Abstract
Background
The purpose of this study is to evaluate the disease-free survival (DFS) and overall survival (OS) of patients with stage IIB osteosarcoma at a single institution for 20 years and to compare the results according to the chemotherapy protocols.
Methods
From Jan 1988 to Nov 2008, 167 patients with osteosarcoma were treated at our hospital and among them, 117 patients (67 males and 50 females) with stage IIB osteosarcoma were evaluable. Their mean age was 22.6 years (range, 8 months to 71 years). Seventy-eight cases underwent the modified T10 (M-T10) protocol (group 1), 23 cases underwent the T20 protocol (group 2) and 16 cases underwent the T12 protocol (group 3). The DFS and OS were calculated and compared according to the chemotherapy protocols.
Results
At a mean follow-up of 78.9 months, 63 patients were continuously disease-free (63/117), 6 patients were alive after having metastatic lesions, 7 patients died of other cause and 41 patients died of their disease. The 5- and 10-year OS rates were 60.2% and 44.8%, respectively and the 5- and 10-year DFS rates were 53.5% and 41.4%, respectively. There was no significant difference of the OS and DFS between the chemotherapy protocols (p = 0.692, p = 0.113).
Conclusions
At present, we achieved success rates close to the internationally accepted DFS and OS. We were able to achieve the higher survival rates using the M-T10 protocol over the 20 years. However, there was no significant difference of results between the chemotherapy protocols. We think the M-T10 protocol will achieve more favorable results in the near future.
Osteosarcoma is the most common primary malignant bone tumor and the treatment of osteosarcoma requires a combined approach of surgery and systemic chemotherapy. Since the introduction of chemotherapy into the multi-modal treatment regimen of osteosarcoma, the prognosis has impressively improved, with long-term survival being achieved by two-thirds of all patients.1-4) The disease-free survival rates have been reported to be between 55-75% in the previous large and multicentric studies.5-8)
The purpose of this study is to evaluate the disease-free survival (DFS) and overall survival (OS) of patients with stage IIB osteosarcoma at a single institution for 20 years and to compare the results according to the chemotherapy protocols.
We reviewed 167 patients who were diagnosed as having osteosarcoma and who were treated at our institution from January 1988 to November 2008. We retrospectively selected 117 patients from among the 167 who met the following criteria: 1) Enneking stage IIB; 2) wide or radical excision of tumor; 3) chemotherapy at our institution; and 4) complete medical records with the last follow-up. The patients with metastatic disease at the time of diagnosis were excluded from this study. The demographics and characteristics of the patients and lesions are reported in Table 1.
The simple radiographs and magnetic resonance imaging of the affected whole bone were obtained, and chest computed tomography and Tc99 bone scintigraphy of the whole body were used for the metastasis work-up. The diagnosis of osteosarcoma was always confirmed on the histologic slides of tumor tissue obtained from an open biopsy and from the resected specimens. The pathological investigation that was done at other centers was repeated by pathologists at our hospital and we obtained another biopsy for a suspicious diagnosis. The surgical stage was assessed according to the system of Enneking et al.9)
The status of the patient with regard to the disease at the time of the final follow-up was recorded as continuously disease free (CDF), no evidence of disease at present, but recurrence or metastasis in the past (NED), died of disease (DOD) or died of other causes (DOC).
The patients who received chemotherapy at our hospital underwent three types of protocols during the study period (Table 2). All the protocols included neoadjuvant chemotherapy. Before May 1994, 16 patients underwent the T12 protocol, which Rosen et al.3,10,11) have described. From June 1994 to April 1999, 45 patients underwent the modified T10 (M-T10) protocol, which has been accurately described in several papers.3,12) From May 1999 to April 2001, 22 patients underwent the T20 protocol and from May 2001 to November 2008, 33 patients underwent the M-T10 protocol again. These protocols have been reported in detail elsewhere.3,10-13)
The adjuvant chemotherapy was based on the histological response to the primary chemotherapy. Good responder patients received the same drugs that were given preoperatively, whereas salvage chemotherapy was done for the poor responders. Patients with pulmonary metastases received thoracotomy at least once, except for those with too many lung lesion to excise or those who were in such poor condition that they could not tolerate the procedure. Of the 117 included patients, 78 patients underwent the M-T10 protocol (group 1), 23 patients underwent the T20 protocol (group 2) and 16 patients underwent the T12 protocol (group 3).
The type of surgery (amputation and limb salvage surgery) as well the type of reconstruction after limb salvage were chosen depending on the tumor location and extension, the involved neurovascular structures, the skeletal maturity and the presence of complicating factors such as displaced pathologic fractures or an infected biopsy site. The time span covered by this study was very long (21 years) and so the surgical techniques for local treatment may have changed, but it was always considered mandatory that the preoperative staging assured the possibility of achieving wide surgical margins and preserving a limb that could at least be partially functional after resection.
The DFS & OS were major focuses of this study. DFS was calculated from the date of biopsy until systemic metastasis, local recurrence or death from toxicity, and other causes of death were considered adverse event. OS was calculated from the date of the diagnostic biopsy until death or the last follow-up visit. The survival curves were calculated according to the Kaplan-Meier method and they were compared by means of the log-rank test (SPSS ver. 12.0, SPSS Inc., Chicago, IL, USA). The calculated survival rates were compared according to the chemotherapy protocols. Statistical significance was set at p-values < 0.05.
At a mean follow-up of 79.8 months, the age distribution was from 8 months old to 71 years old, and the mean age was 22.6 years. There were 67 males and 50 females. Forty-five patients (38.4%) developed pulmonary metastases. Of the patients with pulmonary metastasis, there were 27 males and 18 females and their mean age was 27.0 years (range, 7 to 61 years) and the mean follow-up duration was 85.3 months (range, 5 to 122 months).
Toddler patients were rare, with only 2 patients (1.7%) presenting in the first 5 years of life. About 9 patients (7.6%) were in the first decade of life, 66 (56.4%) were in the second, 16 (13.6%) were in the third, 13 (11.1%) were in the fourth, 6 (5.1%) were in the fifth and 5 (4.2%) were above the sixth.
Of the 117 selected patients, the definite histologic diagnoses were osteoblastic osteosarcoma (n = 81), chondroblastic osteosarcoma (n = 18), fibroblastic osteosarcoma (n = 14) and telangiectactic osteosarcoma (n = 4). The primary lesions were located in the distal femur (n = 49), proximal tibia (n = 38), humerus (n = 11), pelvis (n = 5), proximal femur (n = 3), proximal fibula (n = 4), distal tibia (n = 2), scapula (n = 2), hand (n = 1), distal radius (n = 1), and patella (n = 1) (Table 1).
Sixty-three patients were CDF, 6 patients were NED, 7 patients were DOC, and 41 patients were DOD (Table 3). Sixty-three patients (53.8%) remained continuously event-free. There were 46 systemic metastasis (39.3%), 1 local recurrence (0.8%), 3 died from chemotherapy toxicity, 3 died due to postoperative hypovolemia and 1 died due to renal failure.
For the 117 patients with no initial misdiagnosis, the surgery after neoadjuvant chemotherapy included 7 amputations and 110 limb-salvage procedures. The fifty-three patients who had endoprosthetic reconstruction were managed with only endoprosthetic reconstruction (n = 49) and an autograft-prosthesis-composite (n = 4). Of the forty-nine patients who underwent biological reconstruction, they were managed with an extracorporeally-irradiated (ECI) autograft (n = 19), an allograft (n = 12), a temporary spacer (n = 12), pasteurization (n = 4), ECI with a vascularized fibular bone graft (VFBG) (n =1) and only VFBG (n = 1). Of the eight patients who underwent wide excision without reconstruction, they underwent total scapulectomy (n =2), proximal fibulectomy (n = 3) and type I pelvic resection (n = 2) and 1 had extraskeletal osteosarcoma of the hand (Table 1).
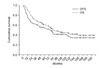
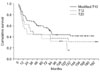
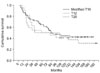
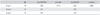
The 5-year DFS was 53.5% and the 5-year OS was 60.2%. The 10-year DFS was 41.4% and the 10-year OS was 44.8% (Fig. 1). As illustrated in Table 4, the 5-year DFS of each group was 59.8% in group 1, 36.3% in group 2 and 43.7% in group 3, and the 5 year OS was 64.6% in group 1, 50.0% in group 2 and 50.0% group 3, respectively (Figs. 2 and 3). There were no significant differences in the 5-year DFS (p = 0.113) and the OS (p = 0.692) between the groups treated with different neoadjuvant chemotherapy; those treated with the group 1 chemotherapy protocol (the M-T10 protocol) had a higher rate of 5-year DFS and 5-year OS than those treated with the remaining 2 protocols.
The results of surgery alone as a treatment for osteosarcoma have not been satisfactory. The 5-year DFS rate after treatment by surgery alone has been reported to be only 12%.14) Neoadjuvant chemotherapy was introduced in 1978.3) The purposes of neoadjuvant chemotherapy are the destruction of the primary tumor cells and the eradication of micrometastasis. Today, using a multi-modal approach consisting of neoadjuvant systemic polychemotherapy followed by local surgical therapy and then adjuvant chemotherapy, long-term, DFS can be achieved in 60-70% of the patients.
However, the DFS rates of 55-65%, which were achieved 10 years ago, have not been improved despite strenuous effort.5,6,8) The study of an Italian group, which evaluated patients with no metastasis at presentation, had a total survival rate of 70% and a DFS rate of 59% at 10 years. A Germany-Austria-Switzerland study group reported a 10-year total survival rate of 59.8% and a 10- year DFS rate of 48.9%. The results we achieved at a single institute are close to these rates.
Our results of DFS and OS showed a slight lower rate than the other internationally data. The first reason for these results was a short minimum follow-up period. Bacci et al.1) reported higher DFS and OS for patients who were followed for at least 5 years. Bielack et al.6) reported 5-, 10- and 15-year event-free survival rates of 52.8%, 49.4%, and 48.3%, respectively. These results are comparable to our results, but our results for over 10-year DFS were lower than the results that Bielack et al.6) reported. To determine accurate results, a long-term follow-up period and at least the 5-year follow-up data are needed.
The second reason that our DFS and OS showed a slight lower rate was that we did not limit the subjects to those with only osteosarcoma of an extremity. We included patients with osteosarcoma of the axial skeleton in the study. The OS of patients with osteosarcoma of the axial skeleton such as pelvis, spine and scapula is considered to be poorer than that of patients with extremity osteosarcoma.15) For these reasons, we suggest our results for the 5- and 10-year DFS and OS were underestimated.
The current standard protocol of a three-drug chemotherapy regimen using cisplatin, doxorubicin and high-dose methotrexate provides about 70% long-term disease-free survival for osteosarcoma patients without metastasis.16) Even with their potential to cause severe, life-threatening toxicity, doxorubicin and methotrexate have been successfully applied as chemotherapy drugs for the treatment of osteosarcoma.17,18) In one study on osteosarcoma chemotherapy, vincristine, bleomycin and dactinomycin were all proven to be ineffective.19,20) Our results also proved the ineffectiveness of the above three drugs.
The benefit of adding ifosfamide, a fourth agent that is generally accepted as being active against the disease, to the regimens of doxorubicin, cisplatin and high-dose methotrexate remains to be confirmed.21,22) The Italian, Scandinavian and COSS groups have used all four drugs together with promising results.21,23,24) However, the addition of ifosfamide did not result in a survival advantage in a large, randomized North American study.25) Subsequently, the addition of cisplatin and ifosfamide to doxorubicin and methotrexate has been able to significantly improve the clinical results.21,26) The M-T10 protocol is now used as the chemotherapy protocol for osteosarcoma patients in our institution. The ongoing challenges include tailoring chemotherapy to the individual risk of relapse and developing biologically driven treatment strategies.
The limitation of this study is the relatively small number of patients compared with the other studies about long-term results of osteosarcoma. The study design represents another limitation, since this was a single institute retrospective study and no randomization chemotherapy protocol was followed during the span of the study.
In conclusion, the 5-year OS rate of osteosarcoma increased from 50% to more than 65% during the study period. Our results for the DFS and OS were close to the internationally accepted rates. We could achieve the higher survival rates using the M-T10 protocol over the 20 years. However, there was no significant difference of the results between the chemotherapy protocols. We think that the M-T10 protocol could achieve more favorable results in the near future.
Figures and Tables
References
1. Bacci G, Longhi A, Fagioli F, Briccoli A, Versari M, Picci P. Adjuvant and neoadjuvant chemotherapy for osteosarcoma of the extremities: 27 year experience at Rizzoli Institute, Italy. Eur J Cancer. 2005. 41(18):2836–2845.

2. Link MP, Goorin AM, Miser AW, et al. The effect of adjuvant chemotherapy on relapse-free survival in patients with osteosarcoma of the extremity. N Engl J Med. 1986. 314(25):1600–1606.

3. Rosen G, Caparros B, Huvos AG, et al. Preoperative chemotherapy for osteogenic sarcoma: selection of postoperative adjuvant chemotherapy based on the response of the primary tumor to preoperative chemotherapy. Cancer. 1982. 49(6):1221–1230.

4. Winkler K, Beron G, Kotz R, et al. Neoadjuvant chemotherapy for osteogenic sarcoma: results of a Cooperative German/Austrian study. J Clin Oncol. 1984. 2(6):617–624.

5. Bacci G, Ferrari S, Bertoni F, et al. Long-term outcome for patients with nonmetastatic osteosarcoma of the extremity treated at the istituto ortopedico rizzoli according to the istituto ortopedico rizzoli/osteosarcoma-2 protocol: an updated report. J Clin Oncol. 2000. 18(24):4016–4027.

6. Bielack SS, Kempf-Bielack B, Delling G, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2002. 20(3):776–790.

7. Petrilli AS, de Camargo B, Filho VO, et al. Results of the Brazilian Osteosarcoma Treatment Group Studies III and IV: prognostic factors and impact on survival. J Clin Oncol. 2006. 24(7):1161–1168.

8. Meyers PA, Gorlick R, Heller G, et al. Intensification of preoperative chemotherapy for osteogenic sarcoma: results of the Memorial Sloan-Kettering (T12) protocol. J Clin Oncol. 1998. 16(7):2452–2458.

9. Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980. (153):106–120.

10. Rosen G. Neoadjuvant chemotherapy for osteogenic sarcoma: a model for the treatment of other highly malignant neoplasms. Recent Results Cancer Res. 1986. 103:148–157.

11. Rosen G, Marcove RC, Huvos AG, et al. Primary osteogenic sarcoma: eight-year experience with adjuvant chemotherapy. J Cancer Res Clin Oncol. 1983. 106:Suppl. 55–67.

12. Rosen G, Huvos AG, Mosende C, et al. Chemotherapy and thoractomy for metastatic osteogenic sarcoma: a model for adjuvant chemotherapy and the rationale for the timing of thoracic surgery. Cancer. 1978. 41(3):841–849.

13. Rosen G. Preoperative (neoadjuvant) chemotherapy for osteogenic sarcoma: a ten year experience. Orthopedics. 1985. 8(5):659–664.

14. Longhi A, Errani C, De Paolis M, Mercuri M, Bacci G. Primary bone osteosarcoma in the pediatric age: state of the art. Cancer Treat Rev. 2006. 32(6):423–436.

15. Fuchs B, Hoekzema N, Larson DR, Inwards CY, Sim FH. Osteosarcoma of the pelvis: outcome analysis of surgical treatment. Clin Orthop Relat Res. 2009. 467(2):510–518.

16. Chou AJ, Gorlick R. Chemotherapy resistance in osteosarcoma: current challenges and future directions. Expert Rev Anticancer Ther. 2006. 6(7):1075–1085.

17. Rosen G, Murphy ML, Huvos AG, Gutierrez M, Marcove RC. Chemotherapy, en bloc resection, and prosthetic bone replacement in the treatment of osteogenic sarcoma. Cancer. 1976. 37(1):1–11.

18. Campanacci M, Bacci G, Bertoni F, Picci P, Minutillo A, Franceschi C. The treatment of osteosarcoma of the extremities: twenty year's experience at the Istituto Ortopedico Rizzoli. Cancer. 1981. 48(7):1569–1581.

19. Avella M, Bacci G, McDonald DJ, Di Scioscio M, Picci P, Campanacci M. Adjuvant chemotherapy with six drugs (adriamycin, methotrexate, cisplatinum, bleomycin, cyclophosphamide and dactinomycin) for non-metastatic high grade osteosarcoma of the extremities: results of 32 patients and comparison to 127 patients concomitantly treated with the same drugs in a neoadjuvant form. Chemioterapia. 1988. 7(2):133–137.
20. Meyers PA, Heller G, Healey J, et al. Chemotherapy for nonmetastatic osteogenic sarcoma: the Memorial Sloan-Kettering experience. J Clin Oncol. 1992. 10(1):5–15.

21. Bacci G, Ferrari S, Longhi A, et al. High dose ifosfamide in combination with high dose methotrexate, adriamycin and cisplatin in the neoadjuvant treatment of extremity osteosarcoma: preliminary results of an Italian Sarcoma Group/Scandinavian Sarcoma Group pilot study. J Chemother. 2002. 14(2):198–206.

22. Smeele LE, Kostense PJ, van der Waal I, Snow GB. Effect of chemotherapy on survival of craniofacial osteosarcoma: a systematic review of 201 patients. J Clin Oncol. 1997. 15(1):363–367.

23. Fuchs N, Bielack SS, Epler D, et al. Long-term results of the co-operative German-Austrian-Swiss osteosarcoma study group's protocol COSS-86 of intensive multidrug chemotherapy and surgery for osteosarcoma of the limbs. Ann Oncol. 1998. 9(8):893–899.

24. Smeland S, Wiebe T, Bohling T, Brosjo O, Jonsson K, Alvegard TA. Chemotherapy in osteosarcoma: the Scandinavian Sarcoma Group experience. Acta Orthop Scand Suppl. 2004. 75(311):92–98.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download