Abstract
Background
This study examined the clinical and radiologic mid-term results of patients treated by Oxford minimally invasive unicompartmental knee arthroplasty.
Methods
One hundred and eighty-eight knees of unicompartmental knee arthroplasties with Oxford Uni® in 166 patients (16 males and 150 females), which were performed between 2002 and 2005, were reviewed. The mean age was 65.3 years (range, 44 to 82 years) and the mean follow-up period was 79.8 months (range, 56 to 103 months). The preoperative diagnosis was osteoarthritis in 166 patients, osteonecrosis of the medial femoral condyle in 20 and chondrocalcinosis in 2.
Results
The mean Hospital for Special Surgery (HSS) knee score was 67.5 (range, 52 to 75) preoperatively and 89.9 (range, 85 to 100) at the final follow-up. The mean preoperative flexion contracture was 6.5° (range, 0 to 15°) and 0.8° (range, 0 to 5°) at the final follow-up. The mean full flexion increased from 135° (range, 90 to 150°) preoperatively to 150° (range, 140 to 165°) at the final follow-up. Active full flexion was possible within 2 postoperative months. The squatting and cross-leg postures were possible in 133 patients (80.1%) and 152 patients (91.6%) at the final follow-up. The mean tibiofemoral angle was improved from varus 1.5° to valgus 4.8°. Complications were encountered in 18 cases (9.5%). A bearing dislocation occurred in 10 cases (5.3%), tibial component loosening in 4 cases (2.1%), femoral loosening in 3 cases (1.6%) and lateral translation in 1 case (0.5%). The mean time for a bearing dislocation was 22.6 months (range, 3 to 70 months) postoperatively. Seven cases returned to the predislocation level of activity with the insertion of a thicker bearing and 3 cases converted to total knee arthroplasty.
Conclusions
Minimally invasive unicompartmental knee arthroplasty with Oxford Uni® provided rapid recovery, good pain relief and excellent function suitable for the Korean lifestyle. In contrast, the high complication rates of Oxford Uni® encountered in the mid-term results suggested less reliability than total knee arthroplasty.
With the aging of the population worldwide, the incidence of symptomatic osteoarthritis of the knee and other degenerative knee disease are also increasing. Unicompartmental knee arthroplasty (UKA) is a treatment option for patients with medial compartment osteoarthritis of the knee.1-3) With the improvements in surgical techniques and instruments, this procedure has many advantages, such as smaller incision, less soft tissue injury, preservation of normal knee kinematics, minimal bone resection, less morbidity due to minimal postoperative blood loss, shortened hospital stay and rapid recovery.4,5) In addition, it appears quite reasonable to replace the only involved unilateral compartment of the knee. Despite these factors, many reports6-8) have shown less favorable long term results or early failures, which require revision total knee arthroplasty or re-operation. Recently, the use of unicompartmental knee arthroplasty has been a contentious issue since its first introduction.
This study compared the mid-term clinical and radiologic results of unicompartmental knee arthroplasty with Oxford Uni® (Biomet Ltd., Bridgend, UK) with those reported in the literatures. The survival and complications were also analyzed.
Approval for the present study from the institutional review board was obtained. From January 2002 to December 2005, 188 consecutive knees of 166 patients were included with no loss to follow-up. The mean age and follow-up period was 65.3 years (range, 44 to 82 years) and 79.8 months (range, 56 to 103 months), respectively. All unicompartmental knee arthroplasty procedures were performed by the senior author.
The indications for unicompartmental knee arthroplasty were severe antero-medial knee pain and considerable difficulty in walking and performing daily activities with a complete loss of cartilage on the medial compartment. The other indications were an intact anterior cruciate ligament (ACL) confirmed by magnetic resonance image (MRI), varus deformity < 15°, flexion contracture < 15°, intact lateral compartment and minimal translation via varus-valgus stress view. The preoperative diagnosis was osteoarthritis in 166 patients, osteonecrosis of medial femoral condyle in 20 and chondrocalcinosis in 2.
All patients were placed in the supine position after spinal anesthesia on a routine operating table with the lower leg rest bent downward. The thigh was fixed with a thigh holder with the hip flexed approximately 30° and the thigh tourniquet was inflated. The lower leg rest was bent downward and the thigh was held with hip flexion to allow passive knee flexion at least 120° during the procedure. Frequent flexion-extension manipulations are necessary during the procedure because some of the medial structures are preferentially visualized at either low or high degree of flexion.9) A medial parapatellar incision was used and the patella was not everted. The mean length was 6.3 cm (range, 6 to 6.5 cm). The average thickness of the bearings were 3.4 mm (range, 3 to 7 mm). All bearings used in this study were non-anatomic bearings, which were non-specific and usable on either side.
The clinical results were evaluated using the range of knee motion and Hospital for Special Surgery (HSS) knee score, preoperatively and at the final follow-up. The squatting and cross leg sitting postures, which were common in Korean daily life, were also checked. In radiologic assessments, weight-bearing anteroposterior and lateral radiographs of the knee as well as a long hip to ankle film for measuring the tibiofemoral angle were taken at each visit. Mechanical failures, such as component loosening or rotation and component migration or subsidence, were also checked.10,11) Either the tibial or femoral component were considered to be loosening when the radiolucency was > 2 mm around the components. Rotation of the component was considered when > 10°. The end point for survival was defined as revision for any reason. The 95% confidence intervals were calculated using the Kaplan-Meier method. All the data was analyzed statistically using SPSS ver.18.0 (SPSS Inc., Chicago, IL, USA) and a p < 0.05 was considered significant.
In all patients, passive full flexion of the knee and painless active full flexion was possible within postoperative 7 days and postoperative 2 months, respectively. The mean preoperative flexion contracture was 6.5° (range, 0 to 15°), which was improved to mean 0.8° (range, 0 to 5°) at the final follow-up. The mean preoperative full flexion was 135° (range, 90 to 150°), which was improved to a mean of 150° (range, 140 to 165°) at the final follow-up. The flexion increased by an average of 15°. The mean HSS score increased from 67.5 (range, 52 to 75) to 89.9 (range, 85 to 100) at the time of final follow-up (p < 0.05). At the final follow-up, squatting and cross-leg postures were possible in 133 patients (80.1%) and 152 patients (91.6%), respectively. The mean preoperative tibiofemoral angle was varus 1.5°, which was to a mean valgus of 4.8°.
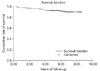
Complications occurred in 18 knees in 17 patients (9.5%) (Table 1). Bearing dislocations occurred in 10 cases (5.3%); 5 cases anteriorly and 5 cases posteriorly. Beneath the tibial components, either completely or partially radiolucent lines were observed in 131 knees out of a total of 188 knees. On the other hand, the formation of radiolucent lines was not related with tibial component loosening. Tibial component loosening was noted in 4 cases (2.1%), femoral component loosening in 3 cases (1.6%) and lateral translation in 1 case (0.5%). The mean time to bearing dislocation was postoperative 22.6 months (range, 3 to 70 months). One case of bearing dislocation with valgus overcorrection was converted to revision total knee arthroplasty. The other case of a bearing dislocation with a visible torn anterior cruciate ligament intraoperatively was also converted to revision total knee arthroplasty. Two bearing dislocations occurred in one patient. The first bearing dislocation occurred at postoperative 2 years 3 months. A thicker and anatomic bearing was inserted and she returned to her pre-dislocation level of activity but she had a second bearing dislocation at postoperative 4 years. Unicompartmental knee arthroplasty was converted to revision total knee arthroplasty. The remaining seven cases returned to their pre-dislocation level of activity with the insertion of thicker bearings. These 7 cases, 4 and 3 with tibial and femoral component loosening, respectively, were converted to revision total knee arthroplasty. One case of lateral translation was asymptomatic and close observation was required. A total of ten knees were converted to revision total knee arthroplasty. The survival rate at 6.6 years was 89.9% with revision for any reason as the end point (95% confidence interval) (Fig. 1).
Unicompartmental knee arthroplasty is a treatment option for selected patients with unicompartmental osteoarthritis. Appropriate patient selection and good surgical techniques are the key factors for achieving good results but a range of results and a number of complications have been reported since its introduction.1,6-8,12-14) Unicompartmental knee arthroplasty for the treatment of medial osteoarthritis is still controversial. The reasons for early failures include the implant design, disease progression of the lateral compartment, inappropriate patient selection and surgical technique.
In a population based study from the Finnish arthroplasty register, fixed bearing Miller-Galante II design showed an 86% survival rate at 7 years.15) Koskinen et al.16) reported that the survival rate of this prosthesis was 86.6%. The increased revision rate appears to be due to the excessive wear of the polyethylene liner or valgus overcorrection. Polyethylene liner wear has been cited as a cause of failure after unicompartmental knee arthroplasty. Gioe et al.17) reported that polyethylene wear accounted for 21% of all revisions of unicompartmental knee arthroplasty. In his study, progression in the uninvolved compartment and aseptic loosening were other reasons for revision. Progression of the disease in the other compartment of the knee is a common reason for revision.17,18) Insall and Aglietti19) concluded that overcorrection of the mechanical axis can result in increased degeneration of the uninvolved side. In the present study, correction of the tibiofemoral angle ranged from varus 1.5° to valgus 4.8°. The mean degree of correction was 6.3°. An attempt was made to avoid overcorrection of the mechanical axis. Patients with a neutral axis are at risk of valgus overcorrection at surgery.
The excellent results by Berger et al.20) suggested that strict inclusion criteria for the procedure are a key factor for success. In the present study, narrow and strict indications were applied for patient selection.
Many excellent results of unicompartmental knee arthroplasty have been reported using Oxford Uni®.21-24) Svard and Price24) reported a 95% cumulative survival rate. Their results were similar to those reported by the designers of this prosthesis. They suggested that if patients are selected appropriately, Oxford Uni® is a reliable treatment option for anteromedial osteoarthritis of the knee. Oxford Uni® has a mobile bearing with full congruency. Despite the high wear rate of fixed bearing,16,25) a mobile bearing can minimize polyethylene wear.26,27) Aldinger et al.25) reported far less wear and failure rates of mobile bearings than fixed bearings. This study confirmed that the meniscal bearing moves posteriorly, as the knee reaches full flexion under the fluoroscopic image intensifier (Fig. 2).
The notable complications in our study were bearing dislocations. Ten bearing dislocations out of a total of 18 complications were encountered. Bearing dislocations were greater than component loosening. The important mechanism of bearing complications would be incomplete gap balancing between flexion and extension. Lewold et al.28) reported that bearing dislocation could be attributed to malposition of the components and soft tissue imbalance with subsequent maltracking of the meniscal bearing. Other possible mechanisms are posterior impingement by the remaining meniscus or osteophytes, ligament laxity due to release of the medial collateral ligament or physiologic laxity of lateral collateral ligament.29) The mechanism of bearing dislocation was examined from careful history taking when the moment meniscal bearing dislocation occurred. The patients stated the moment when the bearing was dislocated, the knee joint was highly twisted with the foot and ankle fixed to the floor. When one case of bearing dislocation was re-operated, a torn anterior cruciate ligament was observed, which was identified as being intact preoperatively. Senter and Hame30) showed that hyperflexion also increases the ACL force. The different lifestyle in Korea, which involves postured with full flexion, squatting and sitting on the floor, might cause strain of the anterior cruciate ligament, which might be a causative factor of bearing dislocation. Another probable factor of bearing dislocation was the early design of the meniscal bearing. All dislocated bearings were non-anatomic type bearings that were non-specific and usable on either side. To provide further protection from dislocation, a new anatomic meniscal bearing has been developed by Oxford group. These specific right and left bearings have an extended length of the medial wall, which increases significantly the amount of rotation that the bearing has to undergo before spin out can take place. In addition, the anterior medial corner of the bearing has been reduced to reduce any anterior overhang in extension that could be a source of soft tissue irritation in some patients. The non-anatomic design of the meniscal bearing might be another factor for bearing dislocation. We recently experienced one case of anatomic bearing dislocation, which was found to have a deformed reduced posterior lip with an intact anterior cruciate ligament. This suggests that deformation of the posterior lip during squatting is one of the causative factors in a bearing dislocation (Fig. 3).
Seven cases of tibial and femoral component loosening were encountered, which all were converted to revision total knee arthroplasty. Loosening of either tibial or femoral component was a commonly reported cause of failure of unicompartmental knee arthroplasty. It should be noted that the femoral component of Oxford Uni® has single fixation peg, which is in contrast to the two fixation peg designs of other unicompartmental knee arthroplasties. Although multiple drill holes were made on the distal femur before inserting the femoral component, it was assumed that one peg is not enough for femoral fixation and rotational stability. The dual peg of the femoral component is believed to be more preferable.
Minimally invasive Oxford Uni® provided rapid recovery, good pain relief and excellent function that are suitable for the Korean lifestyle. On the other hand, the high complication rate in the mid-term result of Oxford Uni® indicated less reliability compared to total knee arthroplasty.
Figures and Tables
References
1. Goodfellow JW, Tibrewal SB, Sherman KP, O'Connor JJ. Unicompartmental Oxford Meniscal knee arthroplasty. J Arthroplasty. 1987. 2(1):1–9.

2. Inglis GS. Unicompartmental arthroplasty of the knee: a follow-up of 3 to 9 years. J Bone Joint Surg Br. 1984. 66(5):682–684.

3. Knutson K, Jonsson G, Langer Andersen J, Larusdottir H, Lidgren L. Deformation and loosening of the tibial component in knee arthroplasty with unicompartmental endoprostheses. Acta Orthop Scand. 1981. 52(6):667–673.

4. Laurencin CT, Zelicof SB, Scott RD, Ewald FC. Unicompartmental versus total knee arthroplasty in the same patient: a comparative study. Clin Orthop Relat Res. 1991. (273):151–156.
5. Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg Br. 1998. 80(5):862–865.
6. Marmor L. Unicompartmental knee arthroplasty: ten- to 13-year follow-up study. Clin Orthop Relat Res. 1988. (226):14–20.
7. Padgett DE, Stern SH, Insall JN. Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg Am. 1991. 73(2):186–190.

9. Argenson JN, Flecher X. Minimally invasive unicompartmental knee arthroplasty. Knee. 2004. 11(5):341–347.

10. Carr A, Keyes G, Miller R, O'Connor J, Goodfellow J. Medial unicompartmental arthroplasty: a survival study of the Oxford meniscal knee. Clin Orthop Relat Res. 1993. (295):205–213.
11. Hodge WA, Chandler HP. Unicompartmental knee replacement: a comparison of constrained and unconstrained designs. J Bone Joint Surg Am. 1992. 74(6):877–883.
12. Cameron HU, Jung YB. A comparison of unicompartmental knee replacement with total knee replacement. Orthop Rev. 1988. 17(10):983–988.
14. Laskin RS. Unicompartmental tibiofemoral resurfacing arthroplasty. J Bone Joint Surg Am. 1978. 60(2):182–185.

15. Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007. 78(1):128–135.

16. Koskinen E, Paavolainen P, Eskelinen A, et al. Medial unicompartmental knee arthroplasty with Miller-Galante II prosthesis: mid-term clinical and radiographic results. Arch Orthop Trauma Surg. 2009. 129(5):617–624.

17. Gioe TJ, Killeen KK, Hoeffel DP, et al. Analysis of unicompartmental knee arthroplasty in a community-based implant registry. Clin Orthop Relat Res. 2003. (416):111–119.

18. Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975-1997: an update with special emphasis on 41,223 knees operated on in 1988-1997. Acta Orthop Scand. 2001. 72(5):503–513.

19. Insall J, Aglietti P. A five to seven-year follow-up of unicondylar arthroplasty. J Bone Joint Surg Am. 1980. 62(8):1329–1337.

20. Berger RA, Meneghini RM, Jacobs JJ, et al. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2005. 87(5):999–1006.

21. Goodfellow JW, O'Connor J. Clinical results of the Oxford knee: surface arthroplasty of the tibiofemoral joint with a meniscal bearing prosthesis. Clin Orthop Relat Res. 1986. (205):21–42.
22. White SH, Ludkowski PF, Goodfellow JW. Anteromedial osteoarthritis of the knee. J Bone Joint Surg Br. 1991. 73(4):582–586.

23. Price AJ, Waite JC, Svard U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005. (435):171–180.

24. Svard UC, Price AJ. Oxford medial unicompartmental knee arthroplasty: a survival analysis of an independent series. J Bone Joint Surg Br. 2001. 83(2):191–194.
25. Aldinger PR, Clarius M, Murray DW, Goodfellow JW, Breusch SJ. Medial unicompartmental knee replacement using the "Oxford Uni" meniscal bearing knee. Orthopade. 2004. 33(11):1277–1283.
26. Goodfellow J, O'Connor J. The mechanics of the knee and prosthesis design. J Bone Joint Surg Br. 1978. 60(3):358–369.

27. O'Connor J, Imran A. Bearing movement after Oxford unicompartmental knee arthroplasty: a mathematical model. Orthopedics. 2007. 30:5 Suppl. 42–45.
28. Lewold S, Goodman S, Knutson K, Robertsson O, Lidgren L. Oxford meniscal bearing knee versus the Marmor knee in unicompartmental arthroplasty for arthrosis: a Swedish multicenter survival study. J Arthroplasty. 1995. 10(6):722–731.

29. Emerson RH Jr. Unicompartmental mobile-bearing knee arthroplasty. Instr Course Lect. 2005. 54:221–224.
30. Senter C, Hame SL. Biomechanical analysis of tibial torque and knee flexion angle: implications for understanding knee injury. Sports Med. 2006. 36(8):635–641.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download