Abstract
Methods
Twelve patients (10 females and 2 males) who underwent revision surgery after vertebroplasty or kyphoplasty were included. In 4 cases, vertebroplasty was done for two or more levels. Six cases with kyphoplasty were included. Through the retrospective review of the radiographic studies and medical record, we analyzed the etiology of the revision surgery.
Results
Uncontrolled back pain was the main clinical presentation. In 4 cases, neurological symptoms were noted, including one case with conus medullaris syndrome. The average time to the revision surgery after vertebroplasty or kyphoplasty was 15 months. Infection (4 cases) and progressive kyphosis with collapse (8 cases) were the causes for the revision. A solid pattern of inserted bone cement and bone resorption around the cement were noted in the all cases with progressive collapse and kyphosis.
Percutaneous vertebroplasty (PVP) using bone cement was first introduced by Galibert et al.1) and this technique has been adopted as a treatment option for patients with painful osteoporotic compression fractures and destructive metastatic lesions of the vertebral bodies. Although it has many advantages, e.g., minimal invasive surgery, rapid relief of pain, early ambulation and restoration of the vertebral height (in the case of percutaneous kyphoplasty [PKP]), it has the potential risk of serious complications. Neurologic complications caused by leakage of injected bone cement, cardiopulmonary complications, infections and the new fractures of the adjacent vertebrae have all been reported.2-8) To the best of our knowledge, no report has been issued on the cause of late revision surgeries after PVP or PKP. The purpose of this study was to determine the causes of revision surgery after PVP or PKP and to evaluate the clinical results after the revisions.
This retrospective study was conducted on a consecutive series of 12 patients. All the patients were referred to the authors' hospital with complaints of uncontrolled pain with or without neurological manifestations between November 2001 and July 2006 (Table 1). The patients ranged in age from 23 to 79 years with a mean age of 67 years. Ten women and 2 men were included. The patients with the following criteria were excluded: 1) emergency decompression for neurological complications after PVP or PKP; 2) revision surgery related to subsequent fractures; and 3) the presence of metastatic lesions. Retrospective reviews of the radiographic and medical record were performed for all 12 patients to determine the causes of revision surgery. During the radiographic review, the accuracies of the initial diagnosis and identifying the problematic levels were evaluated and the distribution patterns of the polymethylmethacrylate cement were classified as trabecular or solid opacification according to the criteria of Lane et al.9) Progression of kyphosis was evaluated by measuring the changes in the kyphotic angle using Cobb's method. During the review of the clinical data, the laboratory findings were analyzed, including the erythrocyte sedimentation rate and the C-reactive protein level. The clinical results were evaluated using the Oswestry Disability Index (ODI) and the visual analogue scale.
Uncontrolled back pain and neurologic complications were the presenting symptoms resulting in revision surgery. Four patients, including one patient with conus medullaris syndrome, complained of progressive neurologic deficits. The average time to revision was 15 months (range, 3 to 70 months). Six of the twelve patients had undergone PKP. Osteoporotic compression fracture was the main diagnosis for performing the initial PVP and PKP, except in one case. In this case (case #11), the patient had undergone PKP for an unstable burst fracture at another institute. Initially, the patient had refused a major operation for religious reasons. The causes of the revision surgery were 1) infection for two patients with a postoperative infection and for two misdiagnosed patients and 2) a progressive kyphosis for four patients with neurological manifestations. In the two misdiagnosed patients, we were able to confirm the presence of a preoperative infection by retrospectively reviewing the clinical data, and this included elevated laboratory findings related to infection. Signal changes on the adjacent vertebral bodies on the initial MRI misled the surgeon to interpret the infection as a benign compression fracture and so PKP was performed as a result (Fig. 1). The causative organism was only identified in one case, in which it was confirmed to be tuberculosis with the appropriate histological findings. Intractable back pain and neurological manifestations were the causes of revision surgery in eight patients with progressive kyphosis. The mean increase in the kyphotic angle in these patients was 11 ± 12.1° (immediate postoperative, 4.8°; pre-revision, 15.1°). In seven of the eight patients, the pattern of inserted bone cement showed solid-patterned opacification as described by the Lane classification (Fig. 2) and osteolysis around the cement on the final radiographs was observed in all eight patients. Anterior and posterior fusion was performed in all cases, except for one who underwent posterior decompression only. During the anterior decompression and corpectomy, we found that the piecemeal removal of the cement had not been complicated and that the cement had been encircled by fibrous tissues. These findings coincided with a finding of peri-cement bone resorption. The histologic findings revealed fibrous tissue with evidence of chronic inflammation. However, neither necrosis nor bone remodeling was observed in the fibrous tissue (Fig. 3). The mean visual analogue scale (VAS) score at 1 month after revision surgery was 4.3 ± 1.1, which represented a considerable improvement compared to the preoperative score of 8.2 ± 0.6. The mean ODI score after operation was 52.9 ± 17.3, which was comparable to the preoperative score of 78 ± 9.8. The complications of revision surgery were one patient death due to postoperative sepsis and worsened metastatic lesion, and the other complication was a metallic failure and protrusion of the instrument, which led to removal of instrumentation at 1 year postoperatively.
Osteoporosis is an increasing medical and social problem in aging societies. According to one report, 30% of post menopausal women suffer from osteoporosis, and 40% of post menopausal woman experience an osteoporotic fracture.10) Moreover, if the fractures are not properly treated, and especially spinal fracture, then secondary medical problems will arise due to the limited ambulation. Thus, proper and timely management is critical. PVP and PKP were recently introduced, in conjunction with polymethylmethacrylate bone cement, to improve the pain, enhance the self-ambulation and reduce the risks of secondary medical problems. Despite their sound theoretical backgrounds, the simplicities of these procedures and the good clinical results obtained, PVP and PKP do present risks for critical complications. In particular, cement leakage to an adjacent disc or through the venous drainage system is frequently encountered, whilst the symptomatic neurological complications due to compression of a nerve root or the spinal cord are less frequent. Several reports have described emergency decompressions for neurological complications caused by cement leakage.6,11) Other acute complications such as pulmonary embolism, hematoma, anaphylactic reaction and death are rarely encountered.5,12) More specifically, the adjacent segment refractures are the focus of recent attention, but it remains debatable whether these adjacent segment refractures should be viewed as a complication of PVP.2,8,13)
One of the fatal complications is massive infection after PVP, but this is very rare and less than 15 such cases have been reported.4,11,14-16) Several studies have insisted that infection after PVP is probably related with a prior nonvertebral infection, an immunocompromised condition or intraoperative contamination. Thus, to prevent postoperative infections, cement mixed with antibiotics has been recommended in the cases with a previous infection, and especially for the cases with a genitourinary tract infection, or in immunocompromised patients.4,16) Alfonso Olmos et al.4) recommended screening and treatment for systemic infection before reoperation. In our cases with infection, antibiotic-impregnated cement was not used. Furthermore, unlike these reported cases, for two of the patients of the present study, a misdiagnosis was caused by infection and PVP was performed in the infected vertebrae in these patients. This scenario was confirmed by a review of the radiographic films and the clinical data. In these cases, the abnormal signal changes caused by infection were erroneously interpreted as osteoporotic compression fractures. So an accurate diagnosis, a careful review of the clinical and laboratory data and considering the use of antibiotic-impregnated cement in this special condition are important to prevent an infective condition following PVP or PKP. Postvertebroplasty infection has generally been treated with long-term antibiotics or by surgical intervention,4,11,14-16) and in the cases that are refractory to antibiotics, surgical debridement and stabilization have been performed.4,16) We also performed anterior corpectomy and stabilization for uncontrolled infections.
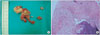
Progressive kyphosis after PVP or PKP can be developed by the subsequent fracture or the progressive collapse of the operated vertebra, as was noted in the present series. In terms of the subsequent fractures, the published reports vary considerably in terms of their incidence after PVP or PKP (range, 3 to 52%).2,8,17) Moreover, although no comparative study has been conducted to compare between vertebroplasty and conservatively treated fractures, the incidence of subsequent fracture after PVP or PKP is higher than the rate of the non-surgically treated fractures in many reports.8,13,17) However, Fribourg et al.2) concluded that the rate of subsequent fracture after 2 months postoperatively decline dramatically and then the rate become more similar to the rate of fracture of the general population. Alteration of the stiffness of an augmented vertebra and the load distribution in the adjacent vertebrae after PVP or PKP might increase the risk of the subsequent fracture, and several biomechanical studies have confirmed these findings.2,18,19) Progressive collapse of an augmented vertebral body could be another cause of progressive kyphosis and neurological complications after PVP or PKP. Our study revealed eight patients with progressive collapse of cement-injected vertebrae. Moreover, 7 of these 8 showed a solid-pattern of cement distribution and 5 of the 8 showed a preoperative intravertebral cleft. Although Belkoff et al.18) found no significant difference between PVP and PKP in terms of the posttreatment stiffness in a biomechanical cadaveric study (904 N/mm vs. 996 N/mm), we presume that the pattern of cement might influence the distribution of stress on the vertebrae. A trabecular-pattern of cement could reduce the stress concentration effects of the injected bone cement, whereas a solid-pattern of cement, which is a lack of interspersion along the trabecular space, will increase the stress concentration on the vertebrae. Oka et al.20) have reported that a solid-pattern of distribution of cement was related to the presence of an intravertebral cleft, and the solid-pattern distribution was often noted in a complicated condition such as pseudarthrosis. Other reports have concluded that the presence of an intravertebral cleft is a poor prognostic indicator after vertebroplasty.7,21) Consequently, the interaction of these findings might increase the risk of progressive collapse of augmented vertebrae. In terms of histologic findings around cement, Togawa et al.22,23) reported that there was good cancellous bone density around the cement after PKP without the extensive necrosis. And those authors insisted that the tamping had displaced bone and there was autografting in the space around the cement. However, in the present study, the thick fibrous tissue was found without extensive bone necrosis (Fig. 3), which differs from that observed by Togawa et al. The time of retrieval of cement fragments and the primary pathologic condition might be related to different histologic findings. Although we are uncertain whether it is a cause or a result, we think that peri-cement bone resorption portends progressive vertebral collapse after PVP or PKP.
The present study is intrinsically limited because it was based on a retrospective case analysis. Case-controlled studies with the long-term follow-up supported by the biomechanical findings after PVP or PKP are required to determine the significance of the cement patterns and peri-cement bone resorption. We conclude that misdiagnosis, postvertebroplasty infection and progressive collapse are the prime causes of radical revision surgery after PVP or PKP. More attention should probably be given to the cases with the presence of the preoperative intravertebral cleft sign, peri-cement bone resorption and a postoperative solid pattern of bone cement.
Figures and Tables
Fig. 1
Case no. 3. Serial MRI (April 21 and 22, 2006 and 2 weeks later) of the kyphoplasty that was done for L1 under the misdiagnosis of osteoporotic compression fracture. Destructive changes of an adjacent endplate and bone resorption around the bone cement were noted.

Fig. 2
Case no. 9. (A) Vertebroplasty of T12: note the solid and trabecular types of bone cement patterns, the peri-cement bone resorption and the local kyphosis. (B) On the CT and MR images, compression of the conus medullaris by progressive kyphosis and retropulsed bone were noted. The solid-type bone cement pattern, peri-cement bone resorption and a high signal around the cement were also noted. (C) Anterior decompression and fusion were performed.

Fig. 3
Gross and microscopic findings of the peri-cement tissue taken by anterior resection. The piecemeal retrieval of cement was not found to be a complicated procedure; the cement had been encircled by fibrous tissues. Thick amorphous fibrous tissue without extensive necrosis or bone remodeling was found (H&E, × 40).
References
1. Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987. 33(2):166–168.
2. Fribourg D, Tang C, Sra P, Delamarter R, Bae H. Incidence of subsequent vertebral fracture after kyphoplasty. Spine (Phila Pa 1976). 2004. 29(20):2270–2276.

3. Lin EP, Ekholm S, Hiwatashi A, Westesson PL. Vertebroplasty: cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004. 25(2):175–180.
4. Alfonso Olmos M, Silva Gonzalez A, Duart Clemente J, Villas Tome C. Infected vertebroplasty due to uncommon bacteria solved surgically: a rare and threatening life complication of a common procedure: report of a case and a review of the literature. Spine (Phila Pa 1976). 2006. 31(20):E770–E773.
5. Quesada N, Mutlu GM. Images in cardiovascular medicine: pulmonary embolization of acrylic cement during vertebroplasty. Circulation. 2006. 113(8):e295–e296.
6. Shin KS, Kim JS, Lee DW, Kim JS, Heo JK. Surgical treatment of root injury after percutaneous vertebroplasty: case report. J Korean Soc Spine Surg. 2002. 9(1):54–58.

7. Trout AT, Kallmes DF, Lane JI, Layton KF, Marx WF. Subsequent vertebral fractures after vertebroplasty: association with intraosseous clefts. AJNR Am J Neuroradiol. 2006. 27(7):1586–1591.
8. Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003. 226(1):119–124.

9. Lane JI, Maus TP, Wald JT, Thielen KR, Bobra S, Luetmer PH. Intravertebral clefts opacified during vertebroplasty: pathogenesis, technical implications, and prognostic significance. AJNR Am J Neuroradiol. 2002. 23(10):1642–1646.
10. Melton LJ 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective: how many women have osteoporosis? J Bone Miner Res. 1992. 7(9):1005–1010.

11. Deramond H, Depriester C, Galibert P, Le Gars D. Percutaneous vertebroplasty with polymethylmethacrylate: technique, indications, and results. Radiol Clin North Am. 1998. 36(3):533–546.
12. Won JH, Yeom JS, Park SK, Lee JH, Chang BS, Lee CK. Two simple tests for adequate needle positioning in vertebroplasty. J Korean Soc Spine Surg. 2006. 13(2):101–105.

13. Lindsay R, Silverman SL, Cooper C, et al. Risk of new vertebral fracture in the year following a fracture. JAMA. 2001. 285(3):320–323.

14. Schmid KE, Boszczyk BM, Bierschneider M, Zarfl A, Robert B, Jaksche H. Spondylitis following vertebroplasty: a case report. Eur Spine J. 2005. 14(9):895–899.

15. Vats HS, McKiernan FE. Infected vertebroplasty: case report and review of literature. Spine (Phila Pa 1976). 2006. 31(22):E859–E862.
16. Yu SW, Chen WJ, Lin WC, Chen YJ, Tu YK. Serious pyogenic spondylitis following vertebroplasty: a case report. Spine (Phila Pa 1976). 2004. 29(10):E209–E211.
17. Grados F, Depriester C, Cayrolle G, Hardy N, Deramond H, Fardellone P. Long-term observations of vertebral osteoporotic fractures treated by percutaneous vertebroplasty. Rheumatology (Oxford). 2000. 39(12):1410–1414.

18. Belkoff SM, Mathis JM, Fenton DC, Scribner RM, Reiley ME, Talmadge K. An ex vivo biomechanical evaluation of an inflatable bone tamp used in the treatment of compression fracture. Spine (Phila Pa 1976). 2001. 26(2):151–156.

19. Berlemann U, Ferguson SJ, Nolte LP, Heini PF. Adjacent vertebral failure after vertebroplasty: a biomechanical investigation. J Bone Joint Surg Br. 2002. 84(5):748–752.
20. Oka M, Matsusako M, Kobayashi N, Uemura A, Numaguchi Y. Intravertebral cleft sign on fat-suppressed contrast-enhanced MR: correlation with cement distribution pattern on percutaneous vertebroplasty. Acad Radiol. 2005. 12(8):992–999.
21. Ha KY, Lee JS, Kim KW, Chon JS. Percutaneous vertebroplasty for vertebral compression fractures with and without intravertebral clefts. J Bone Joint Surg Br. 2006. 88(5):629–633.

22. Togawa D, Bauer TW, Lieberman IH, Takikawa S. Histologic evaluation of human vertebral bodies after vertebral augmentation with polymethyl methacrylate. Spine (Phila Pa 1976). 2003. 28(14):1521–1527.

23. Togawa D, Kovacic JJ, Bauer TW, Reinhardt MK, Brodke DS, Lieberman IH. Radiographic and histologic findings of vertebral augmentation using polymethylmethacrylate in the primate spine: percutaneous vertebroplasty versus kyphoplasty. Spine (Phila Pa 1976). 2006. 31(1):E4–E10.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download