Abstract
Background
Displaced intraarticular zone I and displaced zone II fractures of the proximal fifth metatarsal bone are frequently complicated by delayed nonunion due to a vascular watershed. Many complications have been reported with the commonly used intramedullary screw fixation for these fractures. The optimal surgical procedure for these fractures has not been determined. All these observations led us to evaluate the effectiveness of percutaneous bicortical screw fixation for treating these fractures.
Methods
Twenty-three fractures were operatively treated by bicortical screw fixation. All the fractures were evaluated both clinically and radiologically for the healing. All the patients were followed at 2 or 3 week intervals till fracture union. The patients were followed for an average of 22.5 months.
Results
Twenty-three fractures healed uneventfully following bicortical fixation, with a mean healing time of 6.3 weeks (range, 4 to 10 weeks). The average American Orthopaedic Foot & Ankle Society (AOFAS) score was 94 (range, 90 to 99). All the patients reported no pain at rest or during athletic activity. We removed the implant in all cases at a mean of 23.2 weeks (range, 18 to 32 weeks). There was no refracture in any of our cases.
There is still much controversy regarding the management of proximal fifth metatarsal fractures more than a century after its original description by Sir Robert Johns1) in 1902, as even today there are no specific guidelines for the management of these fractures. Many classifications have been described for proximal fifth metatarsal fractures.2-6) However, we prefer the three zone concept by Lawrence and Botte3) when classifying these fractures (Fig. 1). Zone I is the most proximal tuberosity avulsion fracture. Zone II is the metaphyseal-diaphyseal junction, and it is also the level of the fourth and fifth metatarsal articulations. This is the true Jones fracture location. Zone III is site of proximal diaphyseal stress fracture. Zone I and zone II fractures are due to acute injury, whereas the zone III fractures are usually pathological stress fractures.
It is of utmost importance to distinguish between the acute fractures and the diaphyseal stress fractures for proper management.7) Undisplaced zone I and zone II fractures usually respond well to conservative treatment; however, operative fixation of the displaced zone II fractures and the displaced intraarticular zone I fractures has shown better results than conservative treatment.6,8-10) To date, no clinical study has evaluated the effectiveness of percutaneous bicortical screw fixation for these fractures. Therefore, the aim of this study was to evaluate the effectiveness of percutaneous bicortical screw fixation for the displaced intraarticular zone I and zone II fractures of the proximal fifth metatarsal. We also evaluated the short- and long-term clinical and radiological results of the bicortical fixation of these fractures.
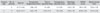
From January 2003 through August 2008, a total of 84 fractures of the proximal fifth metatarsal bone were treated operatively by one orthopaedic surgeon (JSS). However, in the present study we included only the displaced intraarticular zone I and zone II fractures with displacement of more than 2 mm, which were treated by percutaneous bicortical screw fixation. There were 23 such fractures (17 in zone II and 6 in zone I) that were treated by bicortical screw fixation. A total of 23 patients were followed up. Extraarticular zone I avulsion fractures, zone III diaphyseal stress fractures, severely comminuted fractures, pediatric fractures, open fractures and fractures that were treated by other methods of fixation were excluded. Our inclusion criteria for percutaneous bicortical screw fixation was acute, closed, not severely comminuted and more than 2 mm displaced intraarticular zone I and zone II fractures. The chronic, open or severely comminuted fractures were treated with open reduction and internal fixation with screws or wires. The displaced zone III diaphyseal fractures were treated with intramedullary screw fixation. The mechanism of injury was inversion of the ankle and adduction of the forefoot, which was twisting and falling in 20 patients and sports injury in 3 patients. In six of the zone I fractures, all the fractures were intraarticularily displaced more than 2 mm. The articulations of the fifth tarsometatarsal joint were involved. There were 12 males and 11 females (median age, 44.3 years; range, 16 to 74 years). Fifteen right feet and seven left feet were involved. Twenty three patients with 23 fractures (17 in zone II and 6 in zone I) were operated on using bicortical screw fixation at a mean of 6.96 ± 5.39 days (range, 1 to 23 days) after injury. We recorded the preoperative displacement and postoperative reduction following bicortical screw fixation in all the patients (Tables 1 and 2).
Our percutaneous operative technique involved the use of local anesthesia, bicortical placement of the guide pin, cannulated drilling and bicortical screw fixation. The patient was placed supine with the affected foot resting over the image intensifier. This arrangement helped us obtain the anteroposterior, lateral and oblique views of the foot with great ease and it allowed easy access to the base of the fifth metatarsal bone. A tourniquet was not applied. The surgeon made a stab incision about 0.5 to 1 cm proximal to the fifth metatarsal bone. After the incision, a 4.0 mm cannulated screw guide pin (Synthes Inc., Paoli, PA, USA) was inserted into the space between the plantar fascia and the peroneus brevis tendon under image guidance. A cannulated drill was used to drill across the fracture to the medial cortex. A partially threaded, 4.0 mm, cannulated, cancellous, titanium screw was then inserted under image guidance over the guide pin to ensure bicortical placement of the screw for compression (Fig. 2). We used a washer in seven cases with mild comminution. Each 4.0 mm screw had 16 mm threads, regardless of the overall length of the screw used. The guide pin was removed after documentation of the bicortical purchase of the screw. Care was taken to ensure the bicortical penetration, and that all the threads were distal to the fracture site. Closure of the wound in an appropriate manner was usually done with a single stitch. The patients were started on tolerable toe touch partial weight bearing during the post operative period. All the patients were advised to walk with crutches till 4 weeks. After 4 weeks, if the fracture was not displaced on radiographs, then the patient was started on full weight-bearing without any aids. However, if we found any loosening over the screw or widening of the fracture gap, then we waited for another 2 weeks till full weight-bearing. After 12 weeks there were no restrictions for the patient for running or contact sports. The serial radiographs were evaluated by two of the authors (VM, HWC).
All patients were followed with radiographs, including three views of the foot (anteroposterior, oblique, and lateral) at each visit. On the radiographs we observed a mean preoperative fracture site displacement of 3.33 ± 1.84 mm (range, 2.0 to 9.1 mm). Following bicortical fixation, a mean postoperative reduction of 1.24 ± 0.49 mm (range, 0.3 to 2.4 mm) was achieved. All the patients were followed clinically at 2 or 3 weeks intervals till the fracture healed. We determined fracture healing on radiographs by the disappearance of a fracture line and the appearance of bridging trabeculae on three of four cortices (Fig. 3). Twenty three fractures healed uneventfully following bicortical fixation with a mean healing time of 6.33 ± 1.74 weeks (range, 4 to 10 weeks). The mean healing time was 5.33 ± 1.03 weeks (range, 4 to 6 weeks) in zone I and 6.59 ± 1.84 weeks (range, 4 to 10 weeks) in zone II.
In one patient with zone I fracture, a bicortical screw was removed after 4 weeks because we noticed a significant gap at the fracture site (2.4 mm). Open reduction and tension band wiring were done following which the fracture healed in 8 weeks after fixation. We also recorded the average American Orthopaedic Foot & Ankle Society (AOFAS) score in all the patients at 6 months. An average AOFAS score was 94 ± 2.34 (range, 90 to 99). The patients were followed for an average of 22.5 ± 2.07 months (range, 17 to 33 months). All the patients reported no pain at rest or during athletic activity. We removed the implant in all the cases at a mean of 23.2 ± 3.14 weeks (range, 18 to 32 weeks). We did not observe refracture in any of our cases.
It is important to understand the anatomy of the fifth metatarsal bone for the management of zone I and II fractures. The tuberosity lies at the proximal aspect, and it serves as the attachment for the wide insertion of the peroneus brevis tendon. The diaphysis has a curve in its distal third. Ebraheim et al.11) reviewed the fifth metatarsal osteology and they found that the fifth metatarsal bone is curved and the dorsal-plantar cortex is thinner than the medial-lateral cortex. In regard to the blood supply, there is a vascular watershed area within the proximal diaphysis, which may be the reason for high rates of nonunion, delayed union and refracture in this region.12,13) Operative fixation shortens the recovery time with lesser rates of nonunion, delayed union and refracture. For these reasons, several authors have recommended early operative fixation even for non-displaced fractures, which is debatable.9,14) However, operative fixation should particularly be considered for displaced fractures with a displacement of more than 2 mm or for intraarticular fractures.10,15-17)
The most popular choice for operative fixation for these fractures is currently intramedullary fixation that traverses the proximal cortex and rests in the medullary canal. However, a review of the literature shows that significant complications have been reported with intramedullary fixation like refracture, a screw missing the medullary canal, etc.18-21)
Biomechanical issues have been raised in regard to intramedullary screw fixation. Gross and Bunch22) found that the cortical thickness of the fifth metatarsal bone is the least of any of the five metatarsals. Kavanaugh19) reported significant complications with using non-cannulated screws such as screw breakage and a screw missing the medullary canal. Glasgow et al.18) reported six failures when performing intramedullary fixation, with three refractures and three delayed unions. Some studies recommend using a longer or larger diameter screw for intramedullary fixation so as to increase the pull out strength.21,23-25) However, this might not always be possible as a longer or larger diameter screw can be detrimental given the curvature in the bone distally and the risk of cortical perforation and distraction of the fracture. The recently reported biomechanical studies have tested another method of fixation for these fractures by bicortical screw fixation. These studies have shown encouraging results for the zone I and zone II fracture fixation with using bicortical screw fixation.15-16) Bicortical fixation can achieve compression at the fracture site to promote primary bone healing while resisting the tension from ligamentous and muscle insertions.15,16) Wright et al.21) reported on six refractures following intramedullary fixation of proximal fifth metatarsal fractures in athletes despite the evidence of complete radiographic and clinical union before the return to full activity. They recommended using a larger diameter screw for fixation in athletes and more prolonged protection using bracing, shoe modification or an orthosis, and performing alternative imaging for assessing complete healing should be considered. We did not have any refracture with bicortical fixation during the treatment or following a return to full activity in any of our patients. We agree with Larson et al.'s 20) suggestion to wait till there is radiographic evidence of solid union before allowing a return to full activity so as to avoid refracture. We did not allow our patients to return to full sports activity till 12 weeks.
In our study the reduction of the preoperative displacement, which was a mean of 3.33 ± 1.84 mm, to a postoperative mean of 1.24 ± 0.49 mm supports the studies that have suggested that bicortical screws offer constant compression at the fracture site and this promotes healing of the fracture.15,16) The maximum preoperative displacement we observed was 9.1 mm in a zone II fracture, and we were able to achieve a postoperative reduction up to 1.8 mm. We were able to achieve compression within 2 mm in all the cases. It is worth mentioning that we achieved compression with bicortical screw fixation in both the cases that presented late to us. Bicortical fixation might decrease the bone union time by maintaining adequate compression at the fracture site. We observed fracture healing with bicortical fixation at a mean of 6.3 ± 1.74 weeks, which compares favorably with that of the previous studies.8,9)
Bicortical screw fixation offers better stability than an intramedullary construct because of three reasons: 1) bicortical screw fixation offers greater fixation stability by the screws purchase the medial cortex, 2) bicortical screw fixation allows the load to disperse over a greater cortex surface area, and so this significantly increases the resistance to a load better than that of an intramedullary construct, and 3) bicortical screw fixation also has significantly more modulus of elasticity than does a intramedullary construct. We also tried more oblique placement of the screw, as was recommended, for better anchoring without generating stress risers.16) Other advantages of the percutaneous bicortical fixation are 1) in case of failure to achieve reduction or significant comminution intraoperatively by a percutaneous technique, the same incision can be converted to a larger incision for open reduction and fixation and 2) there are less chances of injury to the peroneus brevis because the entry point and the direction of screw are more laterally and distally placed. Vertullo et al.26) suggested that intramedullary screw fixation of proximal fifth metatarsal fractures offers little resistance to rotation of the proximal and distal fragments relative to one another. They also suggested that a fixation device that has the capability to resist torsion as well as tension and bending would appear to be optimal to treat these fractures. We believe that bicortical screw fixation satisfies all these criteria. We conclude that bicortical screw fixation is a reliable, easy and safe method of fixation for displaced intraarticular zone I and II fractures. We recommend it as one of the useful techniques for fixation of displaced zone II fractures and displaced intraarticular zone I fractures.
The limitation of this study is this was an uncontrolled retrospective study, and so further studies with more cases should be done before establishing bicortical screw fixation as the method of choice for fixation of these fractures.
Figures and Tables
Fig. 1
Schematic representation of the fracture zones for fifth metatarsal base fractures by Lawrence and Botte3) (zone I, zone II, zone III) and the gray-colored area represents the zone II and intraarticular zone I fractures for surgical intervention in this study.

Fig. 2
Intraoperative radiographs. (A) Stab incision. (B) Guide wire introduction. (C) Bicortical guide wire placement. (D) Bicortical screw fixation (oblique). (E) On the lateral view, note the compression at the fracture site following bicortical fixation.

References
1. Jones R. I. Fracture of the base of the fifth metatarsal bone by indirect violence. Ann Surg. 1902. 35(6):697–700.
2. DeLee JC, Evans JP, Julian J. Stress fracture of the fifth metatarsal. Am J Sports Med. 1983. 11(5):349–353.

3. Lawrence SJ, Botte MJ. Jones' fractures and related fractures of the proximal fifth metatarsal. Foot Ankle. 1993. 14(6):358–365.

4. Torg JS, Balduini FC, Zelko RR, Pavlov H, Peff TC, Das M. Fractures of the base of the fifth metatarsal distal to the tuberosity: classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am. 1984. 66(2):209–214.

5. Dameron TB Jr. Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J Bone Joint Surg Am. 1975. 57(6):788–792.

6. Quill GE Jr. Fractures of the proximal fifth metatarsal. Orthop Clin North Am. 1995. 26(2):353–361.

7. Reinherz RP, Sink CA, Westerfield M. Management of trauma to the fifth metatarsal bone. J Foot Surg. 1989. 28(4):301–307.
8. Mologne TS, Lundeen JM, Clapper MF, O'Brien TJ. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005. 33(7):970–975.

9. Portland G, Kelikian A, Kodros S. Acute surgical management of Jones' fractures. Foot Ankle Int. 2003. 24(11):829–833.

11. Ebraheim NA, Haman SP, Lu J, Padanilam TG, Yeasting RA. Anatomical and radiological considerations of the fifth metatarsal bone. Foot Ankle Int. 2000. 21(3):212–215.

12. Shereff MJ, Yang QM, Kummer FJ, Frey CC, Greenidge N. Vascular anatomy of the fifth metatarsal. Foot Ankle. 1991. 11(6):350–353.

13. Smith JW, Arnoczky SP, Hersh A. The intraosseous blood supply of the fifth metatarsal: implications for proximal fracture healing. Foot Ankle. 1992. 13(3):143–152.

14. Mindrebo N, Shelbourne KD, Van Meter CD, Rettig AC. Outpatient percutaneous screw fixation of the acute Jones fracture. Am J Sports Med. 1993. 21(5):720–723.

15. Husain ZS, DeFronzo DJ. Relative stability of tension band versus two-cortex screw fixation for treating fifth metatarsal base avulsion fractures. J Foot Ankle Surg. 2000. 39(2):89–95.

16. Husain ZS, DeFronzo DJ. A comparison of bicortical and intramedullary screw fixations of Jones' fractures. J Foot Ankle Surg. 2002. 41(3):146–153.

17. Zwitser EW, Breederveld RS. Fractures of the fifth metatarsal: diagnosis and treatment. Injury. 2010. 41(6):555–562.

18. Glasgow MT, Naranja RJ Jr, Glasgow SG, Torg JS. Analysis of failed surgical management of fractures of the base of the fifth metatarsal distal to the tuberosity: the Jones fracture. Foot Ankle Int. 1996. 17(8):449–457.

19. Kavanaugh JH, Brower TD, Mann RV. The Jones fracture revisited. J Bone Joint Surg Am. 1978. 60(6):776–782.

20. Larson CM, Almekinders LC, Taft TN, Garrett WE. Intramedullary screw fixation of Jones fractures: analysis of failure. Am J Sports Med. 2002. 30(1):55–60.
21. Wright RW, Fischer DA, Shively RA, Heidt RS Jr, Nuber GW. Refracture of proximal fifth metatarsal (Jones) fracture after intramedullary screw fixation in athletes. Am J Sports Med. 2000. 28(5):732–736.

22. Gross TS, Bunch RP. A mechanical model of metatarsal stress fracture during distance running. Am J Sports Med. 1989. 17(5):669–674.

23. Kelly IP, Glisson RR, Fink C, Easley ME, Nunley JA. Intramedullary screw fixation of Jones fractures. Foot Ankle Int. 2001. 22(7):585–589.

24. Porter DA, Rund AM, Dobslaw R, Duncan M. Comparison of 4.5- and 5.5-mm cannulated stainless steel screws for fifth metatarsal Jones fracture fixation. Foot Ankle Int. 2009. 30(1):27–33.

25. Reese K, Litsky A, Kaeding C, Pedroza A, Shah N. Cannulated screw fixation of Jones fractures: a clinical and biomechanical study. Am J Sports Med. 2004. 32(7):1736–1742.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download