Abstract
Purpose
There are numerous reports about the usefulness of antibiotics such as doxycycline or metronidazole in the conventional treatment for the patients with chronic periodontal diseases. However, seldom are the reports about effects of vitamins or nutraceuticals. The purpose of this study was to evaluate the effects of nutrient supplement including multiple vitamins and neutraceuticals with PRF-K2 from plants and seaweed in treatment of the patients with chronic periodontitis which is needed a nonsurgical or a surgical treatment by evaluating the clinical parameters and the gingival crevicular fluid volume.
Methods
The systemically healthy and nonsmoking patients diagnosed with chronic periodontitis were divided into a nonsurgical group and a surgical group. They were also divided into the test group with nutrient supplements and the control group without nutrient supplements. In the nonsurgical group, the clinical parameters (probing depth, clinical attachment level, sulcus bleeding index, and plaque index) and the gingival crevicular fluid volume were checked on baseline, at 1 week, at 3 week and at 9 week after a supplement treatment. In the surgical group, the clinical parameters and the gingival crevicular fluid volume were also checked at 15 week after a surgical treatment.
Results
In both nonsurgical and surgical groups, reduction of pocket depth and increment of clinical attachment level were revealed in the test group compared with the control group, but there was not statistically significant difference (p>0.05), and sulcus bleeding index was decreased with statistically significant difference (p<0.05). In addition, plaque index was decreased with statistically significant difference (p<0.05) in the nonsurgical group. Gingival crevicular fluid volume was decreased with statistically significant difference (p<0.05) at week 9 in both non-surgical and surgical groups.
Figures and Tables
 | Figure 1Study design of non-surgical group (GCF, gingival crevicular fluid; PD, pocket depth; CAL, clinical attachment level; SBI, sulcus bleeding index; PI, plaque index; OHI, oral hygiene instruction). |
 | Figure 2Study design of surgical group (GCF, gingival crevicular fluid; PD, pocket depth; CAL, clinical attachment level; SBI, sulcus bleeding index; PI, plaque index; OHI, oral hygiene instruction; FO. flap operation). |
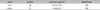
Table 5
Clinical Parameters for Anterior and Posterior Segments in Test Group of Non-surgical Group (Mean±SD)

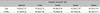
Table 8
Clinical Parameters for Anterior and Posterior Segments in Test Group of Surgical Group (Mean±SD)

References
1. Amaliya , Timmerman MF, Abbas F, et al. Java project on periodontal diseases: the relationship between vitamin C and the severity of periodontitis. J Clin Periodontol. 2007. 34:299–304.

2. Alfano MC. Controversies, perspectives, and clinical implications of nutrition in periodontal disease. Dent Clin North Am. 1976. 20:519–548.
3. Pedrazzoli V, Kilian M, Karring T, Kirkegaard E. Effect of surgical and non-surgical periodontal treatment on periodontal status and subgingival microbiota. J Clin Periodontol. 1991. 18:598–604.

4. Becker W, Becker BE, Ochsenbein C, et al. A longitudinal study comparing scaling, osseous surgery and modified Widman procedures. Results after one year. J Periodontol. 1988. 59:351–365.

5. Emingil G, Atilla G, Sorsa T, et al. The effect of adjunctive low-dose doxycycline therapy on clinical parameters and gingival crevicular fluid matrix metalloproteinase-8 levels in chronic periodontitis. J Periodontol. 2004. 75:106–115.

6. Akincibay H, Orsal SO, Sengün D, Tözüm TF. Systemic administration of doxycycline versus metronidazole plus amoxicillin in the treatment of localized aggressive periodontitis: a clinical and microbiologic study. Quintessence Int. 2008. 39:33–39.
7. Woolfe SN, Hume WR, Kenney EB. Ascorbic acid and periodontal disease: a review of the literature. J West Soc Periodontol Periodontal Abstr. 1980. 28:44–56.
8. Melnick SL, Alvarez JO, Navia JM, Cogen RB, Roseman JM. A case-control study of plasma ascorbate and acute necrotizing ulcerative gingivitis. J Dent Res. 1988. 67:855–860.

9. Neiva RF, Al-Shammari K, Nociti FH Jr, Soehren S, Wang HL. Effects of vitamin-B complex supplementation on periodontal wound healing. J Periodontol. 2005. 76:1084–1091.

10. Muroyama K, Murosaki S, Yamamoto Y, Ishijima A, Toh Y. Effects of intake of a mixture of thiamin, arginine, caffeine, and citric acid on adiposity in healthy subjects with high percent body fat. Biosci Biotechnol Biochem. 2003. 67:2325–2333.

11. Kozik A, Korytowski W, Sarna T, Bloom AS. Interactions of flavins with melanin. Studies on equilibrium binding of riboflavin to dopa-melanin and some spectroscopic characteristics of flavin-melanin complex. Biophys Chem. 1990. 38:39–48.
12. Morrow LE, Grimsley EW. Long-term diuretic therapy in hypertensive patients: effects on serum homocysteine, vitamin B6, vitamin B12, and red blood cell folate concentrations. South Med J. 1999. 92:866–870.

13. Aprahamian M, Dentinger A, Stock-Damgé C, Kouassi JC, Grenier JF. Effects of supplemental pantothenic acid on wound healing: experimental study in rabbit. Am J Clin Nutr. 1985. 41:578–589.

14. Berg RA, Steinmann B, Rennard SI, Crystal RG. Ascorbate deficiency results in decreased collagen production: under-hydroxylation of proline leads to increased intracellular degradation. Arch Biochem Biophys. 1983. 226:681–686.

15. Alvares O, Siegel I. Permeability of gingival sulcular epithelium in the development of scorbutic gingivitis. J Oral Pathol. 1981. 10:40–48.

16. Washko P, Rotrosen D, Levine M. Ascorbic acid in human neutrophils. Am J Clin Nutr. 1991. 54:1221–1227.

17. Glickman I. Acute vitamin C deficiency and the periodontal tissues; the effect of acute vitamin C deficiency upon the response of the periodontal tissues of the guinea pig to artificially induced inflammation. J Dent Res. 1948. 27:201–210.

18. Russell AL, Leatherwood EC, Consolazio CF, Vanreen R. Periodontal disease and nutrition in South Vietnam. J Dent Res. 1965. 44:775–782.

19. Nishida M, Grossi SG, Dunford RG, et al. Dietary vitamin C and the risk for periodontal disease. J Periodontol. 2000. 71:1215–1223.

20. Amarasena N, Ogawa H, Yoshihara A, Hanada N, Miyazaki H. Serum vitamin C-periodontal relationship in community-dwelling elderly Japanese. J Clin Periodontol. 2005. 32:93–97.

21. Muñoz CA, Kiger RD, Stephens JA, Kim J, Wilson AC. Effects of a nutritional supplement on periodontal status. Compend Contin Educ Dent. 2001. 22:425–428.
22. Kim YK, Chung HJ, Kim SW, Baek DH. The effect of neutraceutical containing PRF-K2 on periodontal condition during maintenance phase. J. Korean Aca Periodontol. 2007. 37:91–102.

23. Muhlemann HR, Son S. Gingival sulcus bleeding-a leading symptom in initial gingivitis. Helv Odontol Acta. 1971. 15:107–113.
24. Silness J, Loe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964. 22:121–135.

25. Vaxman F, Olender S, Lambert A, et al. Effect of pantothenic acid and ascorbic acid supplementation on human skin wound healing process. A double-blind, prospective and randomized trial. Eur Surg Res. 1995. 27:158–166.

26. Alvarez OM, Gilbreath RL. Thiamine influence on collagen during the granulation of skin wounds. J Surg Res. 1982. 32:24–31.

27. Halliwell B. Reactive oxygen species in living systems: source, biochemistry, and role in human disease. Am J Med. 1991. 91:14–22.

28. McGowan SE, Parenti CM, Hoidal JR, Niewoehner DE. Ascorbic acid content and accumulation by alveolar macrophages from cigarette smokers and nonsmokers. J Lab Clin Med. 1984. 104:127–134.
29. Kimura S, Yonemura T, Kaya H. Increased oxidative product formation by peripheral blood polymorphonuclear leukocytes in human periodontal diseases. J Periodontal Res. 1993. 28:197–203.

30. Parfitt GJ, Hand CD. Reduced plasma ascorbic acid levels and gingival health. J Periodontol. 1963. 34:47–51.

31. Vogel RI, Lamster IB, Wechsler SA, et al. The effects of megadoses of ascorbic acid on PMN chemotaxis and experimental gingivitis. J Periodontol. 1986. 57:472–479.

32. Leggott PJ, Robertson PB, Rothman DL, Murray PA, Jacob RA. The effect of controlled ascorbic acid depletion and supplementation on periodontal health. J Periodontol. 1986. 57:480–485.

33. Staudte H, Sigusch BW, Glockmann E. Grapefruit consumption improves vitamin C status in periodontitis patients. Br Dent J. 2005. 199:213–217.

34. Pihlstrom BL, McHugh RB, Oliphant TH, Ortiz-Campos C. Comparison of surgical and nonsurgical treatment of periodontal disease. A review of current studies and additional results after 61/2 years. J Clin Periodontol. 1983. 10:524–541.

35. Lamster IB. Evaluation of components of gingival crevicular fluid as diagnostic tests. Ann Periodontol. 1997. 2:123–137.

36. Loe H, Holm-Pedersen P. Absence and presence of fluid from normal and inflamed gingivae. Periodontics. 1965. 149:171–177.
37. Griffiths GS. Formation, collection and significance of gingival crevice fluid. Periodontol 2000. 2003. 31:32–42.

38. Minn WK, Lee MS. Effects of ascorbic acid and unsaponifiable fractions of Zea Mays L. on the experimentally induced periodontitis in rats. J. Korean Aca Periodontol. 1988. 18:6–23.
39. Kwon YH, Lee MS, Yang SH, Kim Y, Park JB. A clinical study of the effects on the healing process of administration of the Zea Mays L. after periodontal surgery. J Korean Aca Periodontol. 1994. 24:649–660.




 PDF
PDF ePub
ePub Citation
Citation Print
Print








 XML Download
XML Download