Abstract
Background
Arthroscopic rotator cuff repair generally has a good clinical outcome but shoulder stiffness after surgery due to subacromial adhesion is one of the most common and clinically important complications. Sodium hyaluronate (HA) has been reported to be an anti-adhesive agent in a range of surgical procedures. However, there are few reports of the outcomes of arthroscopic rotator cuff repair of the shoulder. This study examined whether a subacromial injection of HA/carboxymethylated cellulose (CMC) affected the postoperative shoulder stiffness and healing of rotator cuff repair, as well as the safety of an injection.
Methods
Between January 2008 and May 2008, 80 consecutive patients with arthroscopic rotator cuff repair were enrolled. The patients were assigned randomly to the HA/CMC injection group (n = 40) or control group (n = 40). All patients were evaluated using the visual analog scale (VAS) for pain, passive range of motion at 2, 6 weeks, 3, 6, 12 months after surgery, and the functional scores at 6, 12 months postoperatively. Cuff healing was also evaluated using CT arthrography or ultrasonography at 6 or 12 months after surgery.
Results
The HA/CMC injection group showed faster recovery of forward flexion at 2 weeks postoperatively than the control group but the difference was not statistically significant (p = 0.09). There were no significant difference in pain VAS, internal rotation, external rotation and functional scores between two groups at each follow-up period. The functional scores improved 6 months after surgery in both groups but there were no differences between the two groups. The incidence of unhealed rotator cuff was similar in the two groups. There were no complications related to an injection of anti-adhesive agents including wound problems or infections.
Conclusions
A subacromial injection of an anti-adhesive agent after arthroscopic rotator cuff repair tended to produce faster recovery in forward flexion with no adverse effects on cuff healing. However, its anti-adhesive effects after rotator cuff repair should be considered carefully with further studies.
Arthroscopic rotator cuff repairs generally have good functional outcomes regardless of tendon healing.1,2) On the other hand, postoperative shoulder stiffness is one of the most common and clinically important complications because it can cause severe pain and limitation of motion, making it difficult to rehabilitate patients,3,4) and decrease the postoperative functional outcomes. Therefore, in addition to improving cuff healing, other efforts to minimize the subacromial adhesions are needed to reduce the shoulder stiffness after arthroscopic rotator cuff repair.
Sodium hyaluronate (HA) has been reported to be an anti-adhesive agent in tendon surgery5,6) and abdominal surgery for reducing adhesions and postoperative ileus, as well as in gynecologic surgery for minimizing infertility due to tubal adhesion.7,8) In animal models, HA gel9) or sheets10) can attenuate post-laminectomy scar formation in spine surgery. Several in vitro studies have reported the enhanced rotator cuff healing potential of HA.11,12) However, to the authors' knowledge, there are no reports on the anti-adhesive effect of HA after arthroscopic rotator cuff repair in vivo. Therefore, this study examined whether a subacromial injection of hyaluronate (HA/carboxymethylated cellulose [CMC]; Guardix-Sol®, 5 g, Hanmi Pharm. Co., Seoul, Korea) affects the postoperative shoulder stiffness and healing process after rotator cuff repair as well as the safety of an injection.
Between January 2008 and May 2008, consecutive 80 patients who underwent arthroscopic rotator cuff repair in authors' institution were enrolled this study. The inclusion criteria were patients with a partial or full-thickness rotator cuff tear who underwent arthroscopic cuff repair with subacromial decompression and acromioplasty. The exclusion criteria were patients with arthritic shoulder, revision of the cuff repair, irreparable cuff tear, open surgery, instability, isolated superior labrum anterior posterior (SLAP) lesion, infection, calcific tendinitis, rheumatoid arthritis, and/or reflex sympathetic dystrophy. The patients were assigned randomly to one of two groups. Randomization was performed using an automatic generated randomization list. the HA/CMC injection was performed by a senior author (JHO) in a blinded manner through the lateral subacromial portal (approximately 2 cm lateral to the acromion in line with the posterior aspect of the clavicle), which was used in arthroscopic surgery during the first dressing on the second day after arthroscopic rotator cuff repair, when normal saline used during arthroscopic surgery was almost drained out (injection group). HA/CMC was not injected in the control group after arthroscopic rotator cuff repair but the same rehabilitation protocol was conducted. Based on a previous study,13) in which the standard deviation of forward flexion at 3 months was 21°, it was determined that a sample size of 32 in each group would have 80% power to detect a 15° difference in forward flexion between two groups at an alpha level of 0.05 (two-tailed) using a Student's t-test. In this study, 40 patients in each group were recruited to allow for a possible 20% loss during the study period. All patients provided written informed consent and all protocols were approved by the Institutional Review Board at the authors' institution.
All arthroscopic procedures were performed by a single surgeon (JHO). After managing the glenohumeral joint pathology, subacromial bursectomy with acromioplasty was performed in all patients. Rotator cuff repair was conducted in single row or double row manner using bioabsorbable suture anchors (Bio-corkscrew: Arthrex, Naples, FL, or Spiralok: Mitek, Raynham, MA, USA). The immobilization period within the abduction brace was determined by the tear size measured at the time of operation, 4 weeks for small (< 1 cm), 5 weeks for medium (> 1 cm, < 3 cm) and 6 weeks for large (> 3 cm) to massive tears (> 5 cm).8) Passive range of motion (ROM) exercises were recommended immediately after surgery for small and medium sized tears but passive ROM exercises were restricted for 2 weeks for large to massive tears. Active ROM exercises were encouraged after weaning off the brace, and strengthening exercises were started 3 months after the operation. Normal sports activities were usually permitted after 6 months of surgery. Rehabilitation was referred to and supervised by the Department of Rehabilitation at the authors' institution.
All data (pre-operation, 2, 6 weeks, 3, 6, 12 months after operation) were collected prospectively by a clinical researcher who was blinded to the study. The injected HA/CMC would be effective for 2 weeks, and early postoperative adhesion might be prevented using HA/CMC in this most painful period. Other outcome measurement periods were chosen according to the rehabilitation protocol: 6 weeks for brace weaning, 3 months for starting strengthening exercise, 6 months for starting sports activity, and 12 months for an evaluation of the cuff integrity with an imaging study and functional score.13)
For a functional outcome evaluation, the visual analog scale (VAS) for pain and the passive ROM were determined at each check-up period. The pain VAS was scaled from 0 to 10; 10 being the worst pain. Passive ROM (abduction, external rotation at side, internal rotation at back) were measured using a goniometer with the scapula in a fixed position. Passive abduction was measured in degrees between the arm and thorax in the scapular plane, and the external rotation of the arm on the side was measured in degrees between the thorax and forearm with the arm in the adducted position and 90° flexion of the elbow. The internal rotation of the back was measured by the vertebral level reached, where the tip of the thumb reached the spine. For analysis, the vertebral level was numbered serially as follows: 12 for the 12th thoracic vertebra, 13 for the 1st lumbar vertebra, and 17 for the 5th lumbar vertebra. A constant score and American Shoulder and Elbow Surgeons (ASES) score were also evaluated at 6 and 12 months, postoperatively. For an evaluation of rotator cuff healing, repaired rotator cuff tendon was examined by ultrasonography (USG) or computed tomography arthrography (CTA) at 6 or 12 months after surgery.
All statistical analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). A Student's t-test was used to compare the pain VAS, ROM and functional scores between the two groups, and a paired t-test was used to compare them between two consecutive periods in each group. A chi-square test was used to examine the gender distribution and tear size. A p-value < 0.05 was considered significant.
The mean age of the injection group (n = 40) was 59.2 ± 8.1 years (range, 40 to 73 years), and 20 patients (50%) were male. The mean age of the control group (n = 40) was 60.2 ± 8.2 years (range, 42 to 74 years) with 19 patients (47.5%) being male. Five and seven patients in the injection and control group, respectively, had diabetes mellitus. There was no associated partial articular surface tendon avulsion (PASTA) lesions or anterior labral tears with a rotator cuff tear. There were 13 and 9 cases with a type 2 SLAP lesion in the injection and control group, respectively. There was one case of a type 7 SLAP lesion in the control group. Combined SLAP lesions were treated with rotator cuff repair by SLAP repair, biceps tenotomy or biceps tenodesis according to the patient's age, integrity of the biceps and activity level. There were no significant differences in gender, age, tear size, and arm dominance between the two groups. Table 1 lists the patients' demographics.
The pain VAS was similar in the two groups before surgery, and improved continuously in a similar manner throughout the follow-up period in both groups. Significant pain improvement was observed at two weeks postoperatively, and between postoperative 3 and 6 months in both groups (p < 0.05) (Fig. 1).
Forward flexion showed no difference at the preoperative period. The injection group (146.47 ± 17.26) showed a tendency for faster recovery than in the control group (137.65 ± 24.69°) at two weeks postoperatively but the difference was not statistically significant (p = 0.09) (Fig. 2). However, no differences were observed between two groups thereafter. The external rotation of the arm on the side (Fig. 3) and internal rotation of the back (Fig. 4) were similar in two groups at the preoperative evaluation and each follow-up period.
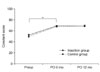
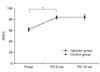
Further analysis was performed to determine if the ROM had improved between two consecutive periods (i.e., 2 to 6 weeks, 6 weeks to 3 months, 3 to 6 months, and 6 to 12 months). Significant improvement in forward flexion (Fig. 2), external rotation at the side (Fig. 3), and internal rotation of the back (Fig. 4) was observed in both groups between 6 weeks and 3 months (p < 0.05) except for an external rotation of the arm on the side in the injection group. However, these differences were not significant between two consecutive periods.
Significant improvement in the functional scores was observed after surgery (p < 0.001) in both groups, but there were no differences in the Constant score (68.4/67.9 at 6 months postoperatively, 68.0/69.3 at 12 months postoperatively) (Fig. 5) and ASES score (82.5/84.4 at 6 months postoperatively, 83.0/85.1 at 12 months postoperatively) (Fig. 6) between the two groups.
The incidence of unhealed rotator cuff tendon confirmed by USG or CTA was 20% (5/25) in the injection group and 26.9% (7/26) in the control group, and there was no significant difference between the two groups.
There were no acute complications related to an injection of anti-adhesive agents including wound problems or infections.
Sodium hyaluronate, which was used as an anti-adhesive agent after arthroscopic rotator cuff repair in this study, is a naturally occurring component of the extracellular matrix. The application of HA gel as antifibrotic material employs the concepts derived from "scarless" fetal wound-healing studies. In several animals, fetal incision healing occurs without scarring in the first two trimesters of pregnancy.14,15) High molecular weight HA is present in increased concentrations in the extracellular matrix of these animals along with low concentrations of hyaluronidase and low concentrations of tumor growth factor (TGF)-beta.16,17) These findings, at least in part, explain the scarless fetal wound healing. Several studies have reported HA gel9) or sheet10) to reduce postlaminectomy scar formation in animal model spinal surgery, which included the histology results. Akeson et al.10) reported progressive scar proliferation and maturation in an untreated postlaminectomy group in a rat laminectomy model. HA gel and 0.2 mm thick bioabsorbable macropore sheet reduced the level of postlaminectomy proliferative scarring without affecting the integrity of incisional wound healing.
The efficacy and safety of HA in abdominal and gynecologic surgery has been widely reported.7,8) Kumar et al.18) reported that a HA/CMC membrane was the only agent showing effectiveness as an anti-adhesiogenesis agent in general surgical patients. Several reports also have been published in orthopedic surgery. There are many reports showing a decrease in the number of peritendinous adhesions with seprafilm or hyaluronate gel after repair of the flexor tendons in animal models.19,20) The use of sodium hyaluronate as a non-surgical therapy in shoulder disorders has been reported.21,22) However, considering that shoulder stiffness is one of the important complications after surgical repair, it is surprising that there are a few reports of the anti-adhesive effects of hyaluronate after shoulder surgery, particularly after rotator cuff repair.
Shoulder stiffness is a common and important complication after arthroscopic rotator cuff repair.3,4,23) Although it was reported that pain and limitation of ROM caused by shoulder stiffness after rotator cuff repair improved steadily regardless of the integrity of the tendon,13,24) early postoperative shoulder stiffness can lead to uncomfortable pain and adverse effects as an obstacle to scheduled rehabilitation.
Huberty et al.4) reported 24 patients (4.9%) who developed postoperative stiffness out of 489 consecutive arthroscopic rotator cuff repairs, and treated these patients with arthroscopic capsular release. Therefore, preventing postoperative shoulder stiffness is an important issue after rotator cuff repair, and various efforts have been carried out.
There are several causative factors that contribute to shoulder stiffness after rotator cuff repair, and pre-existing pathology, surgical technique and inadequate rehabilitation are the three main factors.25) Considering these factors, this study was randomized one. Hence, the number of patients with a pre-existing SLAP lesion or adhesive capsulitis was similar. In addition, all procedures were conducted by one senior surgeon (JHO), and the postoperative rehabilitation was supervised by the Department of Rehabilitation. Therefore, the effects of confounding factors were reduced. Furthermore, subacromial adhesion and capsular contracture might affect the postoperative shoulder stiffness. However, it is believed that a subacromial adhesion may play a more important role in postoperative stiffness because many procedures were performed in the subacromial space (acromioplasty, bursectomy, cuff repair, etc.) thereby postoperative inflammation and subacromial fibrous adhesion can occur in the subacromial space. Accordingly, it is expected that a HA/CMC injection into subacromial space after arthroscopic rotator cuff repair would help to prevent postoperative subacromial adhesion and improve the ROM. However, these results show disappointing anti-adhesive effects of HA/CMC after rotator cuff surgery. Postoperative adhesion of the shoulder appears to be different from that of abdominal or gynecological surgery because shoulder stiffness and pain from adhesion can be relieved or prevented by vigorous ROM exercises. This suggests that ROM exercises can mask or dilute the anti-adhesive action of hyaluronate in rotator cuff surgery, and might show similar clinical results to the control group. Early passive ROM other than HA/CMC after cuff repair might reduce the level of postoperative subacromial adhesion and stiffness but the possible higher unhealing rate of rotator cuff might be another complication of early motion. Limited subacromial decompression including routine acromioplasty might help reduce the level of postoperative subacromial adhesion but the procedure will need to be performed in a certain group of patients. It was expected that hyaluronate would be effective in preventing postoperative adhesion in the subacromial space and improve postoperative functions including pain, ROMs, and functional scores but the results suggested otherwise.
There are several reports that hyaluronate may stimulate wound healing in several ways. During the early inflammatory phase of wound healing, a high concentration of hyaluronate in the wound matrix leads to increased infiltration and proliferation of cells in this area.26,27) Immunohistochemical staining of CD45 showed that the cells invading the repair site were mainly non-leukocyte cells, most likely fibroblasts.28) These fibroblasts produce new collagen fibers that eventually bridge the repair and restore tendon breaking strength.29) However, these results did not demonstrate the enhancing effects of hyaluronate for cuff healing. The non-healing rate of rotator cuff was similar in the two groups, even though there were insufficient follow-up imaging studies. Further study will be needed to examine the wound healing effect of hyaluronate.
There were several limitations in this study. First, the follow-up period was too short to fully support this data. Therefore, a further long-term study will be needed. Second, postoperative images could only be obtained in approximately 50% of patients, which might hamper the statistical power regarding cuff healing after surgery. Finally, all patients in both groups underwent early passive motion after surgery and there was no other control group with restricted passive motion while wearing brace. Therefore, it was not possible to determine if hyaluronate is more effective than restricted motion after rotator cuff repair.
In conclusion, although a subacromial injection of sodium hyaluronate to prevent subacromial adhesion after arthroscopic rotator cuff repair showed a tendency for faster improvement in forward flexion at 2 weeks postoperatively (p = 0.09) with no adverse effects on cuff healing, its anti-adhesive effect after rotator cuff repair should be considered carefully in future studies because all parameters were similar to the control group 12 weeks after surgery.
Figures and Tables
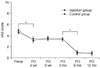 | Fig. 1Preoperative pain visual analog scale (VAS) was not different between two groups and improved continuously throughout follow-up period. Significant pain improvement was found at two weeks postoperatively, and between postoperative (PO) 3 and 6 months in both groups. Range bars show the standard errors. *p < 0.05. |
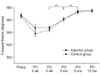 | Fig. 2Forward flexion (FF) showed no difference at preoperative period, but faster recovery was demonstrated in injection group (146.47° ± 17.26°) than in control group (137.65° ± 24.69°) at two weeks postoperatively (*p = 0.09). Significant improvement of FF within groups was found between postoperative (PO) 6 weeks and 3 months, and postoperative 3 months and 6 months in both groups (**p < 0.05). |
 | Fig. 3External rotation (ER) at side showed no significant statistical difference between two groups at serial follow-ups. Significant improvement of ER within groups was found between postoperative (PO) 6 weeks and 3 months (*p < 0.05) and postoperative 3 months and 6 months in control groups (**p < 0.05). |
 | Fig. 4Internal rotation at back showed no significant statistical difference between two groups at serial follow-ups. Significant improvement of internal rotation (IR) within groups was found between postoperative (PO) 6 weeks and 3 months and postoperative 3 months and 6 months in both groups (*p < 0.05). 5: level of 5th thoracic vertebra, 13: level of 1st lumbar vertebrae, 17: level of 5th lumbar vertebrae, 18: any level below the sacral vertebrae. |
 | Fig. 5Constant score demonstrated no statistical difference between two groups at serial follow-ups. Significant improvement of constant score within groups was found between preoperative check and postoperative (PO) 6 months in both groups (*p < 0.05). |
ACKNOWLEDGEMENTS
The authors gratefully acknowledge the assistance of Hye Ran Kim and Shang Mi Shim for collecting the data.
References
1. Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004. 86(2):219–224.

2. Nho SJ, Adler RS, Tomlinson DP, et al. Arthroscopic rotator cuff repair: prospective evaluation with sequential ultrasonography. Am J Sports Med. 2009. 37(10):1938–1945.
3. Brislin KJ, Field LD, Savoie FH 3rd. Complications after arthroscopic rotator cuff repair. Arthroscopy. 2007. 23(2):124–128.

4. Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009. 25(8):880–890.

5. Hagberg L, Gerdin B. Sodium hyaluronate as an adjunct in adhesion prevention after flexor tendon surgery in rabbits. J Hand Surg Am. 1992. 17(5):935–941.

6. Tuncay I, Ozbek H, Atik B, Ozen S, Akpinar F. Effects of hyaluronic acid on postoperative adhesion of tendo calcaneus surgery: an experimental study in rats. J Foot Ankle Surg. 2002. 41(2):104–108.

7. Fujii S, Shimada H, Ike H, et al. Reduction of postoperative abdominal adhesion and ileus by a bioresorbable membrane. Hepatogastroenterology. 2009. 56(91-92):725–728.
8. Mais V, Bracco GL, Litta P, Gargiulo T, Melis GB. Reduction of postoperative adhesions with an auto-crosslinked hyaluronan gel in gynaecological laparoscopic surgery: a blinded, controlled, randomized, multicentre study. Hum Reprod. 2006. 21(5):1248–1254.

9. Kato T, Haro H, Komori H, Shinomiya K. Evaluation of hyaluronic acid sheet for the prevention of postlaminectomy adhesions. Spine J. 2005. 5(5):479–488.

10. Akeson WH, Massie JB, Huang B, et al. Topical high-molecular-weight hyaluronan and a roofing barrier sheet equally inhibit postlaminectomy fibrosis. Spine J. 2005. 5(2):180–190.

11. Shimpuku E, Hamada K, Handa A, et al. Molecular effects of sodium hyaluronate on the healing of avian supracoracoid tendon tear: according to in situ hybridization and real-time polymerase chain reaction. J Orthop Res. 2007. 25(2):173–184.

12. Yamada T, Gotoh M, Nakama K, Mitsui Y, Higuchi F, Nagata K. Effects of hyaluronan on cell proliferation and mRNA expression of procollagens alpha 1 (I) and alpha 1 (III) in tendon-derived fibroblasts from patients with rotator cuff disease: an in vitro study. Am J Sports Med. 2007. 35(11):1870–1876.

13. Oh JH, Kim SH, Lee HK, Jo KH, Bin SW, Gong HS. Moderate preoperative shoulder stiffness does not alter the clinical outcome of rotator cuff repair with arthroscopic release and manipulation. Arthroscopy. 2008. 24(9):983–991.

14. Iocono JA, Ehrlich HP, Keefer KA, Krummel TM. Hyaluronan induces scarless repair in mouse limb organ culture. J Pediatr Surg. 1998. 33(4):564–567.

15. Stern M, Longaker MT, Stern R. Adzick NS, Longaker MT, editors. Hyaluronic acid and its modulation in fetal and adult wound healing. Fetal wound healing. 1991. New York: Elsevier;189–198.
16. Ferguson MW. Skin wound healing: transforming growth factor beta antagonists decrease scarring and improve quality. J Interferon Res. 1994. 14(5):303–304.

17. Shah M, Whitby DJ, Ferguson MW. Jackson IT, Sommerlad BC, editors. Fetal wound healing and scarless surgery. Recent advances in plastic surgery. 1996. Edinburgh: Churchill Livingstone.
18. Kumar S, Wong PF, Leaper DJ. Intra-peritoneal prophylactic agents for preventing adhesions and adhesive intestinal obstruction after non-gynaecological abdominal surgery. Cochrane Database Syst Rev. 2009. (1):CD005080.

19. Liu Y, Skardal A, Shu XZ, Prestwich GD. Prevention of peritendinous adhesions using a hyaluronan-derived hydrogel film following partial-thickness flexor tendon injury. J Orthop Res. 2008. 26(4):562–569.

20. Menderes A, Mola F, Tayfur V, Vayvada H, Barutcu A. Prevention of peritendinous adhesions following flexor tendon injury with seprafilm. Ann Plast Surg. 2004. 53(6):560–564.

21. Shibata Y, Midorikawa K, Emoto G, Naito M. Clinical evaluation of sodium hyaluronate for the treatment of patients with rotator cuff tear. J Shoulder Elbow Surg. 2001. 10(3):209–216.

22. Moskowitz RW, Blaine TA. An overview of treatment options for persistent shoulder pain. Am J Orthop (Belle Mead NJ). 2005. 34:12 Suppl. 10–15.
23. Boileau P, Brassart N, Watkinson DJ, Carles M, Hatzidakis AM, Krishnan SG. Arthroscopic repair of full-thickness tears of the supraspinatus: does the tendon really heal? J Bone Joint Surg Am. 2005. 87(6):1229–1240.

24. Trenerry K, Walton JR, Murrell GA. Prevention of shoulder stiffness after rotator cuff repair. Clin Orthop Relat Res. 2005. (430):94–99.

25. Rockwood CA Jr, Matsen FA 3rd, Wirth MA, Lippitt SB, Fehringer EV, Sperling JW. The shoulder. 2009. 4th ed. Philadelphia: Saunders;899–902.
26. Brecht M, Mayer U, Schlosser E, Prehm P. Increased hyaluronate synthesis is required for fibroblast detachment and mitosis. Biochem J. 1986. 239(2):445–450.

27. Chen WY, Abatangelo G. Functions of hyaluronan in wound repair. Wound Repair Regen. 1999. 7(2):79–89.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download