Abstract
Background
We would like to analyze the risk factors of no thumb test among knee alignment tests during total knee arthroplasty surgery.
Methods
The 156 cases of total knee arthroplasty by an operator from October 2009 to April 2010 were analyzed according to preoperative indicators including body weight, height, degree of varus deformity, and patella subluxation and surgical indicators such as pre-osteotomy patella thickness, degree of patella degeneration, no thumb test which was evaluated after medial prepatella incision and before bone resection (1st test), no thumb test which was evaluated with corrective valgus stress (2nd test, J test), and the kind of prosthesis. We comparatively analyzed indicators affecting no thumb test (3rd test).
Results
There was no relation between age, sex, and body weight and no thumb test (3rd test). Patellar sulcus angle (p = 0.795), patellar congruence angle (p = 0.276) and preoperative mechanical axis showed no relationship. The 1st no thumb test (p = 0.007) and 2nd test (p = 0.002) showed significant relation with the 3rd no thumb test. Among surgical indicators, pre-osteotomy patella thickness (p = 0.275) and degeneration of patella (p = 0.320) were not relevant but post-osteotomy patellar thickness (p = 0.002) was relevant to no thumb test (3rd test). According to prosthesis, there was no significance with Nexgen (p = 0.575). However, there was significant correlation between Scorpio (p = 0.011), Vanguard (p = 0.049) and no thumb test (3rd test). Especially, Scorpio had a tendency to dislocate the patella, but Vanguard to stabilize the patella.
The no thumb test is the most common and convenient clinical examination technique that is used to evaluate patellar alignment during total knee arthroplasty (TKA).1-3) Although some studies question the reliability of the test due to its oversensitivity,4) we believe the test could be a useful diagnostic aid. Unfortunately, the test is carried out at almost the last stage of operation and hence the surgeon's option for correcting patellar alignment is limited to lateral retinacular release. Therefore, we designed this study to explore ways to predict patellar instability in the early stage of operation.
In this study, we analyzed the impact of various indicators on the no thumb test (3rd test) performed after bone resection and implant insertion: preoperative indicators, age, gender, weight, the degree of varus deformity and radiologic patellar subluxation; pre-osteotomy intraoperative indicators, the patella thickness before bone resection, degree of patella degeneration, and the 1st no thumb test performed between medial patella incision and bone resection (1st test), and the 2nd no thumb test performed with corrective valgus stress (2nd test; J test); and post-osteotomy intraoperative indicators, the patella thickness after bone resection and the kind of prosthesis.
A total of 156 patients (156 cases) who underwent TKA between October 2009 and April 2010 were enrolled in this study. There were 149 females (95.5%) and 7 males (4.5%) with a mean age of 68.7 years (range, 53 to 83 years). The prosthesis used was Nexgen (LPS-Flex, Nexgen, Zimmer, Warsaw, IN, USA) in 13 cases (8.3%), Scorpio (NRG, Osteonics, Stryker, NJ, USA) in 50 cases (32%), and Vanguard (Vanguard Knee System, Biomet, Warsaw, IN, USA) in 93 cases (59.7%).
The surgery was performed by the same surgeon via a medial parapatellar approach in all cases. Distal femoral bone resection was done with 5° to 6° of external rotation relative to the posterior condylar axis using a sonographyguided extramedullary alignment guide system.5-7) Proximal tibial resection was done using an extramedullary alignment guide. The posterior cruciate ligament was removed and a prosthesis was inserted in all cases. If the post-osteotomy no thumb test (3rd test) was positive, a lateral release (patellar retinacular peel) was performed.8-10) A tourniquet was applied at 250 mmHg during surgery in all cases. A suction drainage was not used after surgery in all cases.
All the patients' weight and height were measured before surgery. The sulcus angle, congruence angle, and mechanical axis angle were measured on the preoperative radiographs. The pre-osteotomy patella thickness, degree of patella degeneration, and post-osteotomy patella thickness were evaluated. Intraoperatively, the 1st no thumb test (1st test) was performed before bone resection to assess patellar dislocation with the knee in flexion after partial removal or incision of the medial retinaculum, anterior cruciate ligament, posterior cruciate ligament, medial meniscus, patellofemoral ligament, infrapatellar fat pad, and osteophyte. Then, the 2nd no thumb test (2nd test; J-test) was performed to assess patellar dislocation with a valgus force applied. After bone resection and implant insertion, the 3rd no thumb test (3rd test) was performed under the same condition. If patella dislocation was observed in the test, a lateral release was performed. This was followed by the 4th no thumb test in which a patella that slips laterally from the femoral trochlear groove or remains 2 cm away from the medial femoral condyle was considered positive.
Logistic multiple regression analysis was performed to evaluate the effects of all valuables above mentioned. Receiver operating characteristic (ROC) curves of the those significant valuables were analyzed to calculate the sensitivity and specipicity to the 3rd no thumb test (3rd test). A p-value < 0.05 was considered statistically significant and dBSTAT 5.0 (2010; DBSTAT Co., Seoul, Korea) was used for statistical analysis.
The preoperative indicators including age, weight, height, and gender were not correlated with the no thumb test (3rd test). The preoperative radiographic indicators including the sulcus angle, congruence angle, and the mechanical axis angle were not related with the no thumb test (3rd test; p = 0.795, p = 0.276, and p = 0.593, respectively). The 1st no thumb test and the 2nd test performed with a varus force applied before bone resection were correlated with each other and the 2nd test was correlated with the 3rd test that was performed after bone resection (p = 0.007 and p = 0.002, respectively). The 3rd no thumb test was not related with the pre-osteotomy patella thickness (p = 0.275) but was correlated with the post-osteotomy patella thickness (p = 0.002).
With regard to the kind of prosthesis, Nexgen was not correlated with the 3rd no thumb test (p = 0.197). Scorpio and Vanguard were correlated with the 3rd no thumb test, causing more patella dislocation (p = 0.011) and more patellar stability (p = 0.049), respectively.
Of the results we obtained, significant results were examined in more detail. 3% of the cases was positive in the 1st test, 48% was positive in the 2nd test, and 10% was positive in the 3rd test. In the 4th test that was done after the lateral release, 4% of the cases were positive. Of the 4 cases that were positive in the 1st test, all were also positive in the 2nd test, 2, in the 3rd test, and 1, in the 4th test. Of the 78 cases that were positive in the 2nd test, 15 were positive in the 3rd test indicating a 19.2% positive predictive value. Of the 78 cases that were negative in the 2nd test, 76 were negative in the 3rd test, indicating a 97.4% negative predictive value. Of the 17 cases that were positive in the 3rd no thumb test, 15 were positive in the 2nd test, indicating 88.2% sensitivity. Of the 139 cases that were negative in the 3rd no thumb test, 63 were positive in the 2nd test, indicating 54.7% specificity.
Regarding the relationship between the kind of prosthesis and the 3rd no thumb test and the 4th no thumb test, Scorpio was the implant inserted in the 6 cases that showed instability in the 4th no thumb test that was carried out after lateral release (patellar retinacular peel).
Of the 17 cases that showed instability in the 3rd no thumb test, Vanguard was used in 3 cases and Scorpio was used in the remaining 14 cases.
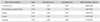
Comparative ROC curves show the sensitivity and specipicity of these factors toward 3rd no thumb test. J test (2nd no thumb test, p = 0.004), Scorpio (p = 0.011) and post-osteotomy patella thickness (p = 0.012) is significant predictors of 3rd no thumb test. Nexgen was not significant (p = 0.575) and Vangard was significant stabilizer of 3rd no thumb test (p = 0.049) (Table 1, Fig. 1).
Lateral retinacular release has been performed by some authors on patients with a positive no thumb test or poor patellar alignment during TKA,11,12) but its impact on the blood supply of the patella remains controversial.13,14)
The authors of this study believe that a proper measure for improving patella tracking should be taken before bone resection to reduce the risk of worsening the blood supply of the patella. However, the no thumb test and other examination methods may not be helpful because they are designed to be performed after bone resection. It is our understanding that if the risk of patella dislocation can be assessed before bone resection in the 1st or 2nd no thumb test, the surgeon can have more options for proper patella tracking ranging from the established methods of using a small patellar prosthesis, lateral placement of a femoral implant, medial placement of a patellar implant, and increasing external rotation of a femoral implant to the methods we documented in this study including the use of a patella-friendly femoral prosthesis and a large patella osteotomy.
We assessed the pre- and intra-operative indicators in this study. Age and gender are the basic variables required in all medical studies. The degree of varus deformity before surgery is thought to be associated with patella dislocation and closely related with the Q angle. Assuming the preoperative degree of patella subluxation as a risk factor of postoperative patella maltracking, we measured the sulcus angle and congruence angle that have been commonly used to assess patella subluxation. Although the relationship between the patella thickness and patella degeneration have not been addressed in any previous studies, we suspected a relationship between them and investigated them in this study.
Some authors found a strong association between tourniquet application and the no thumb test and suggested to perform the test with the tourniquet deflated due to the hypersensitivity of the test.15) In contrast, many studies showed that tourniquet release before wound closure results in increased blood loss and surgical time and no difference in the incidence of postoperative complications.16,17) Therefore, we attempted to explore indicators that can be measured without tourniquet release in this study.
The no thumb test was positive in 10% of the patients (17 cases), a low positive rate compared to the previous studies. Tourniquet inflation pressure was ≥ 300 mmHg in most studies,15,18-20) but we maintained the pressure at 250 mmHg based on our experience. Although we did not release the pressure during surgery, the relatively low pressure may have partially contributed to the low positive rate, which should be investigated in further studies.
Of the 2 cases that were positive in the 3rd no thumb test after bone resection, 1 was also confirmed positive in the 4th test performed after lateral release. We attributed this to the hypersensitivity of the test that was done without tourniquet release. In addition, lateral instability was not observed in a test using one towel clip with the tourniquet applied although we did not describe it in this study.
The low positive rate in the 3rd no thumb test may have been associated with the 5° to 6° of external rotational femoral ostetomy during procedure that contributed to patellar stability.21) In most studies, 3° of external rotation off the posterior femoral condyles is recommended.22,23) However, some authors suggested ≥ 3° of external rotation in Koreans due to the bone structure differences,24,25) which is congruent with our findings and has been practiced in surgery at our institution.
With regard to the kind of femoral prosthesis, Scorpio has so narrow a femoral trochlear groove that the patella might slip laterally (Fig. 2). In contrast, Vanguard and Nexgen have a patella-friendly femoral trochlear groove that is relatively wide and tilted to allow the patella to be on track. Especially, Vanguard has the widest femoral groove among the three prostheses. We think the relationship between the size and shape of different prostheses and patella tracking should be addressed in further studies.
One of the limitaitons of this study is that it is solely based on intraoperative examination findings without long-term follow-up. We believe our study results should be confirmed by a long-term follow-up study including clinical results. Another limitation is that the impact of tourniquet could not be completely ruled out. However, the significance of this study can be found in the fact that we suggested an examination method using pre-osteotomy indicatrors to predict post-osteotomy patellar stability.
Figures and Tables
Fig. 1
Receiver operating characteristic (ROC) curves show the sensiti vity and specipicity of factors toward 3rd no thumb test. J test (2nd no thumb test, p = 0.004), Scorpio (p = 0.011) and post-osteotomy patella thickness (p = 0.012) are significant predictors of 3rd no thumb test. Nexgen was not significant (p = 0.575) and Vangard was significant stabilizer of 3rd no thumb test (p = 0.049). J test (2nd no thumb test) has high sensitivity but low specificity and post-osteotomy patella thickness has relatively high specificity but low sensitivity.

References
1. Ewald FC. Leg lift technique for simultaneous femoral, tibial and patella prosthetic cementing, rule of "no thumb" for patella tracking and "steel rod rule" for ligament tension. Tech Orthop. 1991. 6(4):44–46.

2. Ogata K, Ishinishi T, Hara M. Evaluation of patellar retinacular tension during total knee arthroplasty: special emphasis on lateral retinacular release. J Arthroplasty. 1997. 12(6):651–656.

3. Yang CC, McFadden LA, Dennis DA, Kim RH, Sharma A. Lateral retinacular release rates in mobile- versus fixed-bearing TKA. Clin Orthop Relat Res. 2008. 466(11):2656–2661.

4. Archibeck MJ, Camarata D, Trauger J, Allman J, White RE Jr. Indications for lateral retinacular release in total knee replacement. Clin Orthop Relat Res. 2003. (414):157–161.

5. Lee S, Kim J, Kim JH, Yang SJ, Ryu CW. A comparison of accuracy between the sonography-guided extramedullary and intramedullary alignment systems for the femoral component in total knee arthroplasty. J Korean Knee Soc. 2009. 21(1):15–21.
6. Matsuda Y, Ishii Y, Ichimura K. Identifying the center of the femoral head using ultrasonography to assess the higher accuracy of femoral extramedullary guides in TKA. J Orthop Sci. 2004. 9(1):6–9.

7. Sawant MR, Murty A, Ireland J. A clinical method for locating the femoral head centre during total knee arthroplasty. Knee. 2004. 11(3):209–212.

8. Chan KC, Gill GS. Postoperative patellar tilt in total knee arthroplasty. J Arthroplasty. 1999. 14(3):300–304.

9. Kim HC, Roh JY, Lee CW, Lee CW, Tak HC. The effect of lateral retinacular peeling in total knee arthroplasty. J Korean Knee Soc. 2006. 18(1):67–73.
10. Shaw JA. Patellar retinacular peel: an alternative to lateral retinacular release in total knee arthroplasty. Am J Orthop (Belle Mead NJ). 2003. 32(4):189–192.
11. Hsu HC, Luo ZP, Rand JA, An KN. Influence of lateral release on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty. 1997. 12(1):74–83.

12. Merican AM, Kondo E, Amis AA. The effect on patellofemoral joint stability of selective cutting of lateral retinacular and capsular structures. J Biomech. 2009. 42(3):291–296.

13. Ritter MA, Campbell ED. Postoperative patellar complications with or without lateral release during total knee arthroplasty. Clin Orthop Relat Res. 1987. (219):163–168.

14. Weber AB, Worland RL, Jessup DE, Van Bowen J, Keenan J. The consequences of lateral release in total knee replacement: a review of over 1000 knees with follow up between 5 and 11 years. Knee. 2003. 10(2):187–191.

15. Kim JH, Kim YJ, Chung US, Chung HK. The effect of tourniquet on patellofemoral tracking during total knee arthroplasty. J Korean Knee Soc. 2005. 17(1):79–83.
16. Burkart BC, Bourne RB, Rorabeck CH, Kirk PG, Nott L. The efficacy of tourniquet release in blood conservation after total knee arthroplasty. Clin Orthop Relat Res. 1994. (299):147–152.

17. Barwell J, Anderson G, Hassan A, Rawlings I. The effects of early tourniquet release during total knee arthroplasty: a prospective randomized double-blind study. J Bone Joint Surg Br. 1997. 79(2):265–268.
18. Cho SH, Ha YC, Chun CW. The role of tourniquet in total knee arthroplasty. J Korean Knee Soc. 2004. 16(1):33–38.
19. Kim HC, Shin SI, Kim YE. The effect of intraoperative tourniquet deflation in total knee arthroplasty. J Korean Knee Soc. 2005. 17(1):34–38.
20. Smith TO, Hing CB. Is a tourniquet beneficial in total knee replacement surgery? A meta-analysis and systematic review. Knee. 2010. 17(2):141–147.
21. Canale ST, Beaty JH. Campbell's operative otrhopaedics. 2008. 11th ed. St. Louis: Mosby Year Book Inc.;265.
22. Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res. 2001. (392):38–45.

23. Olcott CW, Scott RD. The Ranawat Award: femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res. 1999. (367):39–42.
24. Cho WS, Park SS, Kim JH, Kim DH, Kim MY. The discrepancy between eipcondylar and posterior condylar axis of femur in total knee arthroplasty. J Korean Knee Soc. 1999. 11(1):8–12.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download