Abstract
Background
To evaluate the utility of additional fixation methods and to suggest a method of reduction in the treatment of unstable pertrochanteric femur fractures with a sliding hip screw (SHS).
Methods
A retrospective study was performed on thirty patients with unstable pertrochanteric femur fractures, who were operated on with a SHS between September 2004 and September 2009 and were followed up for at least 6 months. The additional fixation devices were as follows; antirotation screw (21 cases), fixation of displaced fractures of the posteromedial bone fragment (cerclage wiring, 21 cases and screw, 2 cases) and trochanter stabilizing plate (27 cases). Clinically, the Palmer's mobility score and Jensen's social function group were used. Radiologically, alignment and displacement were observed. The tip-apex distance (TAD) and sliding of the lag screw were measured, and the position of the lag screw within the femoral head was also examined.
Results
The mean age at the time of surgery was 76 years (range, 56 to 89 years) and the average follow-up period was 25 months (range, 6 to 48 months). At the last follow-up, the average mobility and social function score was 6.2 (± 3.5) and 2.3 (± 1.5). Postoperatively, the alignment and displacement indices were adequate in almost all the cases. The mean amount of lag screw sliding and the mean TAD was 5.1 mm (range, 2 to 16 mm) and 6 mm (range, 3 to 11 mm) respectively. The lag screws were located in the center-center zone in 21 cases. The average period to union was 18.7 weeks without any cases of nonunion or malunion. Mechanical failure was noted in one case with breakage of the lag screw and clinical failure was noted in another case with persistent hip pain related to excessive sliding (16 mm).
The pertrochanteric femur fracture can be classified simply into three groups; stable fractures (A1), unstable fractures (A2), and transtrochanteric fractures (A3).1) In cases of unstable fractures (type A2), the treatment can often be frustrating with excessive sliding being the main concern.1) Historically, sliding hip screws (SHS) have been the preferred implant to stabilize trochanteric area fractures.2) On the other hand, intramedullary hip screws have gained popularity more recently owing to their mechanical and theoretical advantages compared to the SHS. Although they have superiority in type A3, there is some concern with this superiority in type A2 because it is important to obtain anatomical reduction as perfectly as possible by direct manipulation. In addition, intramedullary nails, such as proximal femur nail and proximal femur nail antirotation, do not appear to be more advantageous in obtaining suitable reduction and fixation for bone union than the conventional SHS. Therefore, type A2 trochanteric area fractures were treated using a range of additional methods to obtain stable fixation with the SHS.
Seventy eight cases of unstable pertrochanteric femur fractures were treated with SHS from September 2004 to September 2009. Of them, forty eight cases were excluded because of death and loss of contact. The remaining thirty cases (male:female = 8:22) were examined and followed up until March 2010. The inclusion criteria included pertrochanteric femur fractures (in people over the age of sixty years) which could be classified as type A2. Type A2 fractures are similar to the types 3, 4, and 5, as described by Jensen,3) Jensen and Michaelsen.4) Cases with greater trochanteric fractures involving the vastus ridge, which were classified as type A3, were excluded. All patients underwent dual-energy X-ray absorptiometry preoperatively.
Additional fixation devices were used to enhance the initial stability of the fractures in all thirty cases; fixation of the displaced fracture of the posteromedial bone fragment (21 cases of cerclage wiring and 2 cases of screw), trochanter stabilizing plates (27 cases) and antirotation screws (21 cases).
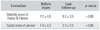
The patients were classified into two groups according to the shape of the posteromedial bone fragment. One group, indicated as group I, was composed of cases with small posteromedial bone fragment involving the lesser trochanter alone. The other group comprised of cases with large posteromedial bone fragment involving the posteroinferior cortical bone beak as well as the lesser trochanter. The former group did not require any posteromedial fixation, whereas the latter group, which required posteromedial fixation, was further divided into II, III and IV, depending on which other combinations of fixation was used. In group II, where the fracture of the posteromedial bone cortex was displaced slightly and could be reduced anatomically without a discernible gap with posteromedial fixation (all cases, cerclage wiring), a trochanter stabilizing plate (TSP) was not necessary but an antirotation screw was used. In group III, all the additional fixations (posteromedial fixation, TSP, and an antirotation screw) could be used. In the remaining cases in group IV where both a TSP and a posteromedial fixation were used, either a narrow femoral neck or the position of the lag screw precluded an antirotation screw (Table 1).
Statistical analysis was performed using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA). A paired t-test was used to compare the preoperative and postoperative conditions. A p-value ≤ 0.05 was considered significant.
All thirty fractures were treated with SHS (4CIS®, Solco Ltd, Pyeongtaek, Korea) and each additional fixation was adopted on a case by case basis. To reduce the unstable pertrochanteric femur fracture in acceptable position laterally and anteroposteriorly, the fracture was manipulated delicately with the patients lying supine on the fracture table while applying traction to the elevated thigh to prevent retroversion caused by the flexed proximal fragment. Under fluoroscopic guidance, a lateral incision was made 5 cm below the trochanteric ridge and a guide pin was inserted using a 135 angle guide.
The following methods were used to enhance the fixation of SHS. Firstly, the anteromedial cortical fracture was reduced with a bone hook and stabilized with K-wire (1.6 mm diameter) passing through the neck just abutting the lower endocortex of the femoral neck (Fig. 1A). Secondly, the wire was passed around the fractured posteromedial bone fragment and tensioned with a special tensioner. At this stage, almost complete anatomical alignment of the proximal femoral neck-shaft area could be achieved (Fig. 1B). Thirdly, a second K-wire (1.6 mm) was inserted through the upper femoral neck, parallel to the first K-wire to prevent twisting of the femoral head while inserting the lag screw (Fig. 1C). Finally, a guide pin, triple reamer and tapper were used sequentially with special care not to breach the posterolateral cortex. If the lateral cortex was compromised inadvertently, a trochanter stabilizing plate was used to buttress it (Fig. 1D).
The patients were allowed to ambulate using a wheel chair on the first postoperative day. A tilting table and parallel bar exercises were started between the third or sixth day postoperatively. From the seventh postoperative day, they were allowed to bear their weight using a four post walker or crutches as tolerably as they could.
Each patient was evaluated with the 'mobility score' reported by Parker and Palmer,5) which considered three specific factors (the patient's ability to ambulate within their residence, the ability to ambulate outside and the ability to go shopping). In addition, each patient was assigned a score for the 'social function' of Jensen:6) four points if the patients were totally dependent before the fracture, three points if moderately dependent, two points if slightly dependent, and one point if the patients were independent. Radiologically, the reduction of the fracture, degree of sliding, tip-apex distance and position of the lag screw within the femoral head were assessed. The state of the reduction was evaluated by observing the alignment and displacement using the method of Fogagnolo et al.7) both postoperatively and at the last follow-up. To be considered as anatomical, the alignment was supposed to be at a normal cervico-diaphyseal angle or in slight valgus in the anteroposterior view and have < 20° of angulation in the lateral view. The displacement of the main fragments was evaluated according to two criteria; > 80% of overlap in both planes, and < 5 mm of shortening. Cases that met both criteria were designated as good. The other cases were either acceptable if only one criterion was met or poor if neither criterion was met. After comparing the postoperative and the last follow-up radiograph, the degree of sliding was calculated by measuring the incremental change in the length from the tip of the lag screw to the lateral barrel plate. The method of Doppelt2) was adopted considering the possible error resulting from external rotation. The tip-apex distance was evaluated and measured using the method of Baumgaertner et al.8) The position of the lag screw within the femoral head was measured using the method of Cleveland et al.9) The fractures were judged to have healed when the fracture line could barely be seen because of the copious callus and sclerosis in simple roentgenogram and when there was no tenderness at the fracture site.
Eight males and 22 females with mean age of 76 years (range, 65 to 89 years) were reviewed. The minimum follow-up period was 6 months with mean follow-up period of 25 months (range, 6 to 48 months). The mean mobility and social function scores were 6.2 and 2.3, respectively, at the last follow-up (Table 2).
Postoperatively, the alignment and displacement indices were adequate in almost all the cases. The mean neck shaft angle was 135° (range, 129° to 140°) on the anteroposterior views and 10° (range, 2° to 15°) on the lateral views (Table 3). The degree of displacement was good in twenty six cases and acceptable in four.
The mean sliding of the lag screw was 5.1 mm (range, 2 to 16 mm) without any cases of cutting out at the last follow-up. The mean tip-apex distance was 6 mm (range, 3 to 11 mm) (Table 3). The lag screws were located in the center-center zone in 21 cases, inferior-center zone in 6 cases and inferior-inferior zone in 3 cases.
Bone union was achieved in all cases after surgery after an average of 18.7 weeks (range, 16 to 25 weeks). There were no cases of nonunion or malunion (Figs. 2, 3, 4, 5). Only one case of breakage of the lag screw and another case of excessive sliding accompanied by persistent hip pain were encountered.
In type 31-A2 fractures, the pertrochanteric component is mainly cortical in the anteromedial portion. Therefore, it is believed that good reduction of the anteromedial cortical fracture could reestablish bone-to-bone contact in treatment with SHS. After obtaining continuity of the anteromedial cortex, it was maintained with K-wires introduced into the femoral head temporarily. Although not perfect, this maneuver could be helpful in preventing toggling of the femoral head during insertion of the triple reamer and tapping. Carr10) also reported that the anterior and medial reduction of the intertrochanteric fractures was a simple method to obtain a stable reduction.
The posteromedial bone fragment including the lesser trochanter has been reported to be implicated in the instability of the pertrochanteric femur fractures fixed with sliding hip screws, and might cause subsequent varus deformation if not stabilized sufficiently.11-14) In seven cases (group I), in which posteromedial fixation was not achievable, the TSP alone was sufficient to obtain stability. The other twenty three cases required posteromedial fixation. In three cases (group II), cerclage wiring alone was sufficient to maintain reduction without a TSP. In both groups, an antirotation screw was also inserted for additional stability. A cancellous screw used parallel to the lag screw was reported to be helpful in preventing rotation of the femoral head portion in the early weight bearing period.15) This antirotation screw was used in twenty one cases (group I-III). Apel et al.11) showed that in unstable intertrochanteric femoral fractures, the fixation of large and small posteromedial bone fragments increased the mechanical stability by 57% and 17%, respectively. There is no general agreement regarding when to use cerclage wires or screws. Lee and Kim12) reported that the SHS with wiring of the lesser trochanter is a useful option for unstable trochanteric fractures because of its initial stability as a buttress effect on the posteromedial cortex to allow early ambulation. Kang et al.13) suggested that additional cable fixation of the lesser trochanter for treating intertrochanteric fractures including large posteromedial fragments is recommended for preventing excessive sliding of the lag screw and varus deformity. On the other hand, Johns14) used screws for fixation of the lesser trochanter fracture fragment. We prefer cerclage wires to screws for fixation of the fractured posteromedial bone fragment. Cercalge wires were used in 21 cases and a screw was used in only 2 cases. Traction was applied superolaterally by passing a wire around the inferior cortical beak of a fractured posteromedial bone fragment, and tension was achieved with a special tensioner. At this stage, the fractured posteromedial bone fragment was reduced almost anatomically and almost the original configuration of the proximal femur could be obtained in every case.
In unstable pertrochanteric fractures with a broken lateral cortex, the TSP has been reported to play an important role by preventing excessive slippage of the lag screw, lateral displacement of the greater trochanter and postoperative functional loss of the hip joint.16-20) The TSP may be helpful in preventing excessive sliding of the lag screws. The TSP combined with posteromedial fixation was used in twenty (group III, 11 cases and group IV, 9 cases) out of twenty three cases that had a large fractured posteromedial bone fragment leaving the lateral femoral cortex narrow. Six cases with a center-center position of the lag screw and three cases with a narrow femoral neck precluded the insertion of an antirotation screw (group IV). Out of the twenty cases in group III and IV, the triple reamer breached the lateral cortical buttress posteriorly in 7 cases and anteriorly 3 cases, which could be converted to type A3. Some authors also cautioned about potentially unstable pertrochanteric fracture, such as the cases mentioned in this series.16) Kim et al.17) reported that in 121 cases of unstable intertrochateric fractures treated with a compression hip screw, the TSP was used in all cases. The mean sliding was 8.4 mm and bone union was achieved in 119 cases (98.3%). Babst et al.18) concluded that in unstable intertrochanteric fractures with small or missing lateral cortical buttress, the addition of a TSP to the dynamic hip screw effectively supported the unstable greater trochanter fragment, and could prevent rotation of the head-neck fragment. Others also dealt with the role of the lateral cortical buttress in the treatment of Jensen type 4 intertrochanteric femoral fractures and it is believed that the proximal-medial fragmentary angle is a useful method for determining if additional fixation, such as the TSP, is needed.19) Palm et al.20) stated that a postoperative fracture of the lateral femoral wall was the main predictor for reoperation after an intertrochanteric fracture. Furthermore, they concluded that fractures involving the lateral wall preoperatively or having the potential for such fractures intraoperatively should not be treated with a compression hip screw alone, but should be managed using other methods.20) As shown here, the lateral cortex is also an important factor for maintaining the stability in the intertrochanteric fracture treated with the SHS.
Fractures of the greater trochanter often accompany unstable intertrochanteric fractures of the femur (type A2). In the present cases, the presence of a fractured posterior part of the greater trochanter, which did not extend to the trochanteric ridge, was always observed. Wang et al.21) noted that the recognition of the posterior wall fragment of the greater trochanter area was an important predictive factor in the treatment of unstable intertrochanteric fractures. However, since the posterior part of the greater trochanter is not the major site for insertion of the hip abductors, the fixation of its posterior fragment not involving the trochanteric ridge area did not play an important role in fracture stability in this series. The fractures of the greater trochanter involving the vastus ridge were not type A2 but type A3, which were not covered in this study. Some reported that this posterior fracture fragment can be fixed with screws to increase the stability, but we could reduce and fix this as well as the posteromedial bone fragment with one cerclage wiring alone.15) The fractured greater trochanteric fragment not involving the vastus ridge could also be supported with the addition of a TSP.
There were two cases of complication with uneventful union. One case had excessive sliding of 16 mm at the last follow-up accompanied by persistent hip pain and delayed union. Initially the posteromedial bone fragment appeared to be small without displacement, but proved to be very large with a linear fracture extending to 10 cm below the lesser trochanter (group III). Excessive sliding was unavoidable despite wiring and screw for fixation of the linear fracture line. Subsequently, the TSP was applied even in cases with a small fractured posteromedial bone fragment with a relatively broad lateral cortex for fear of an occult fracture line or fragility fracture. The other case in group II showed breakage of the lag screw with varus malunion.
Recently, many hip surgeons select intramedullary nails in the treatment of unstable pertrochanteric femur fractures. Although the intramedullary device appears to be more suitable for certain types like type A3, there is no evidence of superiority to SHS in type A2.22) Furthermore, there are even reports addressing certain drawbacks of the up-to-date model of intramedullary nails.23-25) Therefore, it is too early to discard the SHS in the management of type A2 unstable pertrochanteric femur fractures. Additional fixations were used in thirty cases with unstable pertrochanteric femur fractures (type A2) treated with SHS. The average time to union was 18.6 weeks and only two complications, breakage of the lag screw and excessive sliding accompanied by persistent hip pain, were encountered. Although the cohort of this study was small, this study suggests relatively reproducible guidelines for the use of additional fixation in the treatment of unstable pertrochanteric femur fractures (type A2) with SHS.
Figures and Tables
Fig. 1
Steps in the surgical procedure. (A) Achievement and maintenance of anteromedial cortical continuity with a K-wire. (B) Wiring of the posteromedial bone fragment to obtain anatomical alignment. (C) A second K-wire to prevent toggling of the femoral head while inserting the lag screw. (D) Anatomical reduction and fixation of type A2 pertrochanteric femur fracture using both the sliding hip screw and three additional fixation devices.

Fig. 2
Group I. (A) Preoperative radiograph of a 65-year-old male showing AO type 31-A2, pertrochanteric femur fracture with a small posteromedial bone fragment with comminution. (B) Immediate postoperative radiograph showing anatomical alignment. (C) Eight months postoperative radiograph showing callus formation.

Fig. 3
Group II. (A) Preoperative radiograph of an 80-year-old male showing AO type 31-A2, pertrochanteric femur fracture with a large posteromedial bone fragment. (B) Immediate postoperative radiograph showing anatomical reduction. (C) Six months postoperative radiograph showing union.

Fig. 4
Group III. (A) Preoperative radiograph of a 74-year-old female showing AO type 31-A2, pertrochanteric femur fracture with a large posteromedial bone fragment. (B) Immediate postoperative radiograph showing anatomical alignment. (C) Fifteen months postoperative radiograph showing union.

Fig. 5
Group IV. (A) Preoperative radiograph of a 70-year-old female showing AO type 31-A2, pertrochanteric femur fracture. The large posteromedial bone fragment has a linear fracture bisecting it horizontally. (B) Immediate postoperative radiograph shows anatomical alignment with the large posteromedial bone fragment well reduced and fixed with cerclage wiring. (C) Seven months postoperative radiograph shows uneventful bone union despite the upper part of posteromedial fragment displaced upwardly. The anteromedial cortex was reformed without a visible step-off and the wired inferior cortical beak was well maintained anatomically. These two factors contributed to the stability until union.

References
1. Pervez H, Parker MJ, Pryor GA, Lutchman L, Chirodian N. Classification of trochanteric fracture of the proximal femur: a study of the reliability of current systems. Injury. 2002. 33(8):713–715.

2. Doppelt SH. The sliding compression screw: today's best answer for stabilization of intertrochanteric hip fractures. Orthop Clin North Am. 1980. 11(3):507–523.

4. Jensen JS, Michaelsen M. Trochanteric femoral fractures treated with McLaughlin osteosynthesis. Acta Orthop Scand. 1975. 46(5):795–803.

5. Parker MJ, Palmer CR. A new mobility score for predicting mortality after hip fracture. J Bone Joint Surg Br. 1993. 75(5):797–798.

6. Jensen JS. Determining factors for the mortality following hip fractures. Injury. 1984. 15(6):411–414.

7. Fogagnolo F, Kfuri M Jr, Paccola CA. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch Orthop Trauma Surg. 2004. 124(1):31–37.

8. Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995. 77(7):1058–1064.

9. Cleveland M, Bosworth DM, Thompson FR, Wilson HJ Jr, Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959. 41(8):1399–1408.

10. Carr JB. The anterior and medial reduction of intertrochanteric fractures: a simple method to obtain a stable reduction. J Orthop Trauma. 2007. 21(7):485–489.

11. Apel DM, Patwardhan A, Pinzur MS, Dobozi WR. Axial loading studies of unstable intertrochanteric fractures of the femur. Clin Orthop Relat Res. 1989. (246):156–164.

12. Lee JM, Kim KY. Treatment of unstable trochanteric fracture using sliding hip screw with wiring of lesser trochanter. J Korean Orthop Assoc. 2000. 35(6):861–866.

13. Kang JS, Moon KH, Kim RS, Bae JH, Lee BC. Fixaton of lesser trochanteric fragments on an unstable intertrochanteric fracture of the femur. J Korean Hip Soc. 2009. 21(3):245–251.

14. Jones JB. Screw fixation of the lesser trochanteric fragment. Clin Orthop Relat Res. 1977. (123):107.

15. Kim JH, Park JH, Kim HS, et al. Methods to increase the effectiveness of trochanteric stabilizing plate for unstable femoral intertrochanteric fractures with greater trochanteric fracture: fixation of greater trochanter with wire and screw. J Korean Hip Soc. 2007. 19(1):58–63.

16. Im GI, Shin YW, Song YJ. Potentially unstable intertrochanteric fractures. J Orthop Trauma. 2005. 19(1):5–9.

17. Kim DO, Jung JH, Yoon KS. Treatment of unstable intertrochanteric fracture using short barrel compression hip screws and a trochanteric stabilizing plate. J Korean Orthop Assoc. 2010. 45(2):101–106.

18. Babst R, Renner N, Biedermann M, et al. Clinical results using the trochanter stabilizing plate (TSP): the modular extension of the dynamic hip screw (DHS) for internal fixation of selected unstable intertrochanteric fractures. J Orthop Trauma. 1998. 12(6):392–399.

19. Kim YS, Kwon SY, Han SK, Choi WH, Choi NY. The role of lateral buttress in treatment of Jensen type 4 intertrochanteric fractures of the femur using dynamic compression hip screw in the elderly. J Korean Orthop Assoc. 2005. 40(7):935–941.

20. Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P. Hip Fracture Study Group. Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. J Bone Joint Surg Am. 2007. 89(3):470–475.

21. Wang L, Shon SK, Lee KY, et al. Classification and treatment of unstable intertrochanteric fracture according to the existence of posterior fragment: preliminary report. J Korean Fract Soc. 2008. 21(2):110–116.

22. Karunakar M, McLaurin TM, Morgan SJ, Egol KA. Improving outcomes after pertrochanteric hip fractures. Instr Course Lect. 2009. 58:91–104.
23. Brunner A, Jockel JA, Babst R. The PFNA proximal femur nail in treatment of unstable proximal femur fractures: 3 cases of postoperative perforation of the helical blade into the hip joint. J Orthop Trauma. 2008. 22(10):731–736.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download