Abstract
Background
Anatomic anterior cruciate ligament (ACL) reconstruction has been presented as a means to more accurately restore the native anatomy of this ligament. This article describes a new method that uses a double bundle to perform ACL reconstruction and to evaluate the clinical outcome.
Methods
Grafts are tibialis anterior tendon allograft for anteromedial bundle (AMB) and hamstring tendon autograft without detachment of the tibial insertion for posterolateral bundle (PLB). This technique creates 2 tunnels in both the femur and tibia. Femoral fixation was done by hybrid fixation using Endobutton and Rigidfix for AMB and by biointerference screw for PLB. Tibial fixations are done by Retroscrew for AMB and by native insertion of hamstring tendon for PLB. Both bundles are independently and differently tensioned. We performed ACL reconstruction in 63 patients using our new technique. Among them, 47 participated in this study. The patients were followed up with clinical examination, Lysholm scales and International Knee Documentation Committee (IKDC) scoring system and radiological examination with a minimum 12 month follow-up duration.
Results
Significant improvement was seen on Lachman test and pivot-shift test between preoperative and last follow-up. Only one of participants had flexion contracture about 5 degrees at last follow-up. In anterior drawer test by KT-1000, authors found improvement from average 8.3 mm (range, 4 to 18 mm) preoperatively to average 1.4 mm (range, 0 to 6 mm) at last follow-up. Average Lysholm score of all patients was 72.7 ± 8.8 (range, 54 to 79) preoperatively and significant improvement was seen, score was 92.2 ± 5.3 (range, 74 to 97; p < 0.05) at last follow-up. Also IKDC score was normal in 35 cases, near normal in 11 cases, abnormal in 1 case at last follow-up.
In spite of many excellent outcomes with arthroscopic anterior cruciate ligament (ACL) reconstruction, problems remain with this procedure; rotation instability and physical disabilities are not always completely resolved.1,2) Rotation stability has been achieved by tunneling the femur at the 10-o'clock position or by double bundle ACL reconstruction.3-8) However, there has been a great deal of debate as to the ability of the double bundle technique with respect to the selection of grafts, fixation methods, and techniques for tightening each bundle.4,5,8,9) Complications of this technique have included failure of graft fixation and excessive tunnel dilation due to an increase in tunnel numbers and adversity when an operation has required revision.
Endobutton (Smith & Nephew, Andover, MA, USA) was introduced and commonly used as a femoral fixation method to overcome limitations in length and thickness of the autograft.5) However, Endobutton has had some problems in the graft healing in the bony tunnel due to shortening of grafted tendons, as well as excessive dilation of tunnels for the receipt of Endobuttons.10) For this reason, we minimized graft motion by fixating the graft with a bio-absorbable transfemoral pin, Rigidfix pin (Mitek, Johnson and Johnson, Raynham, MA, USA). In order to restore the native tibial insertion of ACL, the Retroscrew (Arthrex, Naples, FL, USA) was designed and introduced. It was proven to facilitate optimum joint line fixation at the level of the intercondylar floor for soft tissue autografts and allografts to maximize graft stiffness, fixation strength, abrasion resistance, and anatomical placement.11) To prove its advantages in the clinical setting and in clinical outcomes, we used the Retroscrew as a tibial fixation to the articular outlet of the tibial tunnel for anteromedial (AM) bundle.
In addition, for further fixation to the distal portion, the gracillis and semi-tendinosus tendons, without detachment of the tibial insertion, were used for the posterolateral (PL) bundle, and a bio-absorbable interference screw, Intrafix (Mitek, Johnson and Johnson), was also applied to the articular outlet of the PL femoral tunnel in order to minimize graft motion. Thus, we designed a clinical study to investigate the clinical outcomes of this technique.
From May 2005 to May 2007, 63 patients underwent anterior cruciate ligament reconstruction with our new technique using the double bundle. We excluded patients with combined injuries of the medial or lateral collateral ligaments and posterior cruciate ligament. Patient with a meniscus injury more than and equal to grade 3 in magnetic resonance imaging (MRI)12) were excluded as well as patient who had undergone revisional surgery. We performed a conventional single bundle reconstruction for osteoporotic patients (bone mineral density < -3.0), these was excluded also. However, there were no patients excluded as a result of loss to follow-up. In total, 47 patients were enrolled into this prospective study. The mean time of follow-up was 18.7 months (range, 12 to 23 months); there were 46 males and 1 female; there was an average age of 23.8 years (range, 19 to 38 years) and 38 operations occurred on right knees, while 9 operations occurred on left knees. The time period from trauma to operation was an average of 6.8 months (range, 1 to 22 months). The reason for anterior cruciate ligament reconstruction included the following: 42 patients reported sports injury; 26 reported jumping injuries and 12 reported running injuries when playing soccer, 2 reported jumping injuries when playing basketball, 2 injured during recreational activities, and 5 patients reported having falling down as a result of their occupation.
In 28 cases, we found meniscal injury under arthroscopy: 18 were medial meniscus injuries, 5 were lateral meniscus, and 5 cases were bilateral. For treatment of combined meniscal injury, we sutured torn meniscus in 13 medial meniscus injuries, 3 lateral meniscus injuries; we did menisectomy in 10 medial meniscus injuries, 6 lateral meniscus. In one case of lateral meniscus injury, we performed a meniscal transplantation using an allograft after 6 months after total menisectomy.
We performed the Lachman test and the pivot-shift test prior to operation and at last follow-up. In addition, we used the Lysholm score and International Knee Documentation Committee (IKDC) for clinical outcome evaluation. For the evaluation of instability, we used the KT-1000 (Medmetric Co., San Diego, CA, USA) arthrometer. A second-look arthroscopy was performed in 28 cases. The indication for second-look arthroscopy was those persons wanted to remove the screw for tibial fixation of the graft 1 year postoperative (average, 13.2 months; range, 12 to 18 month).
We classified graft tension by pulling the middle portion of the graft with probe at 80o flexion of knee joint. If the graft pulled less than 3 mm on the basis of lateral femoral condyle, it was considered 'Normal'. If the graft pulled 4 to 5 mm, it was considered 'Partial Relaxation'. If the graft was torn or pulled over 5 mm, it considered a 'Failure'.13) In addition, we classified synovial formation into 3 categories. When the graft was covered with synovial membrane completely, we made a judgment of 'Good'. When the synovial membrane was thin or insufficient compared with the posterior cruciate ligament, it was considered 'Half'. In cases of minimal synovialization and visible strands of graft, we considered it 'Pale'.13)
In evaluation of continuous variables, we used the paired t-test in evaluation of knee scores, results of KT-1000 arthrometers and the Wilcoxon signed-rank test in evaluation of the Lachman test, degree of synovialization, and pivot-shift test. Spearson correlation analysis was used in the evaluation of follow-up periods and in the degree of graft tension that occurred in second-look operations. The statistical program SPSS ver. 11.0 (SPSS Inc., Chicago, IL, USA) was for statistical analyses. The level of significance was set at a p-value less than 0.05.
Tibialis anterior tendon allograft is obtained for the AM bundle, and the gracillis and semi-tendinosus tendon, without detachment of the tibial insertion, are used for the PL bundle. The tibialis allograft is double-looped, 8 mm in thickness and ≥ 120 mm in total length, so that additional fixation to the tibia. Endobutton is suspended at the looped portion of the allograft in relation to the length of a femoral tunnel. Whipstitch sutures with No. 2 Ethibond were placed 3 cm below the suspended site, and No. 1 Ethibond (Ethicon, Somerville, NJ, USA) was passed through the 2 holes of the Endobutton (Fig. 1A). The hamstring tendon graft is harvested cautiously with an open tendon stripper, in order to prevent the insertion site from detaching from the tibia. Gracillis and semi-tendinosus tendons are sutured to form 1 bundle that measures 6 mm in thickness and ≥ 120 mm in total length (Fig. 1B). Whipstitch sutures with No. 2 Ethibond were placed 3 cm below the femoral end of the graft, and 5-0 Ethibond sutures were placed in the femoral end of the graft.
After minimal notchplasty, the tibia is first reamed for the PL bundle with the knee held in 90 degrees of flexion. An ACL tibial guide (Acufex Micro Surgical, Mansfield, MA, USA) set a 45 degrees is introduced through the anteromedial portal. The tunnel is reamed with consideration of the graft size after the intra-articular side is placed 5 mm anterior to the posterior cruciate ligament, just in the anteromedial portion of the posterior horn of the lateral meniscus, and in the posterolateral portion of ACL footprint (Fig. 2A).
The tibial tunnel for the AM bundle was made at the extra-articular portion, which was placed 1.5 cm above the upper margin of the pes anserius and 1 cm posterior to the medial margin of the tibial tubercle. An ACL tibial drill guide set at 40° is placed 7 mm anterior to the PL bundle, while the intra-artucular starting point was maintained in the anteromedial portion of ACL footprint (Fig. 2A). The tibal tunnel was reamed over a guide pin according to the diameter of graft and a transtibial technique that was used. The femoral tunnel for the AM bundle was reamed proximal to and posterior to femoral ACL footprint. After a 6 mm off set guide was introduced through the tibial tunnel into the intra-articular space and was placed at the 10- to 10:30-o'clock position and 6 mm anterior to the posterior margin of the intercondylar notch in the case of a right knee. When the target position was reached, the tunnel was reamed with a 4.5 mm Endobutton cannulated drill over the guide pin, and the tunnel length was measured. The femoral tunnel was reamed with consideration of a diameter of 8 mm that allows for Endobutton rotation, a length of 30 mm that allows for fixing a Rigidfix pin, and the diameter of the graft.
The femoral tunnel was reamed for the PL bundle with an ACL guide by the outside-in technique. After introducing an ACL guide through the anterolateral portal, the intra-articular side on medial wall of the lateral femoral condyle was placed 5-7 mm above to the lateral meniscus posterior horn at 90 degree knee flexion. The guide pin was positioned towards the intra-articular side of the bundle in the just posterior and proximal portion of the lateral femoral epicondyle. The tunnel was reamed along the guide pin, and the distance between the 2 femoral tunnels was maintained at ≥ 4 mm. The wire loop was pulled out of the posterolateral tibial tunnel after being introduced into the intra-articular space from the lateral femoral condyle.
A femoral Ethibond suture of the graft for the PL bundle was suspended to a wire loop that was pulled out of the PL tibial tunnel and the graft for the PL bundle was introduced through the femoral tunnel via a wire loop (Fig. 3A). After a tension-measuring instrument is connected to the PL bundle, cyclic loading was applied to the graft 20 times, at a tension of 15-20 lbs. Next, a bio-absorbable interference screw, Intrafix was introduced through the anteromedial portal into the intra-articular surface and fixed to the femur with the knee held in 10-20 degrees of flexion. Before the AM bundle was introduced through the tunnel, a Retroscrew was prepared for insertion. After introducing a No. 5 fiberwire through the anteromedial portal into the intra-articular space and pulling it out of the anteromedial tibial tunnel to the extra-articular space, a cannula was introduced through the antermedial portal, and the suture was tucked in the cannula. Thereafter, a guide pin was introduced through the tunnel for the AM bundle by the transtibial approach. The No. 5 Ethibond suture in the AM bundle was tied to the eyelet of the guide pin and the graft for AM bundle was introduced through the tibial tunnel to the femoral tunnel by pulling out the No. 5 Ethibond suture. After the Endobutton was flipped, 1 Rigidfix bioabsorbable pin (length, 42 mm; diameter, 3.3 mm; Rigid Fix, Ethicon, Depuy Mitek Division, Norderstedt, Germany) was fixed to the proximal portion of the sheath by preparing the site in a manner so to prevent the graft from wrapping around the sheath (Fig. 3B); it's the tight fixation was confirmed by pulling the graft. Another Rigidfix pin was applied to the distal portion. After cyclic loading was applied about 20 times at 15-20 lbs of tension, with the knee held at 60-70 degrees of flexion, a suture was connected to a Retroscrew and tucked in the intraarticular space with a pituitary rongeur. The suture outside the tibial tunnel was fixed with a cannulated Retroscrew driver, while it was advanced retrograde in the tunnel, then the AM bundle outside the tibia was fixed with 2 staples or with a 6.5 mm spiked washer screw (Fig. 3C).
After skin closure, cylinder splint was applied with full extension of the knee joint. Splint was maintained until subsiding of postoperative pain approximately 2 days. After the closed drain removed, continuous passive range of motion exercise was started. For recovery of range of motion by 90° flexion at postoperative 4 weeks, partial weight bearing ambulation with crutch was permitted at postoperative 1 day and hinged knee brace with limited motion was applied at postoperative 2 days with increasing exercise intensity and maintained at 4 weeks postoperative. After 6 weeks of partial weight bearing, full weight bearing was permitted at 7 weeks postoperative and patients were educated on being completely postoperative at 3 months. We had the patients to start muscle strengthening exercises after disappearance of postoperative pain; bicycling exercise was allowed at postoperative 2 months; swimming was allowed at 3 months postoperative; and light exercise, such as jogging, was allowed at 6 months postoperative; every sports activity was allowed at 9 months postoperative.
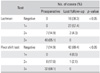
Significant improvement was seen on Lachman test and pivot-shift test between preoperative and last follow-up (Table 1). At last follow-up, negative in pivot-shift test was seen in 42 cases. In range of motion, there was preoperative flexion contracture between 5 to 10 degrees in 8 cases. In one case, flexion contracture remained of about 5 degrees at last follow-up.
We checked the difference from contralateral side in anterior drawer test by KT-1000 before operation and at last follow-up (Table 2). We found improvement from an average 8.3 mm (range, 4 to 18 mm) preoperative to average 1.4 mm (range, 0 to 6 mm) at last follow-up. At last follow-up, a difference of less than 3 mm was seen in 42 cases. In one case, a 6 mm difference was seen.
Average Lysholm score of whole patients was 72.7 ± 8.8 (range, 54 to 79) preoperative. At last follow-up, significant improvement was seen, score was 92.2 ± 5.3 (range, 74 to 97; p < 0.05). At last follow-up, IKDC score was normal (A) in 35 cases, near normal (B) in 11 cases, abnormal (C) in 1 case. There was no patient that was considered severely abnormal (D) (Table 3).
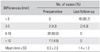
In the 28 cases that required a second-look operation, graft tension was checked at 80° flexion.13) The anteromedial bundle wasnormal in 22 cases, while partial relaxation was reported in 6 cases. There were no cases of failure. The posterolateral bundle was normal in 16 cases, partially relaxation in 8 cases, and failure was seen in 4 cases. There was no correlation between follow-up periods and degree of graft tension in anteromedial and posterolateral bundles (p = 0.48, 0.31).
Synovial membrane formation of graft was reported as good in 18 cases, half in 9 cases, pale in 1 case in anteromedial bundle. The posterolateral bundlewas good in 16 cases, half in 8 cases, and pale in 4 cases. However, there was no significant correlation between graft tension and clinical results (p > 0.05).
Intraoperative complication was seen in 5 cases during the flipping of Endobutton device. We confirmed fixation of Endobutton by pulling graft after flipping Endobutton. In cases where the skin retracted when the graft pulled, we checked the radiograph during operation. The Endobutton had not been fully attached to the femur due to impingement in muscles, so we put additional incisions to release impinged muscles and repositioned the Endobutton. Complications after the operation were reported in 13 cases. Sensory changes at the donor site occurred in 12 cases, superficial infection was reported in 1 case. There was no deep infection. Among 28 cases taken second-look operation, partial rupture was seen in the posterolateral bundle in 4 cases and debridement was performed in these cases. Despite partial rupture, satisfactory clinical results were shown.
In double bundle ACL reconstruction, there are controversies and weaknesses. One of them is taking much time for graft incorporation into bone due to an increase in the number of tunnels. Therefore, we did not detach the tibial insertion of the hamstring tendon autograft in order to obtain a more durable fixation of the distal portion of the graft or to shorten incorporation time into bone with a more viable graft.14) Also, we were able to reduce discomfort in the tibial area during postoperative rehabilitation due to excessive volume of the graft in the anteromedial portion of the tibia after tibial fixation by using the conventional technique, since fixation of the PL bundle was not needed in our technique (Fig. 4).14) But, there were limitations, such as lengthened fixation length causing tunnel widening.
Edwards et al.15) have reported that the most excellent outcome can be obtained when 2 tunnels are used for the tibia and the femur each, respectively. Thus, we used 2 tibial and 2 femoral tunnels, because the single tibial tunnel technique can be difficult in the restoration of the native shape of the ACL. But the increase in the number of tunnels may lead to some disadvantages, such as difficulty in the operative technique and more frequent occurrence of dilation of tunnels. Siebold et al.16) found that MRI taken at the 1-year follow-up revealed remarkable dilation of the 2 femoral tunnels when 2 tibial tunnels are broken and communicated in double bundle ACL reconstruction using 4 tunnels. Authors were able to separate 2 tibial tunnels by leaving the tibial cortical bone between them when reaming the tibial tunnel.
The choice of grafts is inevitable issue in discussion of our technique. Many graft options are available for ACL reconstruction, including different autograft and allograft tissues. Autografts include bone-patellar tendonbone composites, combined semitendinosus and gracilis hamstring tendons, and quadriceps tendon. Allograft options include the same types of tendons harvested from donors, in addition to Achilles and tibialis tendons. In studies deal with graft choice recently, allografts proved its durability and strength in single-bundle technique17) and double bundle technique,18) and through comparison with autografts.19) Though risk of graft failure was higher in hamstring tendon than bone-patellar tendon-bone grafts, the hamstring tendon has shown favorable clinical results. For this reason, we thought there would be no difficulties using allografts in double-bundle reconstruction.20) But, in aspect of interaction between autograft and allograft, we could not predict the types of side effects. Studies discussed this subject have to be done in near future.
Endobutton is also one of subjects in controversy. Although several authors have recently used Endobutton to fix short grafts, this technique has difficulty to fix at femoral cortex accurately. We experienced 4 cases in which Endobutton was not able to attach to the femoral cortex because of a bottleneck between muscles. So, we recommend if skin retraction was seen when pulling graft after turning of Endobutton, intraoperative radiograph should be taken to confirm the fixation of Endobutton. In addition, Endobutton has led to dilation of the tunnel and the bungee cord effect, which is perpendicular motion of a graft due to distant fixation of each end of the graft. To this effect, the authors fixed 2 additional Rigidfix pins in order to strengthen Endobutton fixation. There have been many studies suggesting that 2 Rigidfix pin possessed adequate strength to fix a graft.21) Between them, Kousa et al.22) reported Rigidfix showed fixation failure at 868N at single cycle load to failure test in biomechanical analysis. However, we experienced 7 cases in which the graft descended or the pin was broken while applying the cyclic load 20 times in case of fixation with the Rigidfix pin alone. Han et al.23) also reported breakage of Rigidfix pin at femoral tunnel after anterior cruciate ligament reconstruction with hamstring tendon graft. Consequently, we avoided single Rigidfix pin fixation. Through additional Rigidfix pin fixation with Endobutton, the femoral tunnel fixation was close to the intercondylar notch, so graft motion could be minimized. And we used a Retroscrew for the tibial graft for reducing fixation length in tibial fixation close to its natural anatomy, and as natural consequence, we could achieve juxta-articular fixation as compared with antegrade screw fixation. Also, divergence of Retroscrew can be avoided by fixing it under arthroscopy.11) In aspects of graft tension, the theoretical advantages of Retroscrew had not been proven in other studies. In a biomechanical study by Chang et al.,24) antegrade bioscrew showed advantages compared to Retroscrew such as superior stiffness, less displacement, greater maximum load at failure in the porcine knee. Shortages of Retroscrew as technical difficulties, low bone density in tibial metaphysis and small diameter could be thought cause of this unfavorable result. So, more clinical study for Retroscrew has to be done to clear this debate.
Clinical studies involving double-bundle reconstruction have been available for several years. In 1999, Muneta et al.8) published the results of a 2-year follow-up in 54 patients who underwent double-bundle reconstruction. They reported a "trend" toward improved anterior tibia translational stability, but no patient data or parameters were available. Kubo et al.25) and Hara et al.26) published that their technique was a "physiologically more durable ACL reconstruction," but outcome data or statistics were not described. Recently, studies with patients' data and outcomes published,9) though its double-sidedness. Between those studies, KT-1000 or 2000 arthrometry is known as the most reliable and reproducible parameter for measurement of anterior translation available. Various results of KT-1000 or 2000 arthrometry as 1.7 ± 2.0 mm, 1.4 ± 1.4 mm, 1.6 ± 2.0 mm, 1.9 ± 1.9 mm, 1.7 ± 2.0 mm was reported by numerous authors.6,7) We found an improvement from an average 8.3 mm (range, 4 to 18 mm) preoperative to an average 1.4 mm (range, 0 to 6 mm) at last follow-up in contrast to the unsatisfactory results of the Lachman test, which had negative results on 38.3% of the time. Despite in the development of bias in comparin our results of anterior translation directly, to other authors' finding, our results are superior to other studies. We regarded this superior outcomes comes from several advantages of our technique. First, viable grafts were obtained by maintaining tibial insertion of the hamstring tendon autograft. Second, AM and PL bundles were fixed to the knee joint at diff erent angles. Third, adequate graft length for fixation were achieved by using the tibialis tendon allograft and the hamstring tendon autograft with intact tibial insertion.
Besides limitations of the study design such as the short follow-up period, small sample size and need of comparing clinical results of our technique to single bundle technique and conventional double bundle technique, in our technique, there are some limitations and disadvantages by its own nature. Same as other technique, it is technically difficult to perform and require a learning curve. Besides technical demands, cost-effectiveness is another weak point. Allograft itself could burden patients with high cost instrument system such as Rigid fix pin system and Retroscrew system we used in this study. If studies that compare our double bundle technique to conventional single-bundle technique could not be done or there were no significant differences between techniques at all, continuous application of our technique could not be recommended. Even if our technique was proven superior to other double bundle techniques, clinicians must consider its cost-effectiveness. In addition, unsuccessful results of PL bundle in second-look operation is our big weakness. In 4 cases among 28 cases that took second-look operation were shown failure of PL bundle and 8 cases of partial relaxation were shown. It could eliminate advantage of double bundle reconstruction. In some point, causal factors of this unfavorable result considered. Nature of PL bundle could make excessive motion of graft, which might be related to the higher non-isometric function of the PL bundle compared with the AM bundle as Siebold and Cafaltzis27) described in study about postoperative bone tunnel widening. Regarding the graft fixation, authors fixed the AM bundle with the knee held in 60 degrees of flexion and the PL bundle with the knee held in 0 to 10 degrees of flexion. Considering that 2 bundles are fixed with the knee held in 30 degrees of flexion in double bundle reconstruction, it is conceivable that excessive tension may rupture the PL bundle and overconstrain knee.28) Despite our attempt not to give too much tension to PL bundle, knee flexion angle during PL bundle fixation with the knee held in 0 to 10 degrees of flexion might not have been sufficient for preserving PL bundle for some reasons authors didn't recognize. Fixation method which remains native insertion of hamstring tendon can be one of the causes. The authors did not perform additional fixation because of bio-interference screw at tibial tunnel of PL bundle, which made fixation length long as described above. Excessive motion of autograft due to this long fixation length may have induced the failure of PL bundle. Femoral tunnel positioning could be one of reasons, because transtibial technique is not appropriate method to make femoral tunnel anatomically as Giron et al.29) discovered. The sequence of creating 2 femoral tunnel might have affected the PL bundle failure. We created a femoral tunnel for AM bundle first in this study. However, Taketomi et al.30) reported PL tunnel first technique seems to be superior to AM first technique regarding anatomic placement. Non-anatomic PL tunnel placement could be a reason of PL bundle failure.
Despite these limitations, our study is significant because we attempted to apply a theoretical possibility to clinical circumstances. This could be a proposal for further progression of double bundle ACL reconstruction.
In conclusions, our new double bundle ACL reconstruction technique used hybrid fixation and Retroscrew with favorable outcomes. But, this technique should be evaluated further in regards to technical difficulty, cost-effectiveness, and the relatively unsatisfactory results of the posterolateral bundle.
Figures and Tables
Fig. 1
(A) The tibialis allograft is prepared (a, 30 mm for the femoral tunnel; b, 30 mm for the intra-articular space; c, 40 mm for the tibial tunnel). Mersilene tape of the Endobutton is suspended at the looped portion of the allograft. Whipstitch sutures with No. 2 Ethibond are placed 3 cm below the suspended site. (B) Anterolateral view of the operative right knee: The hamstring tendon autograft was harvested and prepared. The gracillis and semi-tendinosus tendons are stripped from the femoral side without detachment of the tibial insertion site (left) (a, 40 mm for the tibial tunnel; b, 20 mm for the intra-articular space; c, 30 mm for the femoral tunnel). The portion for tibial tunnel of graft was prepared with Ethibond (right).

Fig. 2
(A) Tibial tunnel for posterolateral (PL) bundle and anteromedial (AM) bundle was seen on arthroscopic view. (B) Anterior cruciate ligament (ACL) footprint of PL bundle (arrow) was seen on intercondylar notch of femoral condyle (left) and femoral tunnel of the PL bundle was guided at remnant of the ACL footprint using outside-in technique (right).

Fig. 3
(A) Wire loop is introduced through the posterolateral (PL) femoral tunnel via outside-in technique (left) and a femoral Ethibond suture of the graft for the PL bundle is suspended to a wire loop that is pulled out of the PL tibial tunnel and the graft for the PL bundle is introduced through the femoral tunnel via a wire loop (right). (B) Lateral view of operative right knee: a Rigidfix fixation guide system is introduced into the anteromedial femoral tunnel through a transtibial approach. The guide sheaths are carefully positioned in the lateral epicondylar area 1 cm above the PL femoral tunnel through the skin incision for the fixation of the bundle in order to prevent the graft from wrapping around the sheath. (C) Anteromedial (AM) bundle was fixed with Retroscrew at tibial articular side (left) and with 1 spiked washer screw outside the tibia. Hamstring autograft for PL bundle was seen at medial side of AM bundle with no fixation (arrow) (right). (D) Final view of the construct at 90° of flexion showing the PL bundle crossing the AM bundle from the back.

References
1. Aglietti P, Buzzi R, Zaccherotti G, De Biase P. Patellar tendon versus doubled semitendinosus and gracilis tendons for anterior cruciate ligament reconstruction. Am J Sports Med. 1994. 22(2):211–217.

2. Kim SJ, Jung KA, Song DH. Arthroscopic double-bundle anterior cruciate ligament reconstruction using autogenous quadriceps tendon. Arthroscopy. 2006. 22(7):797.e1–797.e5.

3. Loh JC, Fukuda Y, Tsuda E, Steadman RJ, Fu FH, Woo SL. Knee stability and graft function following anterior cruciate ligament reconstruction: comparison between 11 o'clock and 10 o'clock femoral tunnel placement. 2002 Richard O'Connor Award paper. Arthroscopy. 2003. 19(3):297–304.

4. Yagi M, Wong EK, Kanamori A, Debski RE, Fu FH, Woo SL. Biomechanical analysis of an anatomic anterior cruciate ligament reconstruction. Am J Sports Med. 2002. 30(5):660–666.

5. Yasuda K, Kondo E, Ichiyama H, et al. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy. 2004. 20(10):1015–1025.

6. Aglietti P, Giron F, Cuomo P, Losco M, Mondanelli N. Single- and double-incision double-bundle ACL reconstruction. Clin Orthop Relat Res. 2007. 454:108–113.
7. Muneta T, Koga H, Mochizuki T, et al. A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing singlebundle and double-bundle techniques. Arthroscopy. 2007. 23(6):618–628.

8. Muneta T, Sekiya I, Yagishita K, Ogiuchi T, Yamamoto H, Shinomiya K. Two-bundle reconstruction of the anterior cruciate ligament using semitendinosus tendon with endobuttons: operative technique and preliminary results. Arthroscopy. 1999. 15(6):618–624.

9. Hamada M, Shino K, Horibe S, et al. Single- versus bisocket anterior cruciate ligament reconstruction using autogenous multiple-stranded hamstring tendons with endobutton femoral fixation: a prospective study. Arthroscopy. 2001. 17(8):801–807.

10. Yamazaki S, Yasuda K, Tomita F, Minami A, Tohyama H. The effect of graft-tunnel diameter disparity on intraosseous healing of the flexor tendon graft in anterior cruciate ligament reconstruction. Am J Sports Med. 2002. 30(4):498–505.

11. Morgan CD, Stein DA, Leitman EH, Kalman VR. Anatomic tibial graft fixation using a retrograde bio-interference screw for endoscopic anterior cruciate ligament reconstruction. Arthroscopy. 2002. 18(7):E38.

12. Reicher MA, Hartzman S, Duckwiler GR, Bassett LW, Anderson LJ, Gold RH. Meniscal injuries: detection using MR imaging. Radiology. 1986. 159(3):753–757.

13. Ahn JH, Cho YB, Lee JY. Second-look arthroscopy after ACL reconstruction: comparison of patellar tendon autografts with hamstring tendon autografts. J Korean Orthop Assoc. 2003. 38(2):159–164.

14. Kim SJ, Kim HK, Lee YT. Arthroscopic anterior cruciate ligament reconstruction using autogenous hamstring tendon graft without detachment of the tibial insertion. Arthroscopy. 1997. 13(5):656–660.

15. Edwards TB, Guanche CA, Petrie SG, Th omas KA. In vitro comparison of elongation of the anterior cruciate ligament and single- and dual-tunnel anterior cruciate ligament reconstructions. Orthopedics. 1999. 22(6):577–584.

16. Siebold R, Dehler C, Ellert T. Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2008. 24(2):137–145.

17. Kuhn MA, Ross G. Allografts in the treatment of anterior cruciate ligament injuries. Sports Med Arthrosc. 2007. 15(3):133–138.

18. Royalty RN, Junkin DM Jr, Johnson DL. Anatomic double-bundle revision anterior cruciate ligament surgery using fresh-frozen allograft tissue. Clin Sports Med. 2009. 28(2):311–326.

19. Lee JH, Bae DK, Song SJ, Cho SM, Yoon KH. Comparison of clinical results and second-look arthroscopy findings after arthroscopic anterior cruciate ligament reconstruction using 3 different types of grafts. Arthroscopy. 2010. 26(1):41–49.

20. Reinhardt KR, Hetsroni I, Marx RG. Graft selection for anterior cruciate ligament reconstruction: a level I systematic review comparing failure rates and functional outcomes. Orthop Clin North Am. 2010. 41(2):249–262.

21. Harilainen A, Sandelin J. A prospective comparison of 3 hamstring ACL fixation devices--Rigidfix, BioScrew, and Intrafix--randomized into 4 groups with 2 years of follow-up. Am J Sports Med. 2009. 37(4):699–706.

22. Kousa P, Jarvinen TL, Vihavainen M, Kannus P, Jarvinen M. The fixation strength of six hamstring tendon graft fixation devices in anterior cruciate ligament reconstruction. Part I: femoral site. Am J Sports Med. 2003. 31(2):174–181.

23. Han I, Kim YH, Yoo JH, Seong SC, Kim TK. Broken bioabsorbable femoral cross-pin after anterior cruciate ligament reconstruction with hamstring tendon graft: a case report. Am J Sports Med. 2005. 33(11):1742–1745.

24. Chang HC, Nyland J, Nawab A, Burden R, Caborn DN. Biomechanical comparison of the bioabsorbable RetroScrew system, BioScrew XtraLok with stress equalization tensioner, and 35-mm Delta Screws for tibialis anterior graft-tibial tunnel fixation in porcine tibiae. Am J Sports Med. 2005. 33(7):1057–1064.

25. Kubo T, Hara K, Suginoshita T, et al. Anterior cruciate ligament reconstruction using the double bundle method. J Orthop Surg (Hong Kong). 2000. 8(2):59–63.

26. Hara K, Kubo T, Suginoshita T, Shimizu C, Hirasawa Y. Reconstruction of the anterior cruciate ligament using a double bundle. Arthroscopy. 2000. 16(8):860–864.

27. Siebold R, Cafaltzis K. Differentiation between intraoperative and postoperative bone tunnel widening and communication in double-bundle anterior cruciate ligament reconstruction: a prospective study. Arthroscopy. 2010. 26(8):1066–1073.

28. Anderson CJ, Westerhaus BD, Pietrini SD, et al. Kinematic impact of anteromedial and posterolateral bundle graft fixation angles on double-bundle anterior cruciate ligament reconstructions. Am J Sports Med. 2010. 38(8):1575–1583.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download