Abstract
A 24-year-old man with tuberculosis meningitis developed acute paraplegia and sensory disturbances 5 weeks after receiving conventional antituberculous therapy. Magnetic resonance imaging revealed an intradural extramedullary long segmental mass mimicking en plaque meningioma at the T2-T6 vertebrae levels. Prompt surgical decompression was performed. A histology examination of the mass revealed a tuberculoma. After surgery, the patient showed improved motor power and a normal bladder function. Intradural extramedullary tuberculoma of the spinal cord is rare complication of tuberculosis meningitis, which can occur as a response to conventional antituberculous therapy.
Tuberculosis is still an important pathological entity in developed and developing countries. Central nervous system involvement in patients with tuberculosis is estimated to be approximately 10% with tuberculous meningitis being the most common manifestation.1-3) Spinal tuberculoma is also an extrapulmonary manifestation of tuberculosis involving the central nervous system, and are characterized as extradural, intradural extramedullary, or intradural according to their location. In particular, an intradural extramedullary tuberculoma is extremely rare. Only 30 cases reports have been found in the literature.3-9)
We describe an unusual case of intradural, extramedullary tuberculoma mimicking en plaque meningioma as a complication of tuberculous meningitis in a previously healthy human immunodeficiency virus (HIV)-negative young male.
A 24-year-old male was admitted to our hospital with a 1 week history of progressive headache and fever. His previous medical history was clear. On the neurologic examination, his mental status was normal without focal neurological deficits. The laboratory examination revealed nonspecific findings. HIV antibodies were negative. Lumbar cerebrospinal fluid (CSF) analysis showed pleocytosis, increased total protein level (167 mg/dL) and decreased glucose (32 mg/dL). Tubercle bacillus was detected in the CSF and the adenosine deaminase (ADA) level was elevated (12 IU/L). Brain MRI revealed small, multiple high signal intensity lesions on the diffusion weighted image. His chest X-ray showed diffuse ill-defined patches and nodules with increased density in both apical lungs. Tuberculosis meningitis and pulmonary tuberculosis were suspected and antituberculous treatment with rifampicin, isoniazid, ethambutol and pyrazinamide was started. Nine days after the antituberculous treatment, his general condition and headache had improved significantly. However, four weeks after antituberculous treatment, he developed acute sensory disturbance below T10 dermatome as well as urination disturbances. A neurological examination revealed grade 3/3 paraparesis and hyporeflexia. Spinal MRI showed a long segmentally located soft tissue mass mimicking a meningioma in the intradural, extramedullary space of the posterior spinal canal from T2 to T6 with severe cord compression and displacement (Fig. 1). Surgical decompression and a biopsy were performed. During the operation, a T3, T4, T5 and T6 laminectomy was performed. The dura was thickened and the cord was infiltrated with an adhesive mass. The dura was opened and closed in the normal manner after removing the mass under microscope guidance. Grossly, the mass was very soft with a dark green color. Optical microscopy of the mass revealed chronic granulomatous inflammation with neutrophil infiltration (Fig. 2). The cultures were negative for Mycobacterium tuberculosis, and the stains for fungi and acid-fast micro organisms were negative. Twelve weeks after surgery, the patients reported low back discomfort. MRI of the thoracic and lumbar areas showed lumbosacral tuberculosis spondylitis with multiple abscesses (Fig. 3). Anti-tuberculous medication was continued for 18 months. At the one year follow-up, the patient could walk without assistance and urinate normally.
Spinal involvement in tuberculosis is classified into four categories: Potts spine, nonosseous spinal tuberculoma, tuberculous arachnoiditis and tuberculous meningitis. Intradural spinal tuberculomas are estimated to be composed of only 2% to 5% of central nervous system tuberculomas.1,3-5)
Compton and Dorsch8) reported 11 cases of intratudral extramedullary tuberculoma in 1984. Since then, there have been 19 more cases reported in the English literature.1,3,5-9) All cases, except for 4 initially presented with tubculous meningitis. Most case reviews involved the thoracic spine.1,3,5-10) The diagnostic method is generally histopathology, even though AFB cultures from the granulomas were positive in only one of the reported cases.7) A myelogram can be helpful but MRI is the diagnostic procedure of choice.
Interestingly, most intradural extramedullary tuberculoma cases were detected after antibuberculous therapy had been initiated, which is known as paradoxical response.2,4,7)
Tuberculoma can occur at any time but most reported cases showed a paradoxical response during the early course of chemotherapy, which ranged from 3 weeks to 1 year.2,4,7) The mechanism for the paradoxical response is unclear. However, is is believed to be the result of an interaction between the host's immune response and the direct effects of mycobacterial products.2,3,7,10) This condition has been recognized more frequently. Narita et al.10) reported paradoxical worsening in up to 36% of patients with tuberculosis and AIDS after antiretroviral therapy. Hydrocephalus and new granuloma can appear despite regular chemotherapy. Therefore, mental or focal neurological changes during the follow-up must be checked in patients with tubeculous meningitis.2,10)
The prognosis for neurological improvement is good with a prompt surgical excison and appropriate antituberculous medication.3,4,6) Although intramedullary tuberculoma can be treated with medication alone, an intradural extramedullary tuberculoma is essential for surgery when compression of spinal cord occurs.
En plaque meningioma can present with thoracic spinal cord and nerve root compression.1) The case presented herein was initially diagnosed with en plaque meningioma based on the radiological findings. The differential diagnosis between tuberculous patchy meningitis and meningioma in the form of plaque is difficult without obtaining a biopsy specimen.
In conclusion, intradural extramedullary tuberculoma can occur in tuberculous meningitis patients as a paradoxical response to antituberculous chemotherapy. Although quite rare, intradural extramedullary tuberculomas should be considered in a differential diagnosis of an en plaque meningioma of the spinal cord.
Figures and Tables
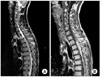
Fig. 1
T2-weighted sagittal (A) and enhanced T1-weighted sagittal (B) section of magnetic resonance imaging scan of a thoracic spine,showing an intradural extramedullary mass extending from T2 through T6 and compressing the spinal cord.
References
1. Mirzai H. Tuberculoma of the cervical spinal canal mimicking en plaque meningioma. J Spinal Disord Tech. 2005. 18(2):197–199.

2. Kumar R, Prakash M, Jha S. Paradoxical response to chemotherapy in neurotuberculosis. Pediatr Neurosurg. 2006. 42(4):214–222.

3. Luo L, Pino J. An intradural extramedullary tuberculoma of the spinal cord in a non-HIV-infected patient: case report and review of the literature. Lung. 2006. 184(3):187–193.

4. Skendros P, Kamaria F, Kontopoulos V, Tsitouridis I, Sidiropoulos L. Intradural, eextramedullary tuberculoma of the spinal cord as a complication of tuberculous meningitis. Infection. 2003. 31(2):115–117.

5. Roca B. Intradural extramedullary tuberculoma of the spinal cord: a review of reported cases. J Infect. 2005. 50(5):425–431.

6. Kumar R, Kasliwal MK, Srivastava R, Sharma BS. Tuberculoma presenting as an intradural extramedullary lesion. Pediatr Neurosurg. 2007. 43(6):541–543.

7. Takahashi H, Ito S, Kojima S, Tanno T, Hattori T. Intradural extramedullary tuberculoma of the thoracic spine: paradoxical response to antituberculous therapy. Intern Med. 2008. 47(8):797–798.

8. Compton JS, Dorsch NW. Intradural extramedullary tuberculoma of the cervical spine: case report. J Neurosurg. 1984. 60(1):200–203.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download