Abstract
Background
Bipolar hemiarthroplasty for unstable intertrochanteric fractures in elderly patients is a viable option that can prevent the complications of an open reduction, such as nonunion and metal failure. This study evaluated the clinicoradiological results of cementless bipolar hemiarthroplasty for unstable intertrochanteric fractures in elderly patients.
Methods
Forty hips were followed for more than 2 years after cementless bipolar hemiarthroplasty using a Porocoat® AML Hip System. The mean age was 78.8 years and the mean follow-up period was 40.5 months. The Harris hip score and postoperative hip pain were analyzed clinically. The radiological results were assessed using a range of indices.
Results
At the last follow-up, the mean Harris hip score was 80.6 points. There were one case of hip pain and one case of thigh pain. Twenty-four cases (60%) showed no decrease in ambulation capacity postoperatively. Radiologically, there were 23 cases (57.5%) of fixation by bone ingrowth and 17 cases (42.5%) of stable fibrous fixation. There were no cases of osteolysis. Eleven cases (27.5%) of new bone formation were found around the stem. All stems were stable without significant changes in alignment or progressive subsidence.
Intertrochanteric fractures with severe displacement or comminution are common in elderly patients with poor bone quality and are often associated with complications, such as nonunion, metal failure and femoral head perforation.1,2) Hemiarthroplasty, which allows rapid rehabilitation is performed as an alternative to osteosynthesis in elderly patients with unstable intertrochanteric fractures.3,4)
There is some controversy regarding the use of cement for the fixation of femoral implants. Cemented fixation is advantageous for enhancing the initial fixation strength in aged patients with poor bone quality,5) whereas cementless fixation facilitates biological fixation and can avoid cardiovascular toxicity.6) Some studies reported positive outcomes of arthroplasty using cementless implants in elderly patients with an improvement of the implant design, material and insertion technique.4,7)
This study evaluated the clinical and radiological outcomes of bipolar hemiarthroplasty in patients over 70-year-old with unstable intertrochanteric fractures. In all cases, cylindrical extensively porous-coated implants, which were designed to be fixed to the proximal and isthmic areas, were used considering the lack of good bony support in the proximal portion.
Cementless bipolar hemiarthroplasty using the anatomic medullary locking (AML) femoral stem (Depuy, Warsaw, IN, USA) was performed on forty-five patients with intertrochanteric fractures, aged 70 and over, and were able to walk either with or without an aid prior to surgery at our institution between January 2000 and December 2005. Of these patients, 40 patients who could be followed up for ≥ 2 years were included in this study. The patients had unstable fractures according to the Evans classification. The surgical indications were severe osteoporosis (≤ grade 3 Singh index8)) and comminution of the medial cortical bone (A2 according to the AO classification), which are associated with high rates of internal fixation failure.
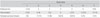
Their mean age was 78.8 (range, 70 to 95 years). There were 32 females (80%) and 8 males (20%). The mean follow-up period was 40.5 months (range, 24 to 62 months). The mean time from fracture to surgery was 7 days. Surgery was performed within 1 week after injury in 35 patients (87.5%). Thirty-four patients (85%) had combined diseases: 18 patients (45%) had hypertension and the remaining patients had diabetes, cardiovascular diseases, cerebrovascular diseases, and lung diseases (Table 1).
Surgery was performed by the first author in all cases. Under general or spinal anesthesia, a cementless AML 5/8 porous-coated femoral stem (Depuy) was inserted using the anterolateral approach. A bipolar cup and a 28 mm femoral head (Depuy) were used in all patients. Proximal fixation of the implant was reinforced with the additional fixation of trochanteric fragments around the proximal stem. Wires or nonabsorbable sutures were used for fixation depending on the size of the fragment.
Quadriceps femoris muscle strengthening exercises were started from one day after surgery. In all patients, partial weight bearing with crutch walking and full weight bearing was started at 1 week and within 3 months after surgery, respectively. Postoperative occurrence of an embolism was confirmed in the patients presenting with chest pain or shortness of breath using blood tests including arterial blood gas analysis and chest computed tomography.
The Harris hip scores9) at the last follow-up were classified into four categories; excellent (90 to 100), good (80 to 89), fair (70 to 79), and poor (60 to 69). The level of pain in the groin and thigh after surgery was divided into 3 grades; mild, moderate, and severe. The changes in walking ability from before to after surgery were investigated. The activities of daily living10) were graded into 4 categories; excellent (no pain or limitation of movement), good (slight pain or limitation of movement not interfering with walking and personal hygiene), fair (moderate pain or limitation of movement requiring assistance in walking), and poor (severe pain, limitation of movement or poor general condition that made walking impossible).
The initial fixation of the femoral stem was assessed in the proximal and isthmic areas on the radiographs taken immediately after surgery. The proximal canal fit was rated good if the stem filled the proximal canal by more than 80%, and the press fit at the isthmus level was considered good when a gap of < 1 mm was noted between the stem and inner cortex.11,12)
The femoral stem stability was classified into fixation by bone ingrowth, stable fibrous fixation, and unstable prosthesis according to the criteria of Engh et al.13,14) The changes in the alignment and subsidence of the femoral components were measured from after surgery to the last follow-up; ≥ 3° of valgus or varus and ≥ 5 mm longitudinal change were considered significant.3,10) The radiolucent line, bone resorption, endosteal new bone formation and osteolysis were examined in the seven zones described by Gruen et al.15) A radiolucent line denoted the radiolucent area around the stem surrounded by radiodense lines, and was considered present if it occupied ≥ 50% of any zone.16) Loosening of the femoral stem was defined as the appearance of a radiolucent line progressive or > 1 mm in all zones, or the presence of continuous subsidence or migration of the femoral stem.
The mean Harris hip score at the last follow-up was 80.6 ± 9.3. Better than fair results were obtained in 27 patients (67.5%); excellent in 8 (20.0%), good in 19 (47.5%), fair in 9 (22.5%), and poor in 4 (10.0%). Groin pain and thigh pain were noted in 7 patients (17.5%) and 5 patients (12.5%), respectively, but significant pain requiring medication was noted in one patient in each area (2.5%).
Of the 40 patients, 11 (27.5%) and 29 (72.5%) patients could walk with and without support before surgery, respectively. Of the 29 patients, 17 could still walk without support after surgery, but 11 required assistance and one was unable to walk. Of the 11 patients who could walk with support before surgery, six showed no difference after surgery, four patients who had used a cane before surgery became more dependent on walking aids and one could not walk due to a poor general condition after surgery. Overall, 24 (60%) out of 40 patients regained their preoperative walking ability (Table 2). Twenty-three patients (57.5%) could carry out their daily living activities and personal hygiene after surgery; 6 (15.0%), 17 (42.5%), 13 (32.5%), and 4 (10%) patients had excellent, good, fair and poor results, respectively.
According to the radiological findings, a press-fit was achieved either at the proximal area or the isthumus in all patients; the proximal canal fit, the press fit at the isthmus and both were achieved in 18 (45%), 12 (30%) and 10 (25%) patients, respectively (Fig. 1). The stability of the femoral stem at the last follow-up according to the criteria of Engh et al.13,14) was fixation by bone ingrowth in 23 patients (57.5%) and stable fibrous fixation in 17 patients (42.5%); there were no unstable prostheses. A radiolucent line was observed in five patients (12.5%) and mainly in Gruen zones 1 and 7; in zone 1 in three patients (7.5%) and in zone 7 in four patients (10%) (Table 3). Endosteal new bone formation was observed in 15 patients (37.5%), mainly in Gruen zones 2, 3, 4, 5, and 6: two (5%), seven (17.5%), twelve (30%), nine (22.5%), nine (22.5%), six (15%), and one patient (2.5%) in zones 1, 2, 3, 4, 5, 6, and 7, respectively (Table 3). Bone resorption was noted in 23 patients (57.5%) and mostly in Gruen zones 1, 2, 6 and 7: six (15%), four (10%), two (5%), one (2.5%), five (12.5%), and eight patients (20%) in zones 1, 2, 3, 4, 5, and 7, respectively (Table 3). With regard to the changes in the alignment of the implant, there was no case with more than 3° varus or valgus. The degree of subsidence of the femoral stem was 1, 2, and 3 mm in ten, six and five patients, respectively. No case of more than 5 mm subsidence or osteolysis was encountered. A superficial infection occurred as a postoperative complication in three patients (3.8%), which was treated with local wound care and antibiotics. Heterotopic ossification was noted in three patients (3.8%). Neither an intraoperative femoral fracture nor death during surgery occurred. No case of death during the hospital stay or other complications, such as joint dislocation, deep infection and embolism, were encountered.
Unstable intertrochanteric fractures in elderly patients with osteoporosis are characterized by severe comminution and displacement. Anatomic reduction of the fractures is difficult to achieve and maintain, often leading to malunion or reduction failure.2) In addition, postoperative early ambulation may not be feasible, and the rates of postoperative complications and mortality are high due to combined disorders. Accordingly, postoperative early ambulation and rehabilitation should be taken into account when considering treatment options, and hemiarthroplasty is regarded as one of the most effective primary treatment methods for unstable intertrochanteric fractures.3,4,17,18)
Cemented fixation is advantageous for achieving initial implant stability and rapid rehabilitation in cases of unstable fractures with poor bone quality.17,19,20) Cementless implants can be used to prevent cement-related problems, but implant migration due to bone ingrowth failure, thigh pain and bone resorption as a result of increased stiffness can be problematic.21,22) There are recent reports showing that implant migration can be avoided by promoting the osteointegration of cementless femoral components.21,23) In particular, the osteointegration rates are high even in elderly patients with osteoporosis and there has been no increase in the implant failure rates.7,22) In the current study, initial press-fit fixation was achieved in all patients either at the proximal canal or isthmus, and fixation by bone ingrowth or fibrous stable fixation were observed after a more than two year follow-up, even though 1 mm, 2 mm, and 3 mm subsidence were observed in 10, 6, and 5 patients at the 1st postoperative year. This indicates that the osteointegration rate in the diaphysis can be high in osteoporotic elderly patients with a Singh index less than grade 3 after the insertion of AML implants. Therefore, the use of cementless implants can lead to satisfactory results, even in elderly patients with osteoporosis. There were no postoperative complications, such as femoral stem loosening, significant alignment changes and progressive subsidence. Kang et al.11) reported that the loss of bone density in the proximal femur after arthroplasty using AML implants was not associated with the clinical symptoms, even though it occurred at a significant level in zone 7. In this study, bone resorption was observed primarily in the proximal area, such as zones 1, 2, and 7, but this did not lead to a fracture or loosening during the follow-up period.
Early ambulation within 2 to 3 weeks after surgery is important for preventing complications that can be caused by long-term bed rest in elderly patients with a poor general condition and combined diseases.24) The achievement of initial press-fit fixation is essential for early ambulation and rehabilitation. In one study, hemiarthroplasty produced better postoperative results than internal fixation in terms of limping and the use of a walking aid in patients with limited walking ability before surgery.18) Considering that press-fit fixation in the proximal femur is difficult to achieve in elderly patients with unstable fractures, the use of a cylindrical implant that can be fixed to the isthmus or diaphysis can be helpful. The AML implant is effective in improving the initial rotational stability owing to its broad triangular shape in the proximal portion. In addition, it can provide initial and late stability25) owing to the cylindrical shape in the middle, which is congruent with the shape of the femoral diaphysis making isthmic level or diaphyseal fixation possible regardless of the Dorr type.26) In this study, initial press-fit fixation was achieved in the isthmus in 12 patients (30%) in whom proximal fixation was not possible. The prevention of complications associated with long bed rest or those requiring intensive treatments, such as fat thrombosis or lung embolism, was attributed to the achievement of initial press-fit fixation, the initiation of quadriceps femoris muscle exercise and wheel chair ambulation immediately after surgery, and walking exercise at 1 week after surgery.
The functional outcomes after hemiarthroplasty tend to worsen over time due to the decrease in activity caused by the aggravation of preexisting diseases.4) In this study, the postoperative walking ability became worse compared to the preoperative one in 16 (40%) of the 40 patients. This was attributed to muscle weakness and a decrease in balancing ability during the postoperative period, which are common in elderly patients. The overall postoperative functional recovery was satisfactory, because all patients could walk with or without support except for two; one patient with worsening cerebrovascular disease and the other with a poor general condition. Similarly, twenty-three patients (57.5%) could carry out their daily activities without assistance, such as walking and washing. Ambulation became worse due to pain in 2 patients but there were no abnormal findings, such as implant loosening or ≥ 2 cm lower limb-length discrepancy.
Cemented fixation is associated with the highest death rate in arthroplasty patients,27) which can be a concern for elderly patients in whom combined diseases and poor general condition are common. A short-term follow-up study showed that bipolar hemiarthropasty using a tapered femoral stem for displaced femoral neck fractures in more than 70-years-old patients produced clinically and radiologically satisfactory outcomes.28) In this study, cementless fixation of cylindrical implants for the treatment of intertrochanteric fractures resulted in satisfactory results due to the avoidance of cement toxicity and the sufficient initial fixation strength provided by the press-fit fixation at either the proximal or isthmic levels. Accordingly, the patients could achieve early ambulation and rehabilitation, and the stability could be secured with endosteal new bone formation postoperatively.
The short-term results of cementless bipolar hemiarthroplasty in elderly patients with unstable intertrochanteric fractures demonstrated satisfactory results. These results are expected to be useful for further studies with a long-term follow-up.
Figures and Tables
Fig. 1
Anteroposterior radiographs of the right hip. (A) A 78-year-old woman had an unstable intertrochanteric fracture. (B) The postoperative radiograph shows a good proximal canal fit. (C) At postoperative 40 months, the radiograph shows the union of the lesser trochanter and stable fibrous fixation of the femoral component without subsidence or changes in alignment.

References
1. Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am. 2001. 83(5):643–650.

2. Kang SY, Lee EW, Kang KS, et al. Mode of fixation failures of dynamic hip screw with TSP in the treatment of unstable proximal femur fracture: biomechanical analysis and a report of 3 cases. J Korean Orthop Assoc. 2006. 41(1):176–180.

3. Hwang DS, Kwak SK, Woo SM. Results of cementless hemiarthroplasty for elderly patients with unstable intertrochanteric fractures. J Korean Hip Soc. 2004. 16(3):386–391.
4. Jahng JH, Sohn JM, Ha NK, Cho ST, Jeong JH. Primary bipolar hemiarthroplasty for treatment of unstable intertrochanteric fracture of the femur in elderly patients. J Korean Hip Soc. 2005. 17(2):76–82.
5. Rothman RH, Cohn JC. Cemented versus cementless total hip arthroplasty: a critical review. Clin Orthop Relat Res. 1990. (254):153–169.
6. Christie J, Burnett R, Potts HR, Pell AC. Echocardiography of transatrial embolism during cemented and uncemented hemiarthroplasty of the hip. J Bone Joint Surg Br. 1994. 76(3):409–412.

7. Kayali C, Agus H, Ozluk S, Sanli C. Treatment for unstable intertrochanteric fractures in elderly patients: internal fixation versus cone hemiarthroplasty. J Orthop Surg (Hong Kong). 2006. 14(3):240–244.

8. Singh M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am. 1970. 52(3):457–467.

9. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969. 51(4):737–755.

10. Kawamura H, Dunbar MJ, Murray P, Bourne RB, Rorabeck CH. The porous coated anatomic total hip replacement: a ten to fourteen-year follow-up study of a cementless total hip arthroplasty. J Bone Joint Surg Am. 2001. 83(9):1333–1338.
11. Kang JS, Moon KH, Park SR, Sun SH. Long-term results of total hip arthroplasty with an AML hip prosthesis. J Korean Hip Soc. 2004. 16(1):17–23.
12. Kim YH, Kim VE. Cementless porous-coated anatomic medullary locking total hip prostheses. J Arthroplasty. 1994. 9(3):243–252.

13. Engh CA, Bobyn JD, Glassman AH. Porous-coated hip replacement: the factors governing bone ingrowth, stress shielding, and clinical results. J Bone Joint Surg Br. 1987. 69(1):45–55.

14. Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990. (257):107–128.

15. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979. (141):17–27.
16. Kim YM, Kim HJ, Ahn JH, Kim KH, Kang SB. Early postoperative periprosthetic radiological findings in cementless THRA: comparison between porous-coated implant and hydroxyapatite-coated implant. J Korean Orthop Assoc. 1997. 32(4):1005–1014.

17. Stern MB, Angerman A. Comminuted intertrochanteric fractures treated with a Leinbach prosthesis. Clin Orthop Relat Res. 1987. (218):75–80.

18. Moon CY, Ji JH, Park SE, Kim YY, Lee SW, Kim WY. Comparison of the clinical outcomes between internal fixation and primary hemiarthroplasty for treating unstable intertrochanteric fracture in the elderly. J Korean Hip Soc. 2008. 20(4):273–277.

19. Green S, Moore T, Proano F. Bipolar prosthetic replacement for the management of unstable intertrochanteric hip fractures in the elderly. Clin Orthop Relat Res. 1987. (224):169–177.

20. Haentjens P, Casteleyn PP, De Boeck H, Handelberg F, Opdecam P. Treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients: primary bipolar arthroplasty compared with internal fixation. J Bone Joint Surg Am. 1989. 71(8):1214–1225.

21. Andress HJ, Kahl S, Kranz C, Gierer P, Schurmann M, Lob G. Clinical and finite element analysis of a modular femoral prosthesis consisting of a head and stem component in the treatment of pertrochanteric fractures. J Orthop Trauma. 2000. 14(8):546–553.

22. Maloney WJ. Femoral fixation in older patients: uncemented is reasonable in many patients. In : 74th Annual Meeting of the American Academy of Orthopaedic Surgeons; 2007 Feb 14-18; San diego, CA, USA.
23. Weber M, Hempfing A, Orler R, Ganz R. Femoral revision using the Wagner stem: results at 2-9 years. Int Orthop. 2002. 26(1):36–39.

24. Hinchey JJ, Day PL. Primary prosthetic replacement in fresh femoral-neck fractures: a review of 294 consecutive cases. J Bone Joint Surg Am. 1964. 46(2):223–240.
25. Engh CA, Hopper RH Jr. The odyssey of porous-coated fixation. J Arthroplasty. 2002. 17:4 Suppl 1. 102–107.

26. Dorr LD, Faugere MC, Mackel AM, Gruen TA, Bognar B, Malluche HH. Structural and cellular assessment of bone quality of proximal femur. Bone. 1993. 14(3):231–242.

27. Parvizi J, Holiday AD, Ereth MH, Lewallen DG. The Frank Stinchfield Award: sudden death during primary hip arthroplasty. Clin Orthop Relat Res. 1999. (369):39–48.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download