The number of patients with knee osteoarthritis has significantly increased in the recent years. High tibial osteotomy (HTO) as a treatment for knee osteoarthritis was first reported on by Jackson in 1958 and it was popularized by Coventry.1) HTO is an accepted surgical technique for the treatment of medial compartmental arthrosis of the knee in younger patients.2)
Selection of the appropriate patients, extensive preoperative planning and accurate surgical technique are essential for the successful outcome of osteotomy. The methods for HTO include open wedge osteotomy and closed wedge osteotomy. An open wedge osteotomy has become increasingly popular compared to the other technique. This procedure is advantageous compared with a closed wedge osteotomy because the peroneal nerve is not in jeopardy, there is no disruption of the proximal tibiofibular joint and lateral ligaments and it can achieve a more precise correction.3)
This paper describes the surgical technique for performing open wedge HTO with using an Aescula open wedge plate (B.Braun, Aesculap) and an allogenic bone graft. We present the postoperative clinical results from a series of patients who underwent this operation, and we also review the relevant medical literature.
METHODS
Patient Selection
From March 2007 to August 2007, 33 patients (37 cases) were treated with an open wedge HTO using an Aescula open wedge plate and an allogenic bone graft by the senior author (KAJ). The study group included twenty nine women and four men with a mean age of 53 years (range, 42 to 61 years). The exclusion criteria for this procedure were symptomatic osteoarthritis of the patellofemoral joint and lateral compartment, rheumatoid arthritis, a history of fractures or previous open surgery of the lower limb, and flexion contracture. The mean follow-up duration was 15.6 months (range, 12 to 18 months).
Clinical and Radiographic Assessment
The clinical assessments included an evaluation of the knee joint function using the knee and function scores based on the Knee Society Score, and the complications such as infection, nonunion and peroneal nerve palsy. The standardized radiography of the knee included the lower extremity scannogram (the standing anteroposterior view including the hip, knee and ankle joint), both knee standing posteroanterior 45° flexion views, both knee standing anteroposterior views and a true lateral radiograph with the knee in 30° of flexion. The pre-operative lower extremity scannogram was used to calculate the weight bearing line (WBL) percentage at the tibial intersection. The denominator was the width of the tibia, and the numerator was the tibial intersection of the WBL (with the medial tibial edge at 0% and the lateral tibial edge at 100%). The methods for determining the correction wedge preoperatively were the same as those previously described by Dugdale et al.4) The WBL was calculated to pass through the lateral tibial plateau at 62% of the width of the plateau if a two or three degrees of valgus overcorrection was required. A radiographic assessment was performed using the radiography of the lower extremity scannogram, where the femoro-tibia angle was measured using the method reported by Bauer et al.,5) and the mechanical axis of the lower extremity was the angle between the femoral and tibial mechanical axis (physiological range, 0 to 2.2° of valgus).6) The joint space distance was measured as follows. A line was drawn parallel to the both femoral condyles and a second line was parallel to both the tibial condyles. A perpendicular line from the lowest point of the femoral condyle to the tibial condyle line was drawn. The length of this perpendicular line was the joint space distance. Therefore, the degree of joint space loss and the postoperative recovery of the joint space were indirectly evaluated.7) The posterior tibial slope was assessed on the lateral X-ray. The tibial shaft axis was calculated by using a previously described technique,8) in which 2 points were identified halfway between the anterior and posterior cortices and a line drawn through those points. The tibial plateau was measured from the line of best fit on the lateral radiograph with using the medial tibial plateau. The tibial slope was the angle formed between the proximal plateau and a line drawn perpendicular to the tibial shaft axis. The Insall-Salvita (IS) ratio was calculated by dividing the length of the patellar ligament by the length of the patella.9)
The clinical indicators we used to assess union were the complaints of pain as well as the signs of tenderness, warmth and swelling at the osteotomy site. The radiographic examinations involved the anteroposterior (AP), lateral and oblique radiographs of the osteotomy site. The indicators used to assess bone union were the increasing density of the graft on the serial examination and bone bridging across the wedge opening. The signs of nonunion were the absence of the above indicators at 6 months after surgery and sclerotic margins at the periphery of the wedge opening.
Statistical comparisons between the pre- and post-operative data (at the last follow-up) were performed using a paired sample t-test (SPSS ver. 13.0; SPSS Inc., Chicago, IL, USA). A p-value < 0.05 was considered significant.
Surgical Technique
An arthroscopic examination was carried out for all the cases, which confirmed the status of the cartilage and the concurrent presence of damage. Chondroplasty and a partial meniscectomy were performed for the cases where there was damage to the articular surface or the meniscus was present.
After the arthroscopy, the anteromedial aspect of the tibia was exposed through a 6 cm vertical skin incision, and a sharp dissection was performed to expose the deep fascia over the pes anserineus, which was retracted distally using a periosteal elevator to expose the superficial fibers of the medial ligament (Fig. 1). A blunt Hohmann retractor was then passed deep to the medial collateral ligament around the posteromedial corner of the proximal tibia, and also along the posterior cortex of the tibia to protect the posterior neurovascular structures. For a biplanar medial open wedge osteotomy,10) two Kirschner wires were placed under fluoroscopic guidance to mark the saw cut. The start point on the medial tibia is normally approximately 3-4 cm distal to the medial joint line. The anteroposterior plane of the osteotomy should be in the same plane as the tibial slope. The lateral aiming point was the upper third of the proximal tibiofibular joint. Behind the tibial tuberosity, the osteotomy was performed with using a thin osteotome to protect the patellar tendon in a plane parallel to the anterior cortex of the tuberosity. A tibial osteotomy was performed just distal to the guide pin, initially with an oscillating saw and then with a thin osteotome. The extent of the osteotomy was checked by fluoroscopy to ensure an appropriate depth and direction of the cut (up to 1 cm medial to the lateral cortex). Opening of the osteotomy and adequate correction in the coronal plane were confirmed by placing a rod from the center of the hip joint to the center of the ankle joint (the weight bearing axis) under fluoroscopic guidance. The rod should be located at 62% of the tibial width and just lateral to the lateral tibial spine.4) The tibial slope was controlled using two plates with different sized space blocks (B. Braun, Aesculap) (Fig. 2). First, a properly sized open wedge plate with a space block was inserted posteromedially with gentle valgus force. The tibial slope was identified on the fluoroscopic image after placing the first plate within the posteromedial osteotomy gap. The anterior plate was placed behind the oblique tuberosity osteotomy and the anterior plate was 2 to 4 mm shorter depending on the size of the posterior plate. The fluoroscopic image was then compared with the preoperative radiographic image. Osteosynthesis was performed as follows. Two screws were applied to the first plate that was placed posteromedially. A smaller plate was then inserted within the anteromedial gap and locked with another two screws. A final fluoroscopic assessment was performed to ensure proper alignment of the lower extremities and adequate positioning of the open wedge plate. An allogenic bone graft was then inserted within the osteotomy gap. In each case, a proximal tibial corticocancellous wedge allograft (hemi-femoral head) and cancellous pieces (Fig. 3) were provided by the Musculoskeletal Transplant Foundation (the Korean Bone Bank). The wedge (ordered to match the size of the predetermined osteotomy opening and it was made up of the medial calcar portion of allogenic bone) was then measured and cut to precisely fill the osteotomy defect. Cancellous pieces were then inserted into the posteromedial (the same size of space block as the Aescula plate) and middle areas of the ostotomy tines, and a corticocancellous piece was inserted into the anterior area between the plates (Fig. 4). In addition, a careful radiographic evaluation of the lateral hinge bone was used to detect the presence of any fracture. If there was a fracture, then supplementary lateral fixation with a 6.5 mm cannulated screw or staple was carried out. The wound was closed with leaving a hemovac drain; the wound was dressed with a compression wrap and a long-leg splint was applied.
Postoperative Protocol
The postoperative protocol included quadriceps and range-of motion exercises on the first day after surgery to obtain knee motion. A long leg cylinder cast was applied three to four weeks after surgery and partial weight-bearing was then started. This was followed by full weight-bearing eight weeks after surgery. The cast was removed after no changes in the opening angle of the osteotomy site were noted with full weight-bearing (Fig. 5).
RESULTS
Clinical Results
The mean knee score significantly improved from 52.19 ± 11.82 preoperatively to 92.49 ± 5.10 at the last follow-up (p < 0.001). The mean functional score significantly improved from 52.84 ± 6.23 preoperatively to 89.05 ± 5.53 at the last follow-up (p < 0.001).
Radiographic Results
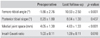
The femoro-tibia angle, which was measured using Bauer's method,5) had a mean varus of -1.86 ± 2.76° preoperatively. This was corrected to a mean valgus of 10.93 ± 2.50° at the final follow-up (p < 0.001). The mechanical axis of the lower extremity showed a mean varus of -7.34 ± 2.86° preoperatively. This was corrected to a mean valgus of 4.38 ± 2.30° at the final follow-up (p < 0.001). The mean posterior tibial slope was 8.20 ± 1.80° preoperatively and 8.04 ± 1.30° at the final follow-up (p = 0.437) (Fig. 4). The mean joint space distance increased from 4.05 ± 1.30 mm pre-operatively to 4.83 ± 1.33 mm at the final follow-up (p < 0.001). The pre- and postoperative Insall-Salvati ratios were 1.03 ± 0.11 and 1.09 ± 0.11, respectively (p = 0.018) (Table 1). The time needed to achieve complete clinical and radiographic bone union was 12.69 ± 1.5 weeks.
Complications
No complications were encountered, such as delayed union, nonunion, superficial infection, deep infection, skin necrosis, peroneal nerve and vascular injury. There was one case of skin irritation due to screw back-out (Fig. 6). However, this was resolved after removing the plate and screws after bone union.
DISCUSSION
The methods for performing HTO include a closed and open wedge osteotomy. The open wedge osteotomy has attracted increasing interest in recent years because it avoids incurring neurological complications, such as peroneal nerve palsies,11) and this technique can overcome the difficulties associated with a total knee arthroplasty after a closed wedge osteotomy.12)
The theoretical advantages of an open wedge over closed wedge include restoration of the anatomy with the addition of bone to the diseased medial side, the ability to achieve a predictable correction in the coronal and sagittal planes, the ability to intraoperatively adjust the correction, the requirement for only a single bone cut and the relative ease of combining this technique with other procedures, such as anterior cruciate ligament (ACL) reconstruction.13) Koshino et al.14) examined 21 knees that were treated with an open wedge HTO with using a hydroxyapatite wedge as a bone-graft substitute. The mean Hospital for Special Surgery score of the knees treated with an open wedge HTO was superior to that in their previous study of knees15) treated with a closed wedge procedure. However, a review of literature favors a closed wedge osteotomy.16-18) A closed wedge osteotomy is done through the cancellous bone, which would minimize the chances of delayed union or nonunion. A closed wedge osteotomy is an excellent operative option with a long record of clinical success and it has minimum chances of nonunion. The osteotomy that's done close to the joint line ensured the more accurate correction of deformity. Aglietti et al.16) described excellent and good results, after at least ten years, for 64% of the patients who underwent closed wedge osteotomies, and Rudan and Simurda19) had good and excellent results in 14 the 20 patients (70%) who were followed up for longer than ten years after they underwent closed wedge osteotomies.
Based on our experience, an open wedge HTO has many advantages over a closed wedge HTO. A tibial osteotomy performed along a biplanar line is a simple procedure. Moreover, internal fixation is easily accomplished easily with using two metal plates and four screws. Furthermore, this procedure is less invasive than a closed wedge HTO and it can be performed on elderly patients. Because wedges are inserted in the osteotomy site during the open wedge HTO, the leg length after this procedure may be slightly greater than that after a closed wedge HTO. Therefore, in order to avoid a leg-length discrepancy, an open wedge osteotomy should be performed on the contralateral side for the case of a patient with an open wedge osteotomy in one knee and who requires surgical treatment of the contralateral knee.
The tibial slope is an important parameter that influences the knee biomechanics. The proximal anteromedial tibial cortex has an oblique or triangular shape when viewed in cross section, whereas the lateral tibial cortex is almost perpendicular to the posterior margin of the tibia. Because of this configuration, an open wedge osteotomy with an anterior tibial tubercle gap equal to the gap at the posteromedial crest would increase the tibial slope, alter the femoro-tibial contact point, decrease the knee extension and potentially increase the ACL tensile load.8,20,21) In contrast, closed wedge osteotomy decreases the posterior tibial slope.22) Dejour and Bonnin23) reported that increasing the tibial slope caused an increase in anterior tibia translation and they suggested there were increased tensile loads on the ACL and posterior cruciate ligament (PCL). They recommended decreasing the posterior tibial slope in ACL-deficient knees if it exceeded 10°. It is important to maintain the posterior tibial slope after an osteotomy. Noyes et al.8) reported that the anterior osteotomy gap required at the tibial tubercle to maintain a normal sagittal tibial slope (based on pre-operative and intra-operative calculations using the three triangle method) is generally one half of the posteromedial gap. In our series, different sized wedge plates and a posteromedial cancellous piece were used to maintain a natural tibial slope. The larger first wedge plate was routinely placed within the posteromedial gap with an adequate valgus correction angle under fluoroscopic guidance, and this was followed by the insertion of a similar sized cancellous piece of space block of an Aescula plate. The postoperative tibial slopes showed almost no change compared with the preoperative values, and we obtained consistent and reproducible results. Fujisawa et al.7) confirmed that the joint space recovered when the destroyed articular cartilage of the knee joint had regenerated.
There is considerable controversy regarding the ideal valgus correction angle. Insall et al.24) reported that a postoperative valgus position ranging from 5 to 14° was acceptable. It is probably better to err on the valgus side of this spectrum, even though a noticeable valgus position might be cosmetically unacceptable to the patient, and particularly if the varus angulation of the contralateral knee creates a so-called wind-blown appearance. Coventry and Bowman25) recommended that an overcorrection of a normal 5° of anatomical valgus improves the long-term results. The precise effects of the various amounts of overcorrection have not been reported on. However, too much valgus angulation may not only overload the lateral compartment, but it might also be cosmetically undesirable. Over the years, surgeons and researchers have reached a compromise and they strive to obtain between 7 to 10° of valgus angulation. When performing a univariate analysis of the risk factors for failure related to angular correction, Coventry et al.18) confirmed that the knees with less valgus correction had a higher risk of failure and there was a lower risk of failure for those knees with more correction. Agneskirchner et al.26) reported that by simulating a varus deformity (0% off set of the loading axis with the medial border of the knee joint), the intra-articular pressure in the medial compartment exceeded that of the lateral compartment by approximately 45%. Gradually shifting the loading vector laterally decreased the medial pressure and it increased the lateral pressure. Interestingly, when in the neutral position (50%, straight leg), somewhat higher pressures were recorded laterally than medially, which corresponds well with the existing data. In the valgus positions (62% and 75%), the lateral pressure values exceeded the medial pressure by 30% to 40%. In our series, the knees were overcorrected by 4-5° for approximately achieving 6° of the normal femoro-tibial angle. Thus, the femoro-tibial angle was set to 10-11°.
Wright et al.27) reported that the height of the patellar bone was decreased in all the cases that underwent proximal tibial osteotomy. This was explained by the articular surface being remote from the tibial tubercle due to the open osteotomy. Noyes et al.28) also reported that the decreased height of the patellar bone was observed at an incidence of 80%, but they noted that the degree of the corrective angle did not affect the decreased height of the patellar bone. This was explained by the phenomenon that the degree of anterior distraction at the site of the osteotomy is not higher than that of an anterior distraction. In addition, in our series, there was no case of a decreased length of the IS ratio associated with patella infra syndrome.
Time-dependent worsening of the clinical results was has been in a long-term follow-up study, and the study was carried out to examine the patients' satisfaction with a HTO. There are some cases in which a total knee arthroplasty must be performed because of the time-dependent progression of lesions after surgery and the recurrence of pain due to the loss of the corrective angle. Compared with total knee arthroplasty, a HTO has advantages such as a simplified surgical technique, a lower surgical cost and a lack of limitations in the flexion motion after surgery (leading to a wider range of motion). In particular, rigorous use of a HTO and hypercorrection will still be useful for treating degenerative knee arthritis when considering the serious complications that can develop after total knee arthroplasty, such as osteolysis or wear.29)
There were some limitations to this study. These results would be supported by the clinical and radiologic outcomes with a longer term of follow-up and with more patients. However, it is believed that good clinical and radiologic result can be expected, based on the established relationship between pain relief and the accuracy of correction.
Performing open wedge HTO with an Aescula open wedge plate and an allogenic bone graft was effective for obtaining a satisfactory correction angle for the treatment of osteoarthritis accompanied by a varus deformity. In addition, this procedure recovered the joint space and enhanced the function of the knee joint. Furthermore, it allowed early-stage joint movement and weight-bearing after obtaining early bone union, and it was effective in preventing the posterior tibial slope. However, these results need to be confirmed by conducting a long-term follow-up study.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download