Abstract
Background
Detection of postoperative spinal cord level change can provide basic information about the spinal cord status, and electrophysiological studies regarding this point should be conducted in the future.
Methods
To determine the changes in the spinal cord level postoperatively and the possible associated factors, we prospectively studied 31 patients with scoliosis. All the patients underwent correction and posterior fusion using pedicle screws and rods between January 2008 and March 2009. The pre- and postoperative conus medullaris levels were determined by matching the axial magnetic resonance image to the sagittal scout image. The patients were divided according to the change in the postoperative conus medullaris level. The change group was defined as the patients who showed a change of more than one divided section in the vertebral column postoperatively, and the parameters of the change and non-change groups were compared.
Results
The mean pre- and postoperative Cobb's angle of the coronal curve was 76.80° ± 17.19° and 33.23° ± 14.39°, respectively. Eleven of 31 patients showed a lower conus medullaris level postoperatively. There were no differences in the pre- and postoperative magnitude of the coronal curve, lordosis and kyphosis between the groups. However, the postoperative degrees of correction of the coronal curve and lumbar lordosis were higher in the change group. There were also differences in the disease entities between the groups. A higher percentage of patients with Duchene muscular dystrophy had a change in level compared to that of the patients with cerebral palsy (83.3% vs. 45.5%, respectively).
Conclusions
The conus medullaris level changed postoperatively in the patients with severe scoliosis. Overall, the postoperative degree of correction of the coronal curve was higher in the change group than that in the non-change group. The degrees of correction of the coronal curve and lumbar lordosis were related to the spinal cord level change after scoliosis correction.
Surgical correction of scoliosis has become a more common procedure due to the continuous development of instruments and surgical procedures.1,2) A severe degree of deformity can now be corrected using pedicle screws and rods.3-5) There might be some postoperative change of the level of the spinal cord during the correction of a vertebral deformity.6,7) Detection of this postoperative change of the spinal cord level can provide basic information on the spinal cord status, and so this can encourage performing electrophysiological studies regarding this point. If there exist some postoperative level changes of the spinal cord after scoliosis surgery, then physicians have to pay attention to this phenomenon because this can cause some changes of the neurological status, even though these changes could be subclinical. Confirmation of this change will encourage performing neurophysiological studies on this subject. If there is significant level change, then the factors related to this phenomenon should be determined.
There have been several reports that have studied the spinal cord level of scoliosis patients using magnetic resonance imaging (MRI).8-13) Sun et al.12) measured the spinal cord level by comparing the conus tip level between subjects on sagittal magnetic resonance (MR) images. Although there was no significant difference in the distributions of the positions of the conus medullaris in the patients with adolescent idiopathic scoliosis (AIS) and the healthy controls, they successfully determined the conus tip level using MR images. We can assume that if there is some level change of the spinal cord during surgery, then the change of the level of the spinal cord can be detected by comparing the pre- and postoperative MR images. The detection of spinal cord level change can be important because it can provide a new concept that scoliosis surgery is a bony surgery as well as neurosurgery, and this surgery causes significant changes of the spinal cord level. However, measuring these changes is not easy partly because of the difficulty in identifying the level of the conus tip in severe scoliosis with the distorted sagittal images. In addition, a postoperative MRI assessment of the spinal cord is also difficult due to metallic artifacts. Ranger et al.14) reported that changes of the body position alter the location of the spinal cord within the vertebral canal. They determined the junction of the conus medullaris with the filum terminale on axial MR images to detect any changes of the spinal cord's location. Although they did not find significant cranio-caudal movement, they reported substantial movement of the conus medullaris using the axial MR images instead of the sagittal MR images. Rudisch et al.15) reported, by selecting specific instruments and MR pulse sequences, that postoperative MRI examinations could give acceptable results despite the presence of metallic artifact. Several authors have also tried to overcome the problem of metallic artifacts from orthopedic implants.15-18)
In this study, our aims were 1) to detect the spinal cord level change after scoliosis surgery using MRI with a useful method, 2) to determine the relationship between the spinal cord level change and the curve characteristics (the type of curve, the pre- and postoperative curve magnitude and the perioperative degree of correcting the curve), and 3) to determine the relationship between the spinal cord level change and etiologic factors (age, gender and the disease entity).
We prospectively studied 31 selected scoliosis patients who were scheduled for surgery from January 2008 to March 2009. The patients were 16 males and 15 females with an average age of 15.4 years (Table 1). The diagnoses included 14 patients with AIS, 11 patients with cerebral palsy (CP) and 6 patients with Duchenne muscular dystrophy (DMD). At first 37 scoliosis patients were enrolled in this study. However, those patients with a history of prior surgery and neurologic deficits were excluded at the first neurologic examinations. On the subsequent preoperative MR examinations, the patients showing the presence of thickening of the filum terminale or a conus tip level lower than L3 were excluded. In addition, the patients for whom the pre- or postoperative MR images made it difficult to evaluate the conus level, despite the specific MRI protocol, were excluded. Therefore, we excluded 6 of 37 patients who were not appropriate for our study.
All the patients underwent correction and posterior fusion using pedicle screws and rods. To correct the curvature, a rod derotation maneuver was performed for all the patients. To minimize the difference between the correction maneuvers, we performed only the derotation method in this study. During the surgery, transcranial electrical stimulation motor-evoked potential monitoring was performed (TES-MEP; Nims Spinal System, Medtronic-Sofamor Danek, Memphis, TN, USA). Titanium screws and rods were used for surgery to minimize the metallic artifacts. The subjects underwent whole-spine anteroposterior (AP) and lateral radiography and MRI of the spine both pre- and postoperatively. From the T11 to L3 vertebrae, the axial MR images through the vertebral bodies were made with a 1.5-mm thickness and a 3-mm gap between the slices.19) The turbospin-echo pulsed sequence (repetition time, 3,600; echo time, 100; bandwidth, 180; acquisition time, 3 minutes; echo train length, 16; field of view, 140 × 141; flip angle, 180) and the T2-weighted images were obtained during the study. The axial images were plotted off a sagittal midline T2-weighted image from T11 to L3, and these axial images were parallel to the each disc level. The axial cutting level was drawn automatically on a computer workstation on the sagittal midline T2-weighted image (the scout image). The serial axial MR images were used to determine the precise conus tip level. Of these images, the one showing the most evident loss of conus configuration was selected to match up with the sagittal scout image. The tip of the conus was defined as the most distal point of the cord that showed an equal or smaller diameter compared to the adjacent nerve fibers of the cauda equina (Fig. 1). On the sagittal scout image, each vertebra/disc unit was divided into three equal portions (upper, middle, lower), and the distal intervertebral disc was defined as a separate region (Fig. 2).11) In addition, the level of the conus tip in relation to the adjacent vertebra and disc space was determined.
The patients' height and trunk length were measured for comparison with the vertebral length. The length of the vertebra and disc space that were located at the conus tip level were measured in each patient. All the magnetic resonance images were reviewed by two authors (JYH, HNM) on a computer workstation (PiViewStar, Infinit, Seoul, Korea), which allowed for easy and accurate determinations. The MR images were provided to two independent observers without any markings regarding the patients' information. The interobserver reliability was calculated as 0.942 (CI, 0.912 to 0.961) and the mean absolute difference was calculated as 1.23 mm between the two observers. For statistical analysis, the patients were divided into the change and non-change groups. The change group was defined as patients showing a change of more than one divided section in the conus medullaris level postoperatively (Figs. 3 and 4). We compared the parameters regarding age, gender, the type of curve, the disease entities, the pre- and postoperative magnitude of the coronal and sagittal curves and the postoperative degree of correcting the coronal and sagittal curves. Thoracic kyphosis was measured between the upper endplate of the T1 vertebra and the lower endplate of the T12 vertebra, and lumbar lordosis was measured between the upper endplate of the L1 vertebra and the lower endplate of the L5 vertebra, as assessed by Cobb's method. The coronal curve was defined as the largest curve on the AP radiography. The absolute value was used to compare the pre- and postoperative curve severity of lordosis and kyphosis. SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis.
The mean length of the vertebra was 21.84 mm (range, 19.12 to 22.54 mm) and that of the disc space was 6.98 mm (range, 6.55 to 7.12 mm). Therefore, in this study, one divided section was approximately more than 6 mm and it was larger than the mean absolute difference between the observers. The mean vertebra/height ratio and the mean vertebra/trunk ratio were 0.0137 (range, 0.0129 to 0.0171) and 0.0244 (range, 0.0213 to 0.0296), respectively, which were similar between the patients (p > 0.05). Preoperatively, the conus tip was located between the T12-L1 disc space and the middle area of the L2 vertebra in 31 patients. We observed no change in the postoperative level of the conus medullaris in 20 patients, and there was a difference of more than one divided section in 11 patients. All 11 patients showed a lower conus medullaris level equal to 1/3 to 2/3 the height of a vertebra. One patient with AIS, 5 patients with CP and 5 patients with DMD exhibited a level change of the conus tip. In these patients, the conus tip was located between the L1 upper body and the L2 lower body area postoperatively (Table 1).
According to the type of main curve, there were 11 thoracic, seven thoracolumbar and 13 lumbar curves and there was no difference (p > 0.05) of the curve type between the change and non-change groups. There were no differences (p > 0.05) in the preoperative and postoperative magnitudes of the coronal curve, kyphosis, and lordosis between the 2 groups (Table 2). The postoperative degree of correction of the coronal curve was higher (p < 0.0001) in the change group than that in the non-change group (59.54° vs. 36.30°, respectively). In addition, the degree of correction of the lumbar lordosis was higher (p < 0.0001) in the change group (45.18° vs. 8.75°, respectively). However, the degree of correction of the thoracic kyphosis was similar (p > 0.05) in both groups.
A higher percentage (p = 0.003) of patients with DMD had a change in the spinal cord level as compared with that of the patients with CP (83.3% vs. 45.5%, respectively) (Table 3). However, the patients' age and gender were similar (p > 0.05) in both these groups. The perioperative degree of correction of the coronal curve was higher in the patients with DMD than that in those patients with CP and AIS (58.67°, 43.91°, and 39.00°, respectively; p = 0.027). In addition, the degree of perioperative correction of lordosis was higher in the patients with DMD than that in those patients with CP and AIS (48.17°, 21.00°, and 10.86°, respectively; p < 0.0001). However, the pre- and postoperative curve magnitude was similar between the disease groups (p > 0.05).
In this study, we could not measure the real spinal cord length, and the spinal canal length should be measured to detect the change of the spinal cord level. However, scoliosis is not a simple coronal deformity. It is a 3-dimensional (3D) deformity that includes coronal, sagittal and axial deformity. The maximal magnitude of curvature can be changed in another 3D plane. We think that if we want to accurately measure the real spinal canal length, we have to develop a new 3D radiographic measure device, or directly measure the length using thread in a cadaveric model. Therefore, we applied the MR conus tip model instead of measuring the real canal length to detect the relative spinal cord level change. In this study, the 31 patients had a mixture of diagnoses. There may be a difference between thoracic scoliosis patients and lumbar scoliosis patients, and differences have been shown between the AIS patients and the neuromuscular disease patients. To minimize this effect, we measured the coronal as well as sagittal magnitude of curvature, and we found that the amount of changed magnitude of curvature has an influence on the conus location regardless of the diagnosis. Although there could be factors for each diagnosis group that determine the conus level pre- and postoperatively, we focused on the general magnitude of the coronal and sagittal correction. In addition, we had tried to compare the level change between the disease groups. There was a difference between the disease groups; however, we could not confirm the influences of the conus tip level change according to the nature of the disease because the number of patients was relatively small in each of the disease groups.
Saifuddin et al.20) reported the conus position by introducing the concept of the vertebra/disc unit to measure the conus tip position. They measured the conus medullaris level on the sagittal images. However, it is clinically difficult to determine the conus medullaris level on the sagittal MR image in patients with severe scoliosis. Furthermore, on the postoperative MR images, the long sagittal image shows artifacts that are too intense to determine the conus level. Therefore, this study used the axial MR images and the sagittal scout images. In this study, the conus tip was determined on the axial MR images when the conus diameter was equal to or smaller than the other nerve fibers.14) By a serial examination of the axial MR images matched with the sagittal scout image, we could determine the precise level of the conus medullaris tip. In addition, the useful postoperative MRI settings were employed to minimize the artifacts. In addition to the intraoperative use of titanium implants, all the patients underwent T2-weighted turbo spin-echo imaging using a 1.5-T MRI system to minimize the artifacts made by implants.15-18) The precise conus tip level could be determined using these methods. In this study, we found a useful protocol for evaluating the spinal cord under specific conditions, such as the operated and deformed spine. We evaluated the postoperative spinal cord level change in patients with scoliosis of different severity and etiology. Substantial spinal cord level change was found in 11 patients. Although the normal spinal cord is held in position by the dentate ligaments, the nerve roots and filum terminale, cadaveric and in vivo MRI studies have shown that the cord is stretched by as much as 10%. While the dentate ligament and each nerve root act to stabilize the spinal cord, they do not appear to prevent spinal cord movement.2,10) The movement of the spinal cord is determined by the balance between the forces pulling the cord via the cord itself with its attachment to the brain and the forces pulling the cord caudally via the filum terminale, the lumbosacral nerve roots and possibly the dentate ligaments.21) In this study, the conus tip moved downward, but no patient complained of neurologic deficits postoperatively. Although pre- and postoperative neurophysiologic evaluation is needed to confirm the patient's neurologic status, this study suggests some concepts when performing corrective surgery forscoliosis. The direction of movement after correction was downward. Moreover, downward movement equal to 1/3 or 2/3 of the patients' vertebral height does not cause neurologic problems. Although the clinical relevance was not confirmed and this should be evaluated in the future, surgeons should consider the possibility of postoperative spinal cord level change.
In this study, the perioperative correction angles of the coronal and sagittal curves were different between the change and non-change groups. The degrees of correction of the coronal curve and lumbar lordosis were higher in the change group. It appears that a large amount of correction in surgery might decrease the cranial tethering force and move the conus caudally. The important factor is not the initial or final curve severity, but the perioperative correction angle. In addition to the correction of the coronal plane, the sagittal correction is important because scoliosis is a three-dimensional deformity. In this study, there was more correction of the lumbar deformity than the thoracic deformity in the change group (45.18° ± 15.79° vs. 9.64° ± 6.87°, respectively). It appears that for correction of the sagittal plane curves, the lumbar lordosis might be a more important factor affecting the movement of the spinal cord. Chu et al.8) reported relative shortening and functional tethering of the spinal cord in patients with AIS. Many researchers have found reduced spinal cord to vertebral column ratios in the AIS patients with severe curves, suggesting a disproportional growth between the skeletal and neural systems.8-10,12,13,22) We can assume that in severe scoliosis, the tethered cord can be released by a significant degree of correction, and that caused the postoperative spinal cord level change. The uncoupled neuro-osseous growth theory has not yet been confirmed. Chu et al.8) found longer spinal column to cord ratios only in the severe cases of scoliosis and not in the mild cases, and this hypothesis can provide a clue to how the spinal cord level changes postoperatively. We assumed patients with scoliosis or lordosis had a longer spinal column length due to the curvature, and there was a relative stretching of the cord, which can migrate the cord upward. If the scoliosis or lordosis is substantially corrected, then the length of the spinal column can be decreased. Therefore, downward migration of the cord was noticed in patients who had a large amount of correction, following the decrease of the upward tethering force. Clinically, in the surgery for scoliosis, we usually fix an appropriate-sized rod to each screw before the correction maneuver. However, after the correction maneuver, the length of the rod becomes longer in severe scoliosis and it often needs to be cut. It appears the spinal column length becomes shorter after correction and the rod moves downward. The spinal cord lies on the concavity of a long lordotic, scoliotic bow. If the curved spinal column is straightened, then the spinal cord also moves more to the center of the spinal column and it will go downward.
We observed no differences in gender and age between the change and non-change groups. However, the disease entities of the patients were different: five of the six patients with DMD (83.3%) and five of the 11 patients with CP (45.5%) were in the change group. However, only one of the 14 patients with AIS (7.1%) was in the change group. It appears that we can we can anticipate spinal cord movement when performing corrective surgery for neuromuscular scoliosis patients. In this study, we found a relationship between disease and the cord level change. However, the number of patients was relatively small. The perioperative degree of correction of the coronal and sagittal curve was higher in the patients with DMD. Therefore, we cannot confirm the relationship between disease entities and spinal cord level change. The scoliosis of patients with DMD often shows flexible long C-shaped coronal curves and sagittal hypolordosis.23-25) In this study, we also found these characteristics of curves in patients with DMD. Therefore, the perioperative correction angle might be higher in the flexible coronal and sagittal curves of the patients with DMD and five of these six patients were in the change group. Further study is warranted in a large population to evaluate the relationships between disease entities and spinal cord movement.
In conclusion, we found the conus medullaris level changed postoperatively in patients with severe scoliosis. The spinal cord level changed after a large amount of correction. The degree of correction of the coronal curve and lumbar lordosis was associated with spinal cord level change. We could found no clinical relevance for the postoperative conus medullaris level changes that warrants a neurophysiologic study. However, this study provides some clues about the perioperative changes in the spinal cord. Correction surgery in scoliosis is a bony procedure that corrects the distorted spine and it is also a neurosurgical procedure that includes a substantial level change of the spinal cord in the canal. Electrophysiological studies regarding this point should be conducted. Substantial level change of the spinal cord is an important concept for surgeons who perform scoliosis surgery.
Figures and Tables
Fig. 1
The serial axial magnetic resonance images show the loss of the conus configuration. The tip of the conus was defined as the most distal point of the cord that could be visualized. The images show (A) the conus body, (B) the conus tip and (C) the cauda equina.

Fig. 2
The sagittal magnetic resonance image shows each vertebra/disc unit, which was divided into three equal portions (upper, middle, lower), and the intervertebral disc.

Fig. 3
The preoperative (A) anteroposterior (AP) and (B) lateral radiographs of a 15-year-old male patient show a Cobb angle, lordosis and kyphosis of 68°, 37°, and 41°, respectively. The postoperative (C) AP and (D) lateral radiographs show a Cobb angle, lordosis and kyphosis of 20°, 32°, and 29°, respectively. The conus tip was identified on the axial magnetic resonance (MR) image and the location was determined by comparing this image with the sagittal scout image. The preoperative (E) sagittal and (F) axial MR images and the postoperative (G) sagittal and (H) axial MR images show the conus tip is located at the L1-L2 disc space.

Fig. 4
The preoperative (A) anteroposterior (AP) and (B) lateral radiographs of a 23-year-old female patient show a Cobb angle, lordosis and kyphosis of 93°, -15°, and 38°, respectively. The postoperative (C) AP and (D) lateral radiographs show a Cobb angle, lordosis and kyphosis of 36°, 26°, and 37°, respectively. The conus tip was identified on the axial MR image, and the location was determined by comparing this image with the sagittal scout image. The preoperative (E) sagittal and (F) axial MR images and the postoperative (G) sagittal and (H) axial MR images show the conus tip is located at the upper L1 body preoperatively and at the lower L1 body postoperatively.
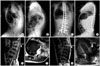
Table 1
Summary of All the Patients' Parameters

Dz: disease, Cur: curve type, Pre: preoperative, Post: postoperative, Corr: postoperative correction degree, Du: duchene muscular dystrophy, I: adolescent idiopathic scoliosis, C: cerebral palsy, TL: thoraco-lumbar, L: lumbar, T: thoracic, D: disc space, U: upper body of vertebra, M: middle body of vertebra, L: lower body of vertebra.
References
1. Lehman RA Jr, Lenke LG, Keeler KA, et al. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine (Phila Pa 1976). 2008. 33(14):1598–1604.

2. Steinmetz MP, Rajpal S, Trost G. Segmental spinal instrumentation in the management of scoliosis. Neurosurgery. 2008. 63:3 Suppl. 131–138.

3. Lenke LG, O'Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM. Posterior vertebral column resection for severe pediatric deformity: minimum two-year follow-up of thirty-five consecutive patients. Spine (Phila Pa 1976). 2009. 34(20):2213–2221.
4. Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine (Phila Pa 1976). 2005. 30(18):2061–2067.
5. Suh SW, Modi HN, Yang J, Song HR, Jang KM. Posterior multilevel vertebral osteotomy for correction of severe and rigid neuromuscular scoliosis: a preliminary study. Spine (Phila Pa 1976). 2009. 34(12):1315–1320.

6. Reid JD. Effects of flexion-extension movements of the head and spine upon the spinal cord and nerve roots. J Neurol Neurosurg Psychiatry. 1960. 23(3):214–221.

7. Yuan Q, Dougherty L, Margulies SS. In vivo human cervical spinal cord deformation and displacement in flexion. Spine (Phila Pa 1976). 1998. 23(15):1677–1683.

8. Chu WC, Lam WW, Chan YL, et al. Relative shortening and functional tethering of spinal cord in adolescent idiopathic scoliosis Study with multiplanar reformat magnetic resonance imaging and somatosensory evoked potential. Spine (Phila Pa 1976). 2006. 31(1):E19–E25.
9. Chu WC, Man GC, Lam WW, et al. Morphological and functional electrophysiological evidence of relative spinal cord tethering in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2008. 33(6):673–680.

10. Porter RW. The pathogenesis of idiopathic scoliosis: uncoupled neuro-osseous growth? Eur Spine J. 2001. 10(6):473–481.

11. Roth M. Idiopathic scoliosis caused by a short spinal cord. Acta Radiol Diagn (Stockh). 1968. 7(3):257–271.

12. Sun X, Chu WC, Cheng JC, et al. Do adolescents with a severe idiopathic scoliosis have higher locations of the conus medullaris than healthy adolescents? J Pediatr Orthop. 2008. 28(6):669–673.

13. Sun X, Qiu Y, Zhu Z, et al. Variations of the position of the cerebellar tonsil in idiopathic scoliotic adolescents with a cobb angle > 40 degrees: a magnetic resonance imaging study. Spine (Phila Pa 1976). 2007. 32(15):1680–1686.

14. Ranger MR, Irwin GJ, Bunbury KM, Peutrell JM. Changing body position alters the location of the spinal cord within the vertebral canal: a magnetic resonance imaging study. Br J Anaesth. 2008. 101(6):804–809.

15. Rudisch A, Kremser C, Peer S, Kathrein A, Judmaier W, Daniaux H. Metallic artifacts in magnetic resonance imaging of patients with spinal fusion: a comparison of implant materials and imaging sequences. Spine (Phila Pa 1976). 1998. 23(6):692–699.

16. Chang SD, Lee MJ, Munk PL, Janzen DL, MacKay A, Xiang QS. MRI of spinal hardware: comparison of conventional T1-weighted sequence with a new metal artifact reduction sequence. Skeletal Radiol. 2001. 30(4):213–218.

17. Lee MJ, Kim S, Lee SA, et al. Overcoming artifacts from metallic orthopedic implants at high-field-strength MR imaging and multi-detector CT. Radiographics. 2007. 27(3):791–803.

18. Petersilge CA. Evaluation of the postoperative spine: reducing hardware artifacts during magnetic resonance imaging. Semin Musculoskelet Radiol. 2000. 4(3):293–297.

19. Stradiotti P, Curti A, Castellazzi G, Zerbi A. Metal-related artifacts in instrumented spine. Techniques for reducing artifacts in CT and MRI: state of the art. Eur Spine J. 2009. 18:Suppl 1. 102–108.

20. Saifuddin A, Burnett SJ, White J. The variation of position of the conus medullaris in an adult population. A magnetic resonance imaging study. Spine (Phila Pa 1976). 1998. 23(13):1452–1456.

21. Chu WC, Lam WM, Ng BK, et al. Relative shortening and functional tethering of spinal cord in adolescent scoliosis: result of asynchronous neuro-osseous growth, summary of an electronic focus group debate of the IBSE. Scoliosis. 2008. 3:8.
22. Porter RW. Idiopathic scoliosis: the relation between the vertebral canal and the vertebral bodies. Spine (Phila Pa 1976). 2000. 25(11):1360–1366.
23. Hahn F, Hauser D, Espinosa N, Blumenthal S, Min K. Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J. 2008. 17(2):255–261.

24. Manzur AY, Kinali M, Muntoni F. Update on the management of Duchenne muscular dystrophy. Arch Dis Child. 2008. 93(11):986–990.

25. Modi HN, Suh SW, Yang JH, et al. Surgical complications in neuromuscular scoliosis operated with posterior-only approach using pedicle screw fixation. Scoliosis. 2009. 4:11.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download