Abstract
Background
To evaluate the effectiveness of minimally invasive surgery total hip arthroplasty (THA) using the two-incision technique as described by Mears.
Methods
From January 2003 to December 2006, sixty-four patients underwent total hip arthroplasty using the one-incision (group I) and two-incision (group II) technique by one surgeon. There were 34 hips in group I and 30 hips in group II. There was no difference in age, gender, and causes of THA between the two groups. We evaluated the operation time, bleeding amount, incision length, ambulation, hospital stay, and complications between the two groups.
Results
There was no difference in the bleeding amount between the two groups. Operation time was longer in the two-incision group than in the one-incision group. Operation time of the two-incision technique could be reduced after 15 cases. Patients started ambulation after surgery earlier in group II than group I, and the hospital stay was shorter in group II than in group I. There was no difference in clinical results between the two groups. There was no difference in component position of the acetabular cup and femoral stem between the two groups. Intraoperative periprosthetic fracture occurred in four cases (13.3%) in group II.
Since its introduction in the 1960s, total hip arthroplasty (THA) has been improved with the development of implant designs and fixation techniques to produce satisfactory long-term clinical and radiological outcomes. Recently, minimally invasive surgery (MIS) has become the norm in almost all medical fields due to the rapid advancement in technology and constant request from patients. In the orthopedic field, a variety of MIS techniques aimed at causing minimal incision, tissue damage, and less pain and promoting rapid recovery and return to activities of daily living has been invented. Against this backdrop, MIS techniques have also been introduced to THA1-3) to facilitate rapid recovery, shorten hospitalization, and obtain satisfactory long-term radiological and clinical outcomes with small incisions and minimal tissue damage. MIS techniques in THA can be performed with either a single incision or two incisions as introduced by Mears.3) Single-incision MIS techniques require an approximately 10 cm long incision and use either an anterior, anterolateral, or posterolateral approach. In contrast, two-incision MIS techniques use an anterior incision for acetabular cup placement and a posterior incision for femoral stem insertion to minimize tissue damage, enhance recovery, and shorten hospitalization.4-7) However, some authors are skeptical about MIS techniques in THA because of restricted visualization during surgery and the need for special equipment, which results in longer operative time and higher complication rates compared to the conventional surgical techniques.8-10) The purpose of this study was to investigate the safety and efficacy of the two-incision MIS technique by comparing ≥ 2 years of radiological and clinical results of a MIS THA using one incision about twice the diameter of an acetabular cup and a two-incision MIS THA introduced by Mears.3)
Fifty-six patients (60 cases) who had undergone either a single-incision or a two-incision MIS THA at our institution between December 2003 and September 2006 were reviewed retrospectively. Single-incision THA was performed using a posterolateral approach on 32 patients (34 cases) between December 2003 and August 2005, and two-incision TKA was performed on 24 patients (26 cases) between August 2005 and September 2006. Two-incision TKA was performed with informed consent of the patients. The cause of single-incision MIS TKA was avascular necrosis of the femur in 21 cases, osteoarthritis in 11 cases, and ankylosing spondylitis in 2 cases. The cause of two-incision MIS TKA was avascular necrosis of the femur in 20 cases and osteoarthritis in 6 cases. In seven patients who underwent bilateral TKA, single-incision TKA was performed on one side and two-incision TKA on the other. In the single-incision group, there were 21 males and 13 females, with a mean age of 61 years. In the two-incision group, there were 19 males and 7 females, with a mean age of 57.5 years. There were no statistical differences in age, gender, and cause for TKA between the groups. The mean follow-up period was longer in the single-incision group compared to the two-incision group at 58 months and 45 months, respectively.
For the single-incision technique, the patient was placed in the lateral decubitus position. A 10-cm skin incision proceeding distally from 1-2 cm proximal to the greater trochanter was made. The tensor fascia lata and gluteal fascia were also incised along the skin incision line. The external rotators were dissected over the greater trochanter, and the joint capsule was opened to expose the femoral neck. For the two-incision technique, the patient was placed in the supine position on a radiolucent operating table. A 5 to 6 cm long midline of the femoral neck was marked under fluoroscopy, and a skin incision was made. After identifying the lateral femoral cutaneous nerve, the fascia was incised, the tensor fascia lata was retracted laterally, and the sartorius and rectus femoris were retracted medially to expose the anterior joint capsule. The joint capsule was incised in line with the femoral neck. Two osteotomies were performed superior to the lesser trochanter, and the femoral neck fragment and the femoral head were removed. An acetabular cup was inserted after reaming (Fig. 1A-B). With the leg adducted, a 5-cm skin incision was made over the proximal greater trochanter, and the fascia lata was incised. The posterior joint capsule was incised via an anterior incision, a pathway to the posterior incision was made using a Kelly, and a fragment in the medial aspect of the greater trochanter was removed to perform femoral reaming in the neutral position. The femur was reamed and rasped through the posterior incision using fluoroscopy. At the same time, the depth of rasping and the presence of a fracture that was unobservable with fluoroscopy were checked by the naked eye through the anterior incision. A femoral stem and a femoral head were inserted through the posterior incision and the anterior incision, respectively, and reduction was performed (Fig. 1C-D).
The patients who underwent single-incision MIS TKA were classified into group I and those who underwent two-incision MIS TKA into group II. For clinical assessment, the mean operative time, intraoperative and postoperative blood loss, resumption of ambulation, hospitalization, and Harris hip score (HHS) were compared between the groups. For radiological assessment, the inclination angle and anteversion angle of the acetabular cup and ≥ 3° of varus or valgus angle between the femoral midline and the femoral stem measured on the postoperative and last follow- up radiographs were compared between the groups. The presence of periprosthetic fractures, infections, revision surgery, and dislocation were investigated in both groups.
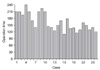
There was no significant difference in the mean body mass index between the groups, with 22.3 in group I and 21.6 in group II. The mean operative time was longer in group II at 163.8 minutes (± 38.1) compared to 118.2 minutes (± 17.7) in group I. The operative time in group II was significantly reduced after the first 15 cases (Fig. 2). There was no difference in the blood loss between the groups; the mean intraoperative blood loss was 586 cc (± 197) in group I and 581 cc (± 254) in group II, and the mean postoperative blood loss was 974 mL (± 465) in group I and 934 mL (± 473) in group II. Ambulation was started 5.3 days (± 1.98) after surgery on average in group I and 3.5 days (± 1.68) after surgery on average in group II, showing a statistically significant difference (p = 0.002). The mean hospitalization was 24.8 days (± 9.3) in group I and 15 days (± 6.8) in group II, showing a significant difference (p = 0.0001). No statistically significant difference was found in the mean HHS between the groups; the preoperative value was 50.8 in group I and 52.9 in group II, and the value at the last follow-up was 98.6 in group I and 94.3 in group II. Of the 7 patients who underwent single-incision MIS THA on one side and two-incision MIS THA on the other, 3 were satisfied with the single-incision THA and 4 with the two-incision THA in terms of postoperative pain and recovery, showing no statistically significant difference.
There was no significant difference in the mean abduction angle of the acetabular cup between the groups, with 42° (± 5.6) in group I and 43.8° (± 6) in group II. No significant difference was found between the groups in the mean acetabular cup anteversion angle, with 16.5° (± 5.8) in group I and 18.6° (± 7) in group II. More than 3° of deviation from neutral alignment was seen in 2 cases in group I and in 1 case in group II.
The incidence of intraoperative periprosthetic fracture was high at 4 cases (15%) in group II. Dislocation was not observed in either group. Revision surgery was performed in 2 cases from each group. The cause of the revision surgery was an infection in 1 case and a ceramic head fracture in the other case in group I and an infection in 1 case and severe leg length discrepancy in the other in group II. At the last follow-up, 2 cases of lateral femoral cutaneous neuropathy were observed in group II.
THA has taken another quantum leap with the introduction of MIS techniques, whose benefits compared to conventional methods include a small incision, minimal soft tissue damage, less pain and drug use, rapid return to activities of daily living, early rehabilitation, and short hospitalization.1,2,5) In our patients, ambulation was started 5.3 days after surgery on average in group I (single-incision MIS THA group) and 3.5 days after surgery on average in group II (two-incision MIS THA group). In the study by Yoon et al.,11) ambulation was started 1.5 days postoperatively on average after two-incision THA. The mean hospitalization was 24.8 days in group I and 15 days in group II in our study. All of the patients were discharged after suture removal on their own will without any pressure from the authors. In the study by Yoon et al.,11) the mean hospitalization was 9.4 days after single-incision THA and 8.4 days after two-incision THA. We found that MIS techniques promoted resumption of ambulation with a crutch and shortened hospitalization as well. Rehabilitation was especially rapid in group II. However, some studies have shown that two-incision MIS technique was not advantageous over other MIS techniques in terms of rehabilitation, because it caused more muscle damage that led to slow recovery.8,10,12)
MIS techniques necessitate significantly smaller skin incisions compared to conventional methods. The mean skin incision length was 10.9 cm in group I and 7.2 cm and 6.4 cm on the anterior and posterior side, respectively, in group II. Small incisions were related to high patient satisfaction in terms of cosmetic results.13) However, MIS techniques have also been associated with some problems. A large muscle incision may be unavoidable due to the poor intraoperative field of view limited by a small skin incision; severe retraction during surgery may cause more damage to the muscle and skin, and postoperative complication rates are high.8-10,14,15) In particular, muscular damage during femoral stem insertion through the posterior incision in two-incision MIS THA can be more severe compared to that in conventional THA or single-incision MIS THA.9,10) In this study, partial necrosis near the anterior skin incision caused by severe skin retraction was observed in the first case in group II, but it was not observed in the other cases where a longer skin incision was made during surgery. The anterior incision in two-incision MIS THA rarely caused musculature damage, because the joint capsule could be reached through the interval between two muscles. In the study by Yoon et al.,16) damage to the anterior muscles could be avoided with use of the Watson-Jones approach that allowed them to reach the joint capsule through the interval between the tensor fascia lata and the gluteus medius with the patient in the lateral decubitus position, and posterior incision made on the posterolateral aspect of the greater trochanter resulted in no damage to the adjacent muscles by using the piriform muscle as the anatomical landmark for incision. In this study, we could minimize musculature damage by incising the posterior joint capsule through the anterior incision, obtaining enough visualization of the medial side of the greater trochanter for rasping and separating the gluteus maximus muscle in the direction of the fibers with a Kelly. If necessary, the femoral implant was inserted through the posterior incision after posterior joint capsule incision and rasping to minimize muscular damage. Bal et al.17) and Bal and Lowe18) compared the results of conventional THA and two-incision MIS THA on MRI images and found that MIS resulted in minimal musculature damage, and there was no difference in the incidence of heterotopic ossification. Chou et al.4) showed that hip flexors are responsible for rapid rehabilitation after two-incision THA. Therefore, it is our understanding that two-incision THA does not necessarily result in significant muscular damage compared to the conventional methods. However, extensor muscle damage appeared to occur during surgery through the posterior incision, which should be addressed in further studies.
Another disadvantage of MIS is the long operation time. Tanavalee et al.19) reported that two-incision THA required long operation time and resulted in massive blood loss. In the study by Yoon et al.,11) there was no difference in the mean operation time between the conventional method and single-incision MIS, but it took 20 more minutes with two-incision MIS. In this study, the mean operation time was 163 minutes for the two-incision MIS, which was longer compared to 118.2 minutes for the single-incision MIS. Of the 26 cases of two-incision MIS, the surgery could be completed within two hours in only three cases. The operation time could be reduced by 20 minutes from the 16th case (p > 0.05). This was because, with additional experience, we could perform acetabular component insertion through the anterior incision without fluoroscopy and reduce dependence on it during femoral component insertion though the posterior incision. Archibeck and White20) and Bal et al.17) could reduce the operation time from the 10th to 15th case. Therefore, we think that two-incision MIS requires much education and experience for a surgeon to reduce the operation time. The operation time may be reduced when we experience more cases. Still, we think two-incision MIS has a longer learning curve compared to other methods. There was no difference in blood loss between the two groups.
Two-incision MIS has been associated with high complication rates.7,21,22) In this study, periprosthetic fractures were found in 4 (15%) of the first 10 cases. Once suspected, the presence of a periprosthetic fracture should be examined with the naked eye, because it may not be observed with intraoperative fluoroscopy. The fractures were fixated with wires that were passed through the anterior and posterior incisions. The crutch ambulation and rehabilitation program were the same as those for the patients without fractures and did not have a negative influence on the clinical outcomes.
Although MIS has a variety of benefits, we believe the priorities of THA include accurate fixation and insertion angle and prevention of dislocation and infection, without which a THA cannot be considered successful. The long-term survival of an implant, let alone the short-term results, should be the first thing to consider in using an MIS technique in replacement surgery. Accordingly, implants should be placed exactly in the planned site. In this study, the mean adduction angle and anteversion angle of the acetabular cup were not different between the groups. In addition, there was no statistically significant difference between the groups regarding the number of acetabular cups outside the safe zone (p = 0.2). Until the last follow-up, revision surgery was performed in 2 of the 26 cases in the two-incision group due to reasons that were not related to dislocation or loosening: 1 was for infection and the other one was for limping due to leg length discrepancy at the second postoperative year. The femoral component insertion site was not significantly different between the two groups. The mean HHS was satisfactory at 94.3 at 45 months after surgery in group II, indicating that the mid-term and long-term results of two-incision MIS would be satisfactory.
In conclusion, two-incision MIS was effective in promoting rapid rehabilitation and shortening hospitalization compared to single-incision MIS. However, due to unfamiliarity with the surgical technique and restricted visualization, the operation time was long and complication rates were high. Therefore, it is our understanding that some improvements should be made for the two-incision MIS introduced by Mears3) to be considered as a reliable surgical technique, and problems of the technique should be addressed in further studies.
Figures and Tables
References
1. Berger RA. Total hip arthroplasty using the minimally invasive two-incision approach. Clin Orthop Relat Res. 2003. (417):232–241.
2. Berger RA, Jacobs JJ, Meneghini RM, Della Valle C, Paprosky W, Rosenberg AG. Rapid rehabilitation and recovery with minimally invasive total hip arthroplasty. Clin Orthop Relat Res. 2004. (429):239–247.

3. Mears DC. Development of a two-incision minimally invasive total hip replacement. J Bone Joint Surg Am. 2003. 85(11):2238–2240.
4. Chou SW, Ueng SW, Lee MS. Muscular recovery of hip fl exors and extensors aft er two-incision total hip arthroplasty. Chang Gung Med J. 2008. 31(6):576–582.
5. Duwelius PJ, Burkhart RL, Hayhurst JO, Moller H, Butler JB. Comparison of the 2-incision and mini-incision posterior total hip arthroplasty technique: a retrospective matchpair controlled study. J Arthroplasty. 2007. 22(1):48–56.

6. Lu ML, Chou SW, Yang WE, et al. Hospital course and early clinical outcomes of two-incision total hip arthroplasty. Chang Gung Med J. 2007. 30(6):513–520.
7. Zhang XL, Wang Q, Shen H, Jiang Y, Zeng BF. Minimally invasive two-incision total hip arthroplasty: a short-term retrospective report of 27 cases. Chin Med J (Engl). 2007. 120(13):1131–1135.

8. Krych AJ, Pagnano MW, Wood KC, Meneghini RM, Kaufmann K. No benefit of the two-incision THA over miniposterior THA: a pilot study of strength and gait. Clin Orthop Relat Res. 2010. 468(2):565–570.

9. Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006. 453:293–298.
10. Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty: a randomized clinical trial. J Bone Joint Surg Am. 2008. 90(5):1000–1006.

11. Yoon TR, Park KS, Song EK, Seon JK, Seo HY. New two-incision minimally invasive total hip arthroplasty: comparison with the one-incision method. J Orthop Sci. 2009. 14(2):155–160.

12. Meneghini RM, Smits SA. Early discharge and recovery with three minimally invasive total hip arthroplasty approaches: a preliminary study. Clin Orthop Relat Res. 2009. 467(6):1431–1437.

13. Goldstein WM, Ali R, Branson JJ, Berland KA. Comparison of patient satisfaction with incision cosmesis aft er standard and minimally invasive total hip arthroplasty. Orthopedics. 2008. 31(4):368.

14. Fehring TK, Mason JB. Catastrophic complications of minimally invasive hip surgery: a series of three cases. J Bone Joint Surg Am. 2005. 87(4):711–714.
15. Feinblatt JS, Berend KR, Lombardi AV Jr. Severe symptomatic heterotopic ossifi cation and dislocation: a complication aft er two-incision minimally invasive total hip arthroplasty. J Arthroplasty. 2005. 20(6):802–806.

16. Yoon TR, Bae BH, Choi MS. A modifi ed two-incision minimally invasive total hip arthroplasty: technique and shortterm results. Hip Int. 2006. 16:Suppl 4. 28–34.

17. Bal BS, Haltom D, Aleto T, Barrett M. Early complications of primary total hip replacement performed with a two-incision minimally invasive technique. J Bone Joint Surg Am. 2005. 87(11):2432–2438.

18. Bal BS, Lowe JA. Muscle damage in minimally invasive total hip arthroplasty: MRI evidence that it is not signifi cant. Instr Course Lect. 2008. 57:223–229.
19. Tanavalee A, Jaruwannapong S, Yuktanandana P, Itiravivong P. Early outcomes following minimally invasive total hip arthroplasty using a two-incision approach versus a miniposterior approach. Hip Int. 2006. 16:Suppl 4. 17–22.

20. Archibeck MJ, White RE Jr. Learning curve for the two-incision total hip replacement. Clin Orthop Relat Res. 2004. (429):232–238.

21. Palutsis RS, Sheridan KC, Wasielewski RC. One surgeon's experience with the 2-incision technique for total hip arthroplasty. J Arthroplasty. 2010. 25(1):71–75.

22. Wetzel R, Dorsch M. Minimally invasive approach to implantation of a hip endoprosthesis. Orthopade. 2006. 35(7):738–743.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download