Abstract
Background
Methods
Results
Figures and Tables
 | Fig. 1The serial radiographs of a 55-year-old female patient show (A) intramedullary calcified bone tumor in the proximal humeral metaphysis preoperatively. The follow-up radiographs taken (B) immediately after the operation, (C) 6 weeks postoperatevely and, (D) 12 weeks postoperatively show the gradual resorption of the injectable calcium sulfate. (E) The final radiograph shows skeletal incorporation. |
 | Fig. 2Linear regression analysis demonstrated that the volume of the injectable calcium sulfate (ICS) graft was correlated with (A) the time to resorption and (B) the time to healing. On the contrary, (C) the volume of the demineralized bone matrix (DBM)-based graft was not correlated with the time to healing. |
 | Fig. 3The anteroposterior radiographs of a 21-year-old man with fibrous dysplasia of his left femur neck show (A) the three months postoperative view after the curettage and injectable calcium sulfate grafting with prophylactic fixation. (B) Six months postoperatively, he complained of continuous pain on his left hip, and the radiograph showed the cortical breakage on the superior aspect of the femur neck (arrow). (C) Ten months postoperatively, complete fracture occurred in spite of activity restriction. Note that the calcium sulfate is not completely resorbed. (D) The final radiograph after curettage of the remnant calcium sulfate and internal fixation with autogenous bone grafting. |
 | Fig. 4The radiographs showed a 20-year-old man who had undergone surgery for myxoid chondrosarcoma that arose from the calcaneus (A, B). (A) The immediate postoperative view shows the status of injectable calcium sulfate injection. At the follow-up, the calcium sulfate was (B) gradually resorbed in a centripetal fashion, and (C) it was completely resorbed at 6 weeks postoperatively. (D) The magnetic resonance imaging taken 6 months postoperatively shows a peripherally enhanced cystic lesion within the calcaneus, and this indicated failure of healing. |
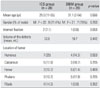
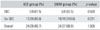
Table 1

SBC: simple bone cyst, M-CS: myxoid chondrosarcoma, OF: ossifying fibroma, ABC: aneurismal bone cyst, FD: fibrous dysplasia, CB: chondroblastoma, IO-lipoma: intraosseous lipoma, L-CS: low grade chondrosarcoma, L-OSA: low grade osteosarcoma, IO-ganglion: intraosseous ganglion, EC: enchondroma, NOF: nonossifying fibroma, GCT: giant cell tumor, OO: osteoid osteoma, LCH: Langerhans cell histiocytosis, 115: minimally-invasive injectable graft (MIIG) 1.1.5, X3: MIIGX3, Allo: allogenic bone graft, Auto: autologous bone graft, ICS: injectable calcium sulfate, DBM: demineralized bone matrix, BM: bone marrow.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download