femur. Since the half pin had been placed for more than 2 weeks, pin site debridement was performed and the location of the half pins was changed from the lateral thigh to the anterior thigh. Intravenous antibiotics were injected for one week. However, infection developed at the original half pin site after converting to plating.
DISCUSSION
According to several studies, staged open reduction and internal fixation with the use of TBEF in complex periarticular fracture with compromised soft tissue (distal femur, proximal tibia and distal tibia) has greatly decreased the rate of infection.
5-
7) Pin site infection and hardware related infection have been continuously reported, but these reports are now much less frequent than earlier.
Most studies have not particularly emphasized infections that are directly related to TBEF. Sirkin et al.
7) have reported a 3% infection rate in closed fracture and a 10% rate in the open fracture among 56 cases of severe pilon fracture. However, TBEF with half pin site related infection was not especially mentioned. TBEF is a simple, convenient procedure with several advantages and it has been widely used, but there have been few reports on its problems and pitfalls.
We performed a retrospective study with emphasizing 3 problems that could be potentially damaging when using TBEF and we found that 7 out of 59 cases (11%) had those problems. These 3 problems are important because of the following reasons. First, there are some cases in which 1 cm of desired length could not be obtained during the definitive surgery if 2 weeks had already passed since the injury. In such cases, several procedures were tried in the surgical field to obtain lengthening and the operation time was extended, which is accompanied by an increased risk of infection. Second, the site of half pins should be carefully considered because it is directly related to infection. Third, the pain caused by neurovascular injury can worsen the results when evaluating complex periarticular fractures. Thus, it becomes difficult to evaluate if pain problems are due to a fracture itself or the increased pain from nerve damage.
Especially noticeable was that four among 7 complications were observed in distal femur fractures, and no particular problem was observed in the proximal tibia. Distal femur fracture can be considered as resistant to infection due to relatively abundant muscle envelope, but this infection problem is especially observed after TBEF application. Infection related to TBEF may occur because the deforming force is strong in the fractured area due to abundant muscles and the risk for infection in the area surrounding the pins is high due to irritation that develops after inserting half pins. Also, half pin insertion in the proximal side is often more difficult because the possibility for neurovascular injury becomes greater as the proximal anterior half pins are inserted in the more proximal region. Some investigators have avoided anterior half pins because this may injure the quadriceps mechanism. These investigators often inserted lateral half pins, but more cautions for infection is needed because inserting lateral half pins can directly involve the zone of definitive surgery compared to anterior fixation. In
figure 4, the proximal side of the fracture showed external rotation and the distal fragment appeared shortened and flexed (
Fig. 1A). One cm of shortening can be considered as insignificant, but if the patient is unstable such as the case of polytraumatized patients, a converting procedure might not be performed for a certain period of time after TBEF application. In such cases, it is very difficult to restore the length during the second surgery. Therefore, it is the best to correct several alignments at the same time if a patient is hemodynamically stable, but the ultimate goal should be the restoration of lengthening if a patient is hemodynamically unstable. In case of distal femur fracture, we first inserted 2 distal half pins in the anteromedial side of the proximal tibia to obtain good alignment and then traction was performed to restore the lengthening without muscle irritation. If half pins are inserted first in the proximal thigh, then sufficient lengthening can not be obtained because pins cause irritation to the muscle during the traction, and such continuous irritation can give rise to infection after the surgery. After that, one half pin is inserted in the proximal side and then internal rotation is performed to correct the external rotation. Finally, two half pins were inserted anteriorly in the proximal femur and then fixation was performed (
Fig. 4).
TBEF is a safe procedure if safe corridors are used for pin insertion and neurovascular damage is not caused on the other side of the cortex while pre-drilling before inserting the half pins. In 2 cases of pilon fracture, medial calcaneal nerve injury was noticed (the medial calcaneal branch was damaged). Some authors have reported that safe placements could be at the back of the half point of the line connecting the posteroinferior medial calcaneus and the inferior medial malleolus, and at the back of the one third point of the line connecting the posteroinferior medial calcaneus and the navicular tuberosity.
4,
8) However, they suggested that half pin insertion is safer when the pins are placed behind the heel, if possible, because of many anatomic variations. They also suggested using blunt dissection and sleeves. We used the similar technique, as seen in
Fig. 2, that the half pins were inserted at the posterior area near the heel and we used blunt dissection and sleeves, but two cases of medial calcaneal nerve damage developed. To solve this problem we do lateral calcaneal pin insertion and 1st metatarsal pin insertion primarily and if this is unable to provide sufficient stability, then more bars are added; if it is not stable enough, then pins are added to the medial side for further stability.
There was no TBEF related problem in the proximal tibia fractures. At the time of injury, this is a region that is easily damaged due to open fracture, but this region seems to have less problems for TBEF application, in which proximal half pins are easily inserted in the distal femur, because it is not a fixation zone and also the pins are relatively easily inserted in the distal part to the ankle area because the anteromedial side is skin on bone.
Although our results were obtained from a retrospective study and the number of total cases was small, this is the first study on the TBEF problems that most orthopedic surgeons easily fail to notice. Also, it is thought that a rate of complications over 10% can sufficiently affect the final results of complex periarticular fracture. Therefore, we feel this study on the application of TBEF will catch the attention of diligent and thoughtful surgeons.
In conclusion, TBEF is a basic procedure for the staged operation technique and this technique has recently been widely used. It is considered to be a relatively easy technique, but its importance has been less emphasized than definitive plating. However, special concerns are needed because the frequency of TBEF related complications is high in cases of distal femur fracture. Thus, better results will be obtained if TBEF is performed with giving full consideration to the fixation zone, the restoration of length and the neurovascular structures. Much caution is needed when performing TBEF and particularly for distal femur fractures.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download