Abstract
Background
Some dysplastic hips with favorable radiographic parameters fail to develop normally, suggesting that we should consider cartilaginous or soft tissue structures for further information regarding the condition of the hip. The purpose of this study was to provide a clear definition of concentric reduction in developmental dysplasia of the hip (DDH) based on magnetic resonance imaging (MRI), and to determine how radiographic and MR-based parameters could be used together to treat dysplastic hips.
Methods
We studied range of motion (ROM)-MRI of 25 patients with unilateral hip dysplasia (mean age at the time of MR imaging, 44.1 months). Each ROM-MRI consisted of a set of bilateral hip scans in the following positions: neutral; abduction; abduction- internal rotation; abduction-internal rotation-flexion; and adduction. Before MR scanning, the 25 patients received the following primary treatments: closed reduction (n = 15; at a mean age of 14.5 months); and open reduction (n = 10; at a mean age of 10.0 months). The following new parameters appear to be useful in treating DDH: 1) the labral angle, the angle the labrum makes with the acetabulum; 2) the uncorrected labral deformity (ULD), the "residual deformity" (deflection of the labrum) when the affected labrum is freed from pressure in abduction; and 3) the zone of compressive force (ZCF), the region of the acetabulum through which the body weight acts on the femoral head.
Results
A concentrically-reduced hip is one in which the labrum points downward in the neutral position, at the same angle as that of the normal side; and in which the ZCF is zone 3, the inner acetabular zone as defined herein. The ULD and the ZCF may be determined precisely as we have done, or the physician may simply observe the changes in the orientation of the labrum and compare the changes qualitatively to the unaffected side, and likewise for the medial joint space.
Although many radiologic parameters, such as the acetabular index (AI),1-4) the center-edge angle (CEA),5) the center-head distance discrepancy (CHDD),6) Smith's c/b and h/b ratios,7) and the amount of femoral head coverage (HC),8) have been proposed to indicate the degree of hip dysplasia, none of the radiologic parameters (either singly or in combination) accurately predicts acetabular development in all cases. For example, Chen et al.6) reported that 96% of hips with a CHDD ≤ 6% had satisfactory results, whereas hips with a CHDD > 6% had 78% unsatisfactory results. Similarly, Kim et al.9) divided patients into four groups based on the CHDD values and the orientation of the sourcil, and reported satisfactory results in 19 of 20 hips (95%) with a CHDD < 6% and horizontal sourcils, while 4 of 5 hips (80%) with a CHDD < 6% and upward sourcils had unsatisfactory results; 8 of 9 hips (88.9%) with upward-oriented sourcils had unsatisfactory results. These studies confirm that while CHDD and AI are important predictors of residual dysplasia, CHDD and AI fail to account for up to 20% of outcomes. Additionally, the often-stated goal of "concentric reduction" of the hip has never been precisely defined.
To overcome these shortcomings of radiograph-based management of hip dysplasia, it seems reasonable to look to soft tissue and/or cartilaginous structures for clues to other avenues of treatment. As the labrum is well-known to have an important role in the growth of the acetabulum,10-17) it is an obvious place to begin. Therefore, we initiated a study using MR imaging of dysplastic hips with emphasis on the labrum to answer or clarify the following questions: 1) What is the usual range of labral angles in normal and dysplastic hips?, 2) What is meant by concentric reduction of the hips?, and 3) How can radiographic and MR-based parameters be used together in managing developmental dysplasia of the hip (DDH)?
Twenty-five range of motion (ROM)-magnetic resonance imagings (MRIs) (one each for 25 patients) were selected for this analysis. ROM refers to range of motion because the images were taken in the following positions: neutral; abduction; abduction-internal rotation; abduction-internal rotation-flexion; and adduction. The criteria for selection of patients and MRI were: 1) unilateral hip dysplasia after closed reduction or open reduction without previous bony surgery in the femur and pelvis; and 2) a clear ROM-MRI, which showed the labrum, articular cartilage, and surrounding soft tissues in all five positions of both hips. All of the dysplastic hips studied had one or more of the following on radiographs: AI ≥ 25°; CHDD ≥ 6%; subluxation; a widened medial or superior joint gap; or an upward-oriented lateral sourcil.9)
Before ROM-MRI, our 25 patients had 2 types of hip dysplasia (dislocation, 21 hips; subluxation, 4 hips). Fifteen hips received non-surgical treatment (Pavlik harness, 2 hips; abduction brace, 3; closed reduction, 10) and 10 hips were treated surgically (open reduction). All surgical procedures were performed at our institution by the senior author. Interposed ligamentum teres and soft tissues were excised and the labrum was preserved. Each patient also required two or three periods of hip spica cast immobilization after arthrographic evaluation. The mean patient age at the time of primary treatment was 10.0 months (range, 4 to 18 months) in the closed reduction group and 14.5 months in the open reduction group (range, 12 to 16 months), while the mean age at the time of MR imaging was 44.1 months (range, 22 to 88 months). There were 22 females and 3 males; involvement was on the left side in 18 and the right in 7.
All MRI scans were performed on a 1.5-T imaging unit (Magnetom Sonata; Siemens, Erlangen, Germany). Three consecutive T2-weighted coronal scans of the anterior, middle, and posterior parts of the hip joint were made in each of five positions: neutral; abduction; abduction-internal rotation; abduction-internal rotation-flexion; and adduction. Our reliance on T2-weighted scans reduced the conventional scanning time and minimized the time that young children had to remain in the MRI scanner. The scanning time for each position was approximately 4 minutes. In a T2-weighted image, the articular cartilage and the muscle have an intermediate signal intensity, while the labrum has low intensity and is triangular. Due to the abnormal accumulation of fluid in a subluxated hip, the widened joint space shown on the radiograph is an area of high intensity between the femoral head and the acetabulum.
Initially we used a specially designed foot holder which rested on the main operating MRI table and slid into the bore of the magnet. The foot holder consisted of a main frame with specially made shoes for the left and right feet. However, as the study progressed, it was found easier for the examiner to manually change the position of the patient's feet for each scan. Younger children were sedated, while explanation of the scanning procedure was helpful in obtaining the cooperation of older children without sedation.
In each case the abduction angle was made as large as possible, but it was limited by the size of the child and the 60-cm bore diameter of the machine; mean abduction angle was 22.7° (range, 9 to 44°). In adduction, the affected leg was adducted about 15° and rested under the normal leg. Internal rotation and flexion were about 15°.
We define LA as the angle which the labrum makes with the acetabulum (Fig. 1). The labral angle is a direct reflection of the degree of concentric reduction of the hip joint. When the femoral head pushes upward on the labrum (causing high values of AI and CHDD in radiographs), the labrum has a more horizontal position than it would normally. Thus, the labral angle is usually higher in the affected (dysplastic) side than in the unaffected side. The LA normally decreases (that is, the labrum moves downward) in the unaffected side as the hip moves from neutral to abduction and increases as the hip moves from neutral to adduction.
In many dysplastic hips the labrum is less elastic than normal, and in abduction the labrum does not return to the normal position (the angle of the labrum on the unaffected side). For that reason, we define the ULD as the difference between the LA of the affected hip in abduction and the LA of the unaffected hip in the neutral position to measure the amount of uncorrected or "residual" deformation of the labrum in the affected hip. If the value of the ULD is close to 0°, the position of the labrum in the affected hip is similar to that of the unaffected hip in neutral. Therefore, the labrum has sufficient elasticity to return to a normal position in abduction.
If the value of ULD is > 0°, the labrum is deformed even when there is no pressure from the femoral head, and more information is needed to evaluate the condition of the hip and the proper treatment.
As a way of confirming the novel information content of the new parameter ULD, we measured the AI and CHDD from radiographs and the ULD from MRI for all of our patients, and defined patient groups based on these parameters, then looked for agreement between the groups thus defined. Little agreement would be interpreted to mean that AI and CHDD do not reflect the condition of the labrum, thus supporting the need for the new parameter (ULD). Radiographs and MRI used for this purpose were taken within 1 week of each other.
The new parameter, ZCF, is used to represent the amount of lateralization of the femoral head (as does CHDD in radiographs). ZCF (Fig. 2) was determined to evaluate the affected hip in relation to the compressive forces acting on it. According to Pauwells,18) the resultant force of the partial body weight and the abductor muscle group will act in a downward and lateral direction, 16° off the vertical line. In a normal hip, the ZCF is zone 3 in the neutral position and abduction; in a dysplastic hip, the ZCF shifts from zone 2 in the neutral position to zone 3 in abduction, or zone 2 in both positions. The ZCF, along with the change in the LA, facilitated visualization of the degree of reduction of the femoral head.
All ROM-MR image data and radiographs were stored in the picture archiving and communication system (PACS; Marosis m-view™ 4.5, Marotech Inc., Seoul, Korea) which provides measurement tools, such as a ruler and goniometer, on the monitor. All parameters were measured 3 times on the 19-inch monitor, then averaged.
The significance of differences in measured parameters between the affected and unaffected hips was analyzed with the Mann-Whitney U-test. The Wilcoxon signed-rank test was used for comparing parameters between hip positions. The agreement between patient groups defined by criteria from radiographs (AI and CHDD) and from ROM-MRI (ULD) was tested in two ways (the simple [unweighted] kappa value and Fisher's exact test). All analyses were performed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). p-values < 0.05 were considered statistically significant.
Parameter values in the abduction-internal rotation and abduction-internal rotation-flexion positions did not differ significantly from the parameter values in abduction; thus, the former are omitted from this analysis.
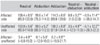
Table 1 gives the values we obtained for LA on the normal and affected sides in the neutral, abduction, and adduction positions when all 25 patients were considered together. In the neutral position, the mean LA of the affected hips was significantly higher than the mean LA of the unaffected hips. Moving from neutral to abduction, the labrum moved downward by a mean of 8.8° and 3.5° in the affected and unaffected hips, respectively. When the hips moved from neutral to adduction, the labrum moved upward by a mean of 5.9° on the affected side, and by a mean of 3.2° on the unaffected side. We believe that the LA changes more on the affected side due to the instability of the joint.
As for ULD, a mean LA of 99.6° in abduction on the affected side was 3.4° smaller than the mean LA of 103.0° of the unaffected side in the neutral position, meaning the mean ULD of our patients was quite favorable. Our 25 affected hips showed the following values of ULD: ULD ≤ 0°, 17 hips; 0° < ULD ≤ 5°, 6 hips; 5° < ULD ≤ 10°, 1 hip; and 10° < ULD ≤ 15°, 1 hip. Thus, 17 (68%) of our affected hips showed "normal" labral elasticity, while 8 (32%) showed residual labral deformity.
Statistically, the agreement between patient groups defined by AI and ULD was shown to be low, as with CHDD and ULD (Table 2). This was true whether or not we considered each of the 4 radiographic groups separately, as in Table 2, or together (first, by AI value alone, as AI ≥ 25° vs. AI < 25°, or by CHDD value alone, as CHDD ≥ 6% vs. CHDD < 6%). This shows that the radiographic parameters AI and CHDD do not closely reflect (or correspond to) the amount of uncorrected labral deformity.
In 10 of the 25 hips (40%), the ZCF shifted from zone 2 in the neutral position to zone 3 in abduction. In the other 15 hips, the ZCF did not change on abduction; the ZCF continued as zone 2 in 8 (32%), and as zone 3 in 7 (28%) hips. In all unaffected hips, the ZCF continued as zone 3 in abduction. Therefore, 17 hips (68%) showed normal reduction of the femoral head into the inner region of the acetabulum in abduction.
As the affected hips moved from the neutral position to adduction, the ZCF shifted from zone 3 to zone 2 in 6 hips and from zone 2 to zone 1 in 2 hips. In the other 17 hips, the ZCF continued as zone 2 in 11 hips and zone 3 in 6. On the normal side, the ZCF continued as zone 3 in 15 hips and zone 2 in 2, while the ZCF shifted from zone 3 to zone 2 in 8. Therefore, in adduction the ZCF was located in the outer region in 19 of the 25 affected hips (76%), but in only 10 of the 25 unaffected hips (40%).
Based on parameters measured from ROM-MRI, we define a concentrically-reduced hip as one in which the affected labrum points downward in the neutral position, at the same angle as the labrum of the normal hip; and in which the ZCF in the neutral position is zone 3 as defined herein (and shown in Fig. 2). For concentric reduction of the femoral head in a dysplastic hip, the LA in hip abduction should be similar to that of the unaffected side in neutral (ULD ≤ 0°) and the medial joint space should be decreased (ZCF moves from zone 2 in neutral to zone 3 in abduction).
MR imaging as the hip moves through a range of positions makes it easy to follow the changes in the cartilage and soft tissues, especially the labrum, which has such an important role in the growth of the acetabulum.10-17) As the hip moves from the neutral position to abduction, if the labrum moves downward (that is, if the LA decreases) from a relatively horizontal position, any treatment must reduce the pressure on the labrum (with an abduction brace or a varus-[derotation] osteotomy of the proximal femur), and/or must orient the labrum downward in the normal direction (by a pelvic osteotomy), to facilitate the lateral and downward growth of the lateral part of the acetabulum and its deepening.
Regarding the ULD, our rationale for comparing the LA of the affected hip in abduction with that of the normal hip in the neutral position is that in abduction we see the affected hip when it is freed from pressure and its reduced elasticity is most visible, while on the normal side the position of most importance is the neutral. The ULD is, simply an approximate measure of the amount of correction we would like to achieve by treatment; thus, it does not figure in our definition of concentric reduction.
It could be argued that the ZCF, as here defined, is another measure of lateralization, but a crude one at that. The important point is that the ZCF is a simple guideline obtained from ROM-MR images. The widened joint space visible on radiographs is often confirmed by MRI to be filled with fluid. The femoral head is shifted laterally to a biomechanically disadvantaged position and the ZCF can shift medially in abduction. However, ROM-MRI sometimes reveals that a widened joint space in the radiograph is occupied by a hypertrophied articular cartilage, and is accompanied by a shallow acetabulum with poor head coverage. In such cases, the ZCF does not shift medially in abduction. A V-shaped tear-drop in the radiograph, with a widened superior portion and a thickened acetabular floor, is indicative of residual acetabular dysplasia19) and a reconstructive procedure should be considered.20)
Given the priority we place on rather small changes in the labral angle and the ZCF, we should acknowledge the possibility of intra- or inter-observer error in determining these parameters. Fortunately, the downward or upward shift of the labrum, and the change in acetabular zone, are generally unambiguous and easy to visualize, even without precise measurement or drawing.
It is very difficult to measure the elasticity of the deformed labrum because the biomechanical properties have been changed by the severity and duration of dislocation of the femoral head. Therefore, even after treatment by abduction brace or varus-(derotation) osteotomy of the proximal femur, we cannot predict at what time in the future the ULD will be normalized. However, the return of the labrum to a normal shape and direction is a prerequisite for normal development of the acetabulum, ether by conservative or surgical treatment. A persistently increased LA suggests a high probability of acetabular dysplasia.
Our goal in treating dysplasia is to have a normal hip as early as possible after primary treatment, even before 4-5 years of age,9,20-24) allowing up to 1-2 years following reduction for the acetabular index to return to normal (< 25°). Based on reviews of our patients' radiographs and ROM-MR images, we have created some general guidelines for complete reduction of the femoral head into the acetabulum. By this approach, after the AI and CHDD are confirmed, the next step is to use the ROM-MRI to evaluate the labrum, either by visually comparing the orientation with that of the unaffected side or by measuring the LA and ULD values as we have done. Next, the ZCF would be determined, or the medial joint space would at least be visually inspected. If soon after closed or open reduction plus a hip spica cast the hip is found to be unstable, (i.e., the ULD is ≤ 0° and the ZCF moves from zone 2 in the neutral position to zone 3 in abduction), then the abduction brace treatment should be extended. However, a child of walking age is understandably reluctant to wear a brace. If, 1-2 years after closed or open reduction plus use of an abduction brace the patient shows the same or similar MRI findings, a secondary surgical procedure should be considered (Figs. 3 and 4). If the ULD and ZCF criteria are unfavorable (ULD > 0°, and the ZCF is zone 2 in the neutral position and abduction, meaning that the medial joint space is not decreased in abduction) (Fig. 5), and the medial superior acetabular cartilage is thickened, then both femoral and pelvic osteotomies are required to enhance complete remodeling of the hip. In a case in which the labrum is directed horizontally due to pressure from the femoral head, combined with a hypertrophied articular cartilage, reversal of the pathology is not simply achieved by a brace, or by a unilateral femoral or pelvic osteotomy (Fig. 6).
It is too early to describe our long-term treatment outcomes because osteoarthritis in DDH usually occurs in early or late adulthood, but the results appear to be excellent thus far. Among the patients who underwent surgery, six had another ROM-MRI scan after the metal was removed. In these six patients, the mean LA of the affected hip in the neutral position decreased by 8.7° (from 114.7° to 106.0°) after surgery, and the ZCF was zone 3 (medial) in the neutral position and abduction.
The scanner which we used cannot give a complete picture of the relationship between the diseased femoral head and the acetabulum because it has limited space for the patient's free leg movement. As with arthrography, the images do not show the hip in a weight-bearing position. For younger children who would not tolerate the noise, positioning and being enclosed in the small scanner, the use of sedation is advisable. MR scanning often places a financial burden on the patient's parents. As an inducement for the parents, our institute enables us to offer a discount for a ROM-MRI (3 slices" in each of the 5 positions [T2 only] for one-half of the current cost of a normal standard MR scan).
While we do not wish to disparage the usefulness of the time-honored radiograph for children in this age range, its limitations are quite obvious, and the best use of radiographs will be in conjunction with an imaging technique, such as ROM-MRI, which elucidates the soft tissue structures. ROM-MRI clearly demonstrates the acetabulolabral relationship in detail, which is not possible in radiographs. The convenience of using MRI on an outpatient clinic basis lessens the need for arthrography in the operating room, and the clear images of the labrum and the relationship between the acetabulum and the femoral head enhance accurate decision-making for further treatment.
Figures and Tables
Fig. 1
Measurement of labral angle (LA). LA is defined as the angle that the labrum makes with the acetabulum (that is, with the line that is used for measurement of acetabular index [AI]). Line A is the midline of the labrum: that is, it passes through a point midway between the outer and inner attachment points of the labrum (points B and C) and the distal apex of the labrum. Line H is Hilgenreiner's line. The figure shows a dysplastic hip in neutral; such hips have LA values that are high in neutral and low in abduction.

Fig. 2
Determination of the zone of compressive force (ZCF). The superior portion of the bony acetabulum is subdivided into three equal zones (numbered 2, 3, and 4); the portion of the roof consisting of the labrum alone is zone 1. ZCF is the acetabular zone which is entered by a line, tilted medially at 16° off the vertical (the vertical is a line perpendicular to the line of Hilgenreiner) and passing through the center of the femoral head. The circle is the smallest one that will completely contain the outer margin of the bony head; the point in the circle is its center. The figure shows a dysplastic hip in abduction; in such hips, the ZCF is usually zone 2 in the neutral position, shifting to zone 3 in abduction.

Fig. 3
Femoral osteotomy. (A) This 25-month-old girl had left hip dysplasia at initial presentation. (B) On the serial range of motion-magnetic resonance imaging (SROM-MRI), her uncorrected labral deformity (ULD) value was -3°; thus she was a candidate for a single femoral or pelvic osteotomy. Femoral varus osteotomy was performed when she was 29 months old. (C) After implant removal, she underwent a second SROM-MRI at 4 years and 2 months of age. Even though her ULD value following surgery was 3°, the zone of compressive force continued as zone 3 even in the neutral position (previously it was zone 2). (D) The radiograph, taken when he was 6 years and 2 months of age, showed improved condition of the hip. NEUT: neutral, ABD: abduction.

Fig. 4
Pelvic osteotomy. This boy had a right hip dislocation, and he underwent closed reduction when he was 13 months old. (A) At the age of 4 years and 5 months (3 years and 4 months after reduction), his right hip was still dysplastic. (B) On the serial range of motion-magnetic resonance imaging (SROM-MRI), the uncorrected labral deformity (ULD) value was 4° and the zone of compressive force (ZCF) shifted from zone 2 to 3; thus he was a candidate for single femoral or pelvic osteotomy. We performed a Salter innominate osteotomy when he was 4 years and 8 months old. (C) In a second SROM-MRI scan taken when he was 9 years and 1 month old, ZCF was zone 3 in both the neutral (NEUT) and abduction (ABD) positions and his ULD value was -6°. (D) The follow-up radiograph, taken at this time, showed improved condition of the hip.

Fig. 5
Borderline case (single vs. dual osteotomy). This girl had a right hip dislocation, and she underwent closed reduction when she was 13 months old. (A) However, at the age of 4 years and 5 months, her right hip was still dysplastic. (B) On the serial range of motion-magnetic resonance imaging (SROM-MRI), her uncorrected labral deformity value was 6° and the zone of compressive force did not move medially on abduction, but remained at zone 2-3. Thus, we could have chosen to perform just one osteotomy (hip or pelvis) or both. To be on the safe side, we performed a dual femoral and pelvic osteotomy. (C) The follow-up radiograph, taken at the age of 9 years and 3 months, showed much improved condition of the hip. NEUT: neutral, ABD: abduction.

Fig. 6
Failure of unilateral osteotomy to reverse pathology. This girl had a left hip dislocation, and was treated with open reduction when she was 21 months old. (A) Two years after reduction (at 3 years and 9 months of age), the left hip was still dysplastic with a widened superior gap; at this time we performed a Dega-type periacetabular osteotomy. (B) Four years after the periacetabular osteotomy (at 7 years and 9 months of age), the left hip was still dysplastic and the superior gap was still wider than normal. At that time, the condition of the hip was checked by range of motion magnetic resonance imaging: (C) neutral and (D) abduction, which revealed a thickened medial acetabular wall and irregular ossification in the hypertrophied acetabular cartilage. (E) The final radiograph, taken at 13 years and 8 months of age, showed progress in the ossification at the widened superior joint gap, although it was not enough to lead to a normal hip joint (note the dysplasia, particularly the upward direction of the lateral end of the sourcil and the broken Shenton's line).

ACKNOWLEDGEMENTS
One of the authors (Hui-Taek Kim) has received funding (2004-26) from "Medical Research Institute, Pusan National University Hospital."
References
1. Mladenov K, Dora C, Wicart P, Seringe R. Natural history of hips with borderline acetabular index and acetabular dysplasia in infants. J Pediatr Orthop. 2002. 22(5):607–612.

2. Pirpiris M, Payman KR, Otsuka NY. The assessment of acetabular index: is there still a place for plain radiography? J Pediatr Orthop. 2006. 26(3):310–315.
3. Tasnavites A, Murray DW, Benson MK. Improvement in acetabular index after reduction of hips with developmental dysplasia. J Bone Joint Surg Br. 1993. 75(5):755–759.

4. Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976. (119):39–47.
5. Wiberg G. Studies on dysplastic acetabular and congenital subluxation of the hip joint: with special reference to the complication of osteoarthritis. Parts HV. Acta Chir Scand Suppl. 1939. 83:Suppl 58. 7–38.
6. Chen IH, Kuo KN, Lubicky JP. Prognosticating factors in acetabular development following reduction of developmental dysplasia of the hip. J Pediatr Orthop. 1994. 14(1):3–8.

7. Smith WS, Badgley CE, Orwig JB, Harper JM. Correlation of postreduction roentgenograms and thirty-one-year follow-up in congenital dislocation of the hip. J Bone Joint Surg Am. 1968. 50(6):1081–1098.

8. Wagner H. Weil UH, editor. Transplantation of the greater trochanter. Progress in orthopaedic surgery. Vol 2. Acetabular dyspasia and skeletal dysplasia in childhood. 1978. Heidelberga: Springer;99–102.
9. Kim HT, Kim JI, Yoo CI. Acetabular development after closed reduction of developmental dislocation of the hip. J Pediatr Orthop. 2000. 20(6):701–708.

10. Ferguson SJ, Bryant JT, Ito K. The material properties of the bovine acetabular labrum. J Orthop Res. 2001. 19(5):887–896.

11. Horii M, Kubo T, Inoue S, Kim WC. Coverage of the femoral head by the acetabular labrum in dysplastic hips: quantitative analysis with radial MR imaging. Acta Orthop Scand. 2003. 74(3):287–292.

12. Kim YH. Acetabular dysplasia and osteoarthritis developed by an eversion of the acetabular labrum. Clin Orthop Relat Res. 1987. (215):289–295.

13. Miozzari HH, Clark JM, Jacob HA, von Rechenberg B, Notzli HP. Effects of removal of the acetabular labrum in a sheep hip model. Osteoarthritis Cartilage. 2004. 12(5):419–430.

14. Nishii T, Tanaka H, Sugano N, Miki H, Takao M, Yoshikawa H. Disorders of acetabular labrum and articular cartilage in hip dysplasia: evaluation using isotropic high-resolutional CT arthrography with sequential radial reformation. Osteoarthritis Cartilage. 2007. 15(3):251–257.

15. Petersen W, Petersen F, Tillmann B. Structure and vascularization of the acetabular labrum with regard to the pathogenesis and healing of labral lesions. Arch Orthop Trauma Surg. 2003. 123(6):283–288.

16. Ponseti IV. Morphology of the acetabulum in congenital dislocation of the hip: gross, histological and roentgenographic studies. J Bone Joint Surg Am. 1978. 60(5):586–599.

17. Ueshima K, Takahashi KA, Fujioka M, et al. Relationship between acetabular labrum evaluation by using radial magnetic resonance imaging and progressive joint space narrowing in mild hip dysplasia. Magn Reson Imaging. 2006. 24(5):645–650.

18. Pauwels F. Schatzker J, editor. Biomechanical principles of varus/valgus intertrochanteric osteotomy (Pauwels I and II) in the treatment of osteoarthritis of the hip. The intertrochanteric osteotomy. 1984. New York: Springer;3–23.

19. Albinana J, Morcuende JA, Weinstein SL. The teardrop in congenital dislocation of the hip diagnosed late: a quantitative study. J Bone Joint Surg Am. 1996. 78(7):1048–1055.

20. Albinana J, Dolan LA, Spratt KF, Morcuende J, Meyer MD, Weinstein SL. Acetabular dysplasia after treatment for developmental dysplasia of the hip: implications for secondary procedures. J Bone Joint Surg Br. 2004. 86(6):876–886.
21. Brougham DI, Broughton NS, Cole WG, Menelaus MB. The predictability of acetabular development after closed reduction for congenital dislocation of the hip. J Bone Joint Surg Br. 1988. 70(5):733–736.

22. Harris NH, Lloyd-Roberts GC, Gallien R. Acetabular development in congenital dislocation of the hip: with special reference to the indications for acetabuloplasty and pelvic or femoral realignment osteotomy. J Bone Joint Surg Br. 1975. 57(1):46–52.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download