Abstract
Background
The clinical and radiological outcomes of revision total knee arthroplasty with a cemented posterior stabilized (PS), condylar constrained knee (CCK) or a fully constrained rotating hinge knee (RHK) prosthesis were evaluated.
Methods
This study reviewed the clinical and radiological results of 36 revision total knee arthroplasties with a cemented PS, CCK, and RHK prosthesis in 8, 25, and 13 cases, respectively, performed between 1998 and 2006. The mean follow-up period was 30 months (range, 24 to 100 months). The reason for the revision was aseptic loosening of one or both components in 15, an infected total knee in 18 and a periprosthetic fracture in 3 knees. The average age of the patients at the time of the revision was 65 years (range, 58 to 83 years). The original diagnosis for all primary total knee arthroplasties was osteoarthritis except for one case of a Charcot joint. All revision prostheses were fixed with cement. The bone deficiencies were grafted with a cancellous allograft in the contained defect and cortical allograft fixed with a plate and screws in the noncontained defect. A medial gastrocnemius flap was needed to cover the wound dehiscence in 6 of the 18 infected cases.
Results
The mean Knee Society knee score improved from 28 (range, 5 to 43) to 83 (range, 55 to 94), (p < 0.001) and the mean Knee Society function score improved from 42 (range, 10 to 66) to 82 (range, 60 to 95), (p < 0.001) at the final follow-up. Good or excellent outcomes were obtained in 82% of knees. There were 5 complications (an extensor mechanism rupture in 3 and recurrence of infection in 2 cases). Three cases of an extensor mechanism defect (two ruptures of ligamentum patellae and one patellectomy) were managed by the RHK prosthesis to provide locking stability in the heel strike and push off phases, and two cases of recurrent infection used an antibiotic impregnated cement spacer. The radiological tibiofemoral alignment improved from 1.7° varus to 3.0° valgus in average. Radiolucent lines were observed in 18% of the knees without progressive osteolysis.
Conclusions
Revision total knee requires a more constrained prosthesis than primary total knee arthroplasty because of the ligamentous instability and bony defect. This short to midterm follow-up analysis demonstrated that a well planned and precisely executed revision can reduce pain and improve the knee function significantly. Infected cases showed as good a result as those with aseptic loosening through the use of antibiotics-impregnated cement beads and proper soft tissue coverage with a medial gastrocnemius flap.
Primary total knee arthroplasty (TKA) has proven to be a highly successful operation over the past two decades with survivorship rates approaching 95% after a 15-year follow-up period.1) However, the results of revision TKA over the same period have been less encouraging. Failure rates in the range of 11% to 60% have been reported after a generally shorter follow-up interval.2-12) The poorer results of revision arthroplasty have been attributed to multiple factors including the loss of host bone stock quantity and quality,5,12,13) extensor mechanism problems,7,12) ligamentous instability or soft tissue incompetence,3,5,12) malalignment,3,12) revision for pain of an unclear etiology,8) progressive radiolucency7) and infection.4,5)
The approach to revision TKA is further complicated by the variability of available prostheses with respect to the degree of prosthesis constraint and the method of fixing the prosthesis to the bone. Similar results have been reported with condylar-type implants designed to preserve, or function in the absence of the posterior cruciate ligament9,14) and semiconstrained or posterior cruciate ligament-substituting condylar designs.6,7,11) There is also some controversy regarding the fixation methods with cementless fixation13,15,16) and cemented fixation5,7,9,11) each having advocates in a revision setting.
These problems, such as soft tissue instability and bone deficiency, have been managed using cemented posterior stabilized (PS), condylar constrained knee (CCK) or fully constrained rotating hinge knee (RHK) prosthesis and a cancellous allograft in a contained defect and a cortical allograft fixed with a plate and screws in a noncontained defects. This study evaluated the clinical and radiologic outcomes of revision total knee arthroplasty with cemented PS, CCK and RHK knee prostheses.
The clinical and radiological results of 36 revision TKAs performed between January 1998 and June 2006 were reviewed. These 36 revision total knees were available for review at a minimum 24-month and an average 30-month follow-up period (range, 24 to 100 months). The mean interval between the primary TKA and revision TKA was 6 years 2 months (range, 6 month to 14 years 8 months). The patient population consisted of 31 women and five men with an average age of 65 years (range, 58 to 83 years) at the time of the revision. The left knee was involved in 20 knees and the right in 16 knees. The original diagnosis for all primary total knee arthroplasties was osteoarthritis except for one case of a Charcot joint. Twenty five knees (69%) had undergone more than one arthroplasty procedure prior to the revision. The reason for revision was aseptic loosening of one or both components in 15 knees (42%), infected total knee in 18 (50%) and a periprosthetic fracture in three knees (8%) (Table 1). The cases of isolated line were excluded.
All revision prostheses were cemented PS, CCK or RHK prosthesis. Among the 36 knees, 8 (22%), 15 (42%), and 13 (36%) knees received a cemented PS prosthesis (LPS-flex, NexGen®, Zimmer, Warsaw, IN, USA), CCK prosthesis (LCCK, NexGen®) and RHK prosthesis (RHK, NexGen®), respectively. In five knees (14%) with a severe noncontained bone defect, a cortical allograft fixed with a plate and screws was performed to replace either the proximal tibia (2 knees) or distal femur (3 knees). Intramedullary stems were commonly used in the femur and tibia. The most commonly used stem length in 28 out of 36 (78%) femoral components and in all 36 (100%) tibial components was 100 mm in both the femur and tibia.
All procedures were performed in a vertical laminar airflow room with body exhaust suits worn by the operating team. Prophylactic antibiotics, second generation cephalosporin or vancomycin, were administered immediately before the skin incision. Cultures and tissue for frozen-section analysis were obtained. The knees were considered aseptic if preoperative gram stain analysis was negative and the intraoperative frozen sections showed less than five leukocytes per high-power field in five different sites. A longitudinal midline skin incision was used in most cases with care being taken to incorporate and not cross the previous skin incisions. Exposure was obtained by a median parapatellar arthrotomy in 16 knees (44%) or by a tibial tubercle osteotomy in 20 knees (56%).
The failed prostheses and cement were removed preserving as much normal bone as possible using various tools, such as a like gigli saw, power saw and microdrill. The knee joint was debrided of cement and granulation tissue. The bone defects were completely excavated or exposed, large segmental defects were filled with cortical allograft bone, and contained cavitary defects were filled with cancellous allograft bone. The large segmental allograft was generally secured to the host bone with plates and screws and served as structural support for the implant (Fig. 1). The cancellous allograft was covered with a thin layer of doughy acrylic cement after filling the contained cavitary defects so that no further cement could penetrate the graft. The condylar prosthesis was implanted after pulse lavage irrigation of the remaining cut bone surfaces and cement pressurization. In general, a cemented PS prosthesis was used if both collateral ligaments were felt to be competent, and a CCK or RHK prosthesis was used if one or both collateral ligaments were incompetent. RHK was used in the case of extensor mechanism failure (Fig. 2). All revision prostheses were fixed with cement. Routine closure was performed over the close-suction drain and a bulky compression dressing was applied. Six out of 18 infection cases showed wound dehiscence located over the tibia tubercle or patellar tendon. A medial gastrocnemius flap was used to cover the skin defect and a skin graft was placed over the exposed medial gastrocnemius muscle (Fig. 3).
After surgery, continuous gentle active and passive motion was begun at 48 hours and partial weight bearing with crutches was recommended for six weeks until full weight bearing was allowed. When a tibial tubercle was osteotomised, active extension exercise was delayed for six weeks and a straight-leg immobilizer was used during ambulation.
The clinical results were graded according to the Knee Society knee score (KSKS) and the Knee Society function score (KSFS). With this scale, a score of 80 to 100, 70 to 79, 60 to 69, and less than 60 was considered excellent, good, fair and poor, respectively. The patients were examined and the X-rays were checked before surgery; six weeks, three months, six months, and one year after surgery; and annually thereafter. The range of motion was included in the same protocol.
Preoperative radiographs, including anteroposterior (AP), lateral, skyline, and long-standing AP views, were evaluated for axial alignment. The radiographs were analyzed in regards to the alignment, occurrence of bone-cement radiolucency and bone-graft incorporation. The radiolucency at the bone-cement or bone-implant interfaces was determined by an examination of the AP and lateral radiographs of the knee joint. The results were recorded in millimeters by the zone of the prosthesis in both the coronal and sagittal planes for the femur and tibia and for the coronal plane for the patella using the method recommended by the Knee Society.17) Both cortical and cancellous bone-grafts were judged qualitatively to be incorporated into the surrounding host bone based on the presence of retrabeculation and a normal bone density. A multiple comparison test and independent sample t-test were perform to analyze the results using SPSS ver. 12 (SPSS Inc., Chicago, IL, USA).
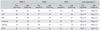
The average KSKS improved from 28 (range, 5 to 43) before the revision to 83 (range, 55 to 94), (p < 0.001), and the average KSFS improved from 42 (range, 10 to 66) to 82 (range, 60 to 95), (p < 0.001) at the final follow-up. Sixteen (44%) knees had an excellent result (80 to 100), 14 (38%) a good result (70 to 79), four (11%) a fair result (60 to 69), and two (5%) a poor result (less than 60). Overall, 30 knees (82%) had good or excellent results. The average range of motion improved from 81° (range, 0 to 125°) before the revision to 92° (range, 0 to 145°), (p < 0.05). There was no significant difference in the average KSKS between three different types of prosthesis; cemented PS (average score, 78; range, 55 to 94), CCK (average score, 81; range, 62 to 92), and RHK implant (average score, 83; range, 55 to 90) (p = 0.55) and in the average KSFS for cemented PS (average score, 79; range, 60 to 94), CCK (average score, 85; range, 64 to 92) and RHK implant (average score, 81; range, 65 to 95) (p = 0.61) (Table 2). In addition, there was no significant difference in the average KSKS between the aseptic loosening group (average score, 84; range, 57 to 94) and infected loosening group (average score, 81; range, 55 to 90) (p = 0.59) and in the average KSFS for the aseptic loosening group (average score, 83; range, 62 to 95) and infected total knee group(average score, 79; range, 60 to 92; p = 0.65) (Table 2).
The overall limb alignment improved from an average of 1.7° varus (range, 10° varus to 12° valgus) before surgery to 3.0° valgus at the final follow-up period (range, -4° varus to 10° valgus; p = 0.001) (Table 1). The radiolucency was relatively uncommon. Overall, seven knees (18%, two femur and five tibia components) had at least 1 mm radiolucency in one zone of one component. Three out of five (60%) radiolucent lines on the AP view of the tibia were localized to the medial tibial plateau. On the lateral view of the tibia, three out of four (75%) radiolucent lines were localized to the area below the anterior aspect of the tibial component. All radiolucent lines on the lateral view of the femur were localized to the anterior femoral condyle. No radiolucent line was observed in the patellar component, and none of the surviving knees showed evidence of either complete bone-cement radiolucency or progressive radiolucency.
Five knees with massive bone loss of the proximal tibia or distal femur were reconstructed with a bulk structural allograft into which the revision component had been cemented. None of these knees showed evidence of graft subsidence or bone-cement radiolucency. In all cases in which a cortical bone-graft had been used, the allograft appeared to be radiographically united to the host bone. All cancellous bone grafts used to fill the contained cavitary defects were also judged to be incorporated into host bone.
There were 5 cases with complications, extensor mechanism defects in 3 cases and a recurrence of infection in 2. The three cases with an extensor mechanism defect (two ruptures of the ligamentum patellae and one patellectomy) were managed using a RHK prosthesis to provide locking stability in the heel strike and push off phases. There were two cases of ligamentum patellae rupture. The first case was ruptured at local clinics by multiple operations due to the infected total knee and was managed by RHK prosthesis. The other was ruptured by trauma 3 months after the revision with a RHK prosthesis due to ligament instability and was managed with a patellar tendon reconstruction and a medial gastrocnemius flap.
The absolute number of revision total knee procedures will undoubtedly increase with the advancing age of the population and the increasing number of primary TKAs being performed.16,18) The high failure rates of revision TKA (up to 60%) prompted a review of our intermediate-term experience with revision TKA using a uniform approach of a cemented PS, CCK, and RHK prosthesis and cancellous or cortical allobone graft for bone defects.2,5)
The 82% good and excellent results in this study compare favorably with those previously reported for total knee revision, 40% to 89% success.2-12) Although most reports of revision TKA include multiple types of prostheses, several studies focused on posterior-stabilized or constrained condylar designs.5,7,11,19) Even within this group, the level of enthusiasm varied. Insall and Dethmers7) reported good and excellent results in 89% of their 72 revision TKAs at a minimum 2 year follow-up period, whereas Goldberg et al.5) reported good and excellent results in only 46% of 59 revision procedures performed for mechanical failure and followed up for an average of five years.
The results of revision TKA are expected to improve as reconstructive surgeons gain more experience with revision TKA and modern instrumentation systems facilitate proper anatomic placement of revision prostheses.5,7,11,19) Indeed in this study, despite the high percentage of patients with significant bone loss, the average anatomic axis improved to 3.0° valgus.
There is some controversy regarding the need to provide added collateral ligament constraint, such as the use of a constrained condylar prosthesis, or simply to maximize collateral ligament tension with an unconstrained implant in the revision setting. The fact that residual soft tissue instability (with a prosthesis that does not augment collateral ligament stability) can be a factor leading to the need to remove a prosthesis suggests that vigorous preoperative and intraoperative consideration should be given to collateral ligament integrity.
Previous authors emphasized the high rate of complications related to the extensor mechanism in revision TKA.5,8,20,21) For example, Stuart et al.,21) in a retrospective review of 655 condylar revision TKAs, found that an extensor mechanism problem was responsible for 41% of 60 knees requiring a reoperation. This highlights the need for meticulous attention to patellar tracking and preservation of the quadriceps and patellar tendon insertions during revision TKA. Three significant complications associated with extensor mechanism defects in this study, were related to the ruptures of the ligamentum patellae and patellectomy. In knees requiring an interruption of the extensor mechanism for enhanced exposure of the knee, our preference has been to perform a long laterally based tibial tubercle osteotomy. In this study, there were no adverse sequelae in the 20 knees (56%) in which the tibial tubercle osteotomy was performed.
Five knees with massive bone loss of the distal femur or proximal tibia required a reconstruction with a cortical bone graft. In all cases, the graft-host junction required internal fixation and the allograft had healed to the host bone. The clinical results (1 excellent, 3 good and 1 fair) and radiographic results (no bone-cement radiolucency) of these knees were similar to those of the total population. Similarly, the finding of apparent cancellous bone graft incorporation in contained cavitary defects is consistent with the data reported by other authors and further supports the use of an allogeneic bonegraft to augment the host bone stock.13,16,22,23)
The 18% prevalence of radiolucent lines in this group of cemented revisions is in the lower range of the 17 to 84% previously reported for knees with condylar-type designs.5,9,11,12,19) Most of the radiolucent lines in this study were limited to one zone and all were 1 mm wide or less. The complete absence of progressive radiolucency may be a reflection of the improved surgical technique or, more likely, the difficulty in visualizing lucent lines without fluoroscopically guided radiographs.
Jones23) reported that the primary indications for a modular rotating hinged knee include medial or lateral collateral loss, massive bone loss, and metaphysis and cortical shell, which includes collateral origins or insertion, as well as a severe flexion gap imbalance requiring a link system for stability. The indications for a hinge in primary TKA include patients with neuromuscular deficits, such as polio or flail knee, who require hyperextension stop.24) Morgan et al.24) reported rotating-hinge knee implants usually are recommended for patients with a severe deformity or instability that cannot be managed with a varus-valgus implant. Our indication of RHK use includes patients with ligamentous instability or soft tissue incompetence, severe bone defect and flexion gap imbalance. The constraint is defined as the effect of the elements of knee implant design that provides the stability required to counteract forces about the knee after arthroplasty in the presence of a deficient soft-tissue envelope.25) Increasing component constraint might reduce the instability. However, doing so may increase the forces transmitted to the fixation and implant interfaces, which might lead to premature aseptic loosening. On the other hand, Utting and Newman25) reported at a mid- and long-term review that no hinge revision knee replacements had failed from an aseptic cause and most of the knees of this challenging group were provided with stability and flexion. In our RHK cases, there was no choice but to use a more constraint prosthesis because of a severe bone defect, soft tissue deficiency and flexion gap imbalance, extensor mechanism problem by multiple operation and infection. Determining the amount of constraint necessary is a challenge requiring long-term research.
Revision total knee required more constrained prosthesis than primary total knee arthroplasty because of a ligamentous instability and bony defect. This short to midterm follow-up analysis demonstrates that a well planned and precisely executed revision can reduce pain and improve the knee function significantly. The infected cases showed as good a result as those with aseptic loosening through the use of antibiotics-impregnated cement beads and proper soft tissue coverage with a medial gastrocnemius flap.
Figures and Tables
Fig. 1
The large segmental allograft was generally secured to the host bone with plates and screws, and served as structural support for the implant. (A) Preoperative radiograph showing loosening of both components and liner wear. (B) Severe bone deficiency in the distal femur and tibia. (C) Large segmental defects were filled with cortical allograft bone and fixed with plates and screws.

Fig. 2
A cemented posterior stabilized prosthesis was used if both collateral ligaments were felt to be competent and a condylar constrained knee or rotating hinge knee prosthesis was used if more than one of collateral ligaments were incompetent or in the case of extensor mechanism failure. The radiograph shows the revision performed by cemented posterior stabilized (A), condylar constrained knee (B) and fully constrained rotating hinge knee prosthesis (C).

Fig. 3
Medial gastrocnemius flap was performed to cover the wound dehiscence of the infected cases. (A) Wound dehiscence after revision total knee arthroplasty. (B) Preparing medial gastrocnemius by posteromedial approach. (C) Wound coverage by a medial gastrocnemius flap. (D) Five months after a skin graft was placed over the exposed medial gastrocnemius muscle.

References
1. Ranawat CS, Flynn WF Jr, Deshmukh RG. Impact of modern technique on long-term results of total condylar knee arthroplasty. Clin Orthop Relat Res. 1994. (309):131–135.
2. Ahlberg A, Lunden A. Secondary operations after knee joint replacement. Clin Orthop Relat Res. 1981. (156):170–174.

3. Rand JA, Bryan RS. Revision after total knee arthroplasty. Orthop Clin North Am. 1982. 13(1):201–212.

4. Cameron HU, Hunter GA. Failure in total knee arthroplasty: mechanisms, revisions, and results. Clin Orthop Relat Res. 1982. (170):141–146.
5. Goldberg VM, Figgie MP, Figgie HE 3rd, Sobel M. The results of revision total knee arthroplasty. Clin Orthop Relat Res. 1988. (226):86–92.

6. Hanssen AD, Rand JA. A comparison of primary and revision total knee arthroplasty using the kinematic stabilizer prosthesis. J Bone Joint Surg Am. 1988. 70(4):491–499.

7. Insall JN, Dethmers DA. Revision of total knee arthroplasty. Clin Orthop Relat Res. 1982. (170):123–130.

8. Jacobs MA, Hungerford DS, Krackow KA, Lennox DW. Revision total knee arthroplasty for aseptic failure. Clin Orthop Relat Res. 1988. (226):78–85.

9. Rand JA, Bryan RS. Results of revision total knee arthroplasties using condylar prostheses: a review of fifty knees. J Bone Joint Surg Am. 1988. 70(5):738–745.

10. Ritter MA, Eizember LE, Fechtman RW, Keating EM, Faris PM. Revision total knee arthroplasty: a survival analysis. J Arthroplasty. 1991. 6(4):351–356.
11. Rosenberg AG, Verner JJ, Galante JO. Clinical results of total knee revision using the total condylar III prosthesis. Clin Orthop Relat Res. 1991. (273):83–90.

12. Thornhill TS, Dalziel RW, Sledge CB. Alternatives to arthrodesis for the failed total knee arthroplasty. Clin Orthop Relat Res. 1982. (170):131–140.

13. Samuelson KM. Bone grafting and noncemented revision arthroplasty of the knee. Clin Orthop Relat Res. 1988. (226):93–101.

15. Bertin KC, Freeman MA, Samuelson KM, Ratcliffe SS, Todd RC. Stemmed revision arthroplasty for aseptic loosening of total knee replacement. J Bone Joint Surg Br. 1985. 67(2):242–248.

16. Whiteside LA. Cementless revision total knee arthroplasty. Clin Orthop Relat Res. 1993. (286):160–167.

17. Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989. (248):9–12.

18. Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement: a meta-analysis. JAMA. 1994. 271(17):1349–1357.

19. Donaldson WF 3rd, Sculco TP, Insall JN, Ranawat CS. Total condylar III knee prosthesis: long-term follow-up study. Clin Orthop Relat Res. 1988. (226):21–28.
20. Engh CA, McGovern TF, Bobyn JD, Harris WH. A quantitative evaluation of periprosthetic bone-remodeling after cementless total hip arthroplasty. J Bone Joint Surg Am. 1992. 74(7):1009–1020.

21. Stuart MJ, Larson JE, Morrey BF. Reoperation after condylar revision total knee arthroplasty. Clin Orthop Relat Res. 1993. (286):168–173.

22. Wilde AH, Schickendantz MS, Stulberg BN, Go RT. The incorporation of tibial allografts in total knee arthroplasty. J Bone Joint Surg Am. 1990. 72(6):815–824.

23. Jones RE. Total knee arthroplasty with modular rotating-platform hinge. Orthopedics. 2006. 29:9 Suppl. S80–S82.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download