Abstract
Liver transplantation has improved the survival of patients with end stage liver disease. As the rates of success of liver transplantation continue to increase, more patients who have a liver transplant will become candidates for joint replacement due to osteonecrosis. The incidence of osteonecrosis has been variously reported as from 2% to 8.2% after liver transplantation. However, there are only three reports in the English medical literature about total hip arthroplasty for osteonecrosis of the femoral head following liver transplantation, and especially there has not been such a report from Asian countries. We report here on two patients with transplanted livers and who then underwent total hip arthroplasty.
Liver transplantation has improved the survival of patients with end stage liver disease. This improvement is mainly due to the advancement in patient selection, preoperative and postoperative care, surgical technique and immunosuppressive drugs1). Cyclosporine A is a potent inhibitor of cytotoic T-cells, and its use has increased the success of organ transplantation. Despite these advances, prednisone is still an important agent and osteonecrosis is a serious complication in this group of patients. The incidence of osteonecrosis was variously reported, from 2% to 8.2% after liver transplantation. One long-term study found no liver recipients developing osteonecrosis. Another study revealed a 1% incidence of osteonecrosis in a liver transplant population2). As the rates of success of organ transplantation continue to increase, more patients who have a liver transplant will become candidates for joint replacement due to osteonecrosis. However, there are only two reports in English literature about total hip arthroplasty (THA) for osteonecrosis of the femoral head following liver transplantation, and especially, there has not been such a report in Asian countries3,4). The authors report two patients with liver transplantation, who underwent total hip arthroplasty. The patients were informed that the data from the cases would be submitted for publication, and gave them consent.
A 55-year-old man visited our institution with severe pain in right hip. Twenty-two months before, the patient had undergone liver transplantation in another institution, because of liver cirrhosis secondary to hepatitis B. He is been administrated 2.5 mg of tacrolimus and 3,000 mg of mycophenolate mofetil (MMF) per day as immunosuppressive agents and injection Hepatitis B immunoglobulin of 10,000 international unit per month because his serum Anti-HBs antibody level was below 1,000 IU/L during the clinic visit. There was no graft rejection history until last review. Tacrolimus is an immunosuppressive drug that is mainly used after allogeneic organ transplant to reduce the activity of the patient's immune system and so lower the risk of organ rejection. It reduces interleukin-2 (IL-2) production by T-cells. MMF is a immunosuppresant and prodrug of mycophenolic acid, used extensively in transplant medicine. MMF is selective for the de novo pathway critical to lymphocytic proliferation and activation.
He showed limping gait and complained right hip pain which was aggravated during walking. And the symptoms had begun about 2 years after liver transplantation. Plain X-ray showed subchondral sclerosis of right femoral head with mild collpase. MRI showed the double line sign on right femoral head at T2 weighted coronal view and the hyperintense signal change of right femoral head at T2 weighted axial view. And left femoral head also showed signal change at T2 weighted coronal and axial view (Fig. 1).
Total hip arthroplasty using modified minimally invasive two incision was performed on right hip. 54 mm Delta PF® (Lima LTO, Vilanova San Daniele del Friuli (Udine), Italy) was used for acetabular cup and size 10 M/L Taper® (Zimmer, Inc. West Center street Warsaw, U.S.A.) for cementless femoral stem. We used cefazoline as prophylactic antibiotics before skin incision, and used antibiotics 3 times a day for 7 days, and patient use elastic stocking for 1 month to prevent venous thromboembolism and had no symptom such as calf pain or dyspnea after surgery. In preoperative liver function test, AST and ALT was slightly higher than normal range but platelet count was within normal range and there was no significant changes after surgery. He started partial weight bearing ambulation with walker on first day after surgery. Day 8 postoperatively Hepatitis B immunoglobulin of 10,000 unit injection was administered, and he started crutch ambulation on postoperative day 9. Day 10 postoperatively, he was discharged without any particular complications.
On last follow up (postoperative day of 35 months), he could walk normally and has no difficulty on his daily life. Harris Hip Score improved from 43 points before surgery to 98 points on last follow up (Fig. 2).
A 65-year-old man visited our hospital with left hip pain. Six years before, the patient had undergone liver transplantation in another institution, because of liver cirrhosis and hepatocellular carcinoma secondary to hepatitis B. He is been administrated lamivudine 100 mg and adefovir 10 mg per day instead of injection Hepatitis B immunoglobulin, and predinisolone 15 mg per day as immunosuppressive agents. There was no graft rejection history.
Lamivudine has been used for treatment of chronic hepatitis B at a lower dose than for treatment of HIV. It improves the seroconversion of e-antigen positive hepatitis B and also improves histology staging of the liver. Adefovir works by blocking reverse transcriptase, an enzyme that is crucial for the hepatitis B virus (HBV) to reproduce in the body. It is approved for the treatment of chronic hepatitis B in adults with evidence of active viral replication and either evidence of persistent elevations in serum aminotransferases (primarily ALT) or histologically active disease.
He complained limping gait and it tends to get aggravated with walking. And the symptoms had begun about 5 years after liver transplantation. He was diagnosed that osteonecrosis of both femoral head on preoperative radiographs and MRIs (Fig. 3).
Total hip arthroplasty using modified minimally invasive two incision was performed on left hip. 52 mm Delta PF® (Lima, Vilanova San Daniele del Friuli (Udine), Italy) and size 10 M/L Taper® (Zimmer, Inc. West Center street Warsaw, U.S.A.) was used. The dose of antibiotics and method to prevent venous thromboembolism were same as the first case. Preoperative liver function test and platelet count was within normal range and there was no significant changes after surgery. The rehabilitation program was same as the first case. He started on partial weight bearing ambulation with walker on first day after surgery. And he started to administrate lamivudine 100 mg and adefovir 10 mg, and tacrolimus 1.5 mg per day as same dose as before surgery. Day 9 postoperatively he started crutch ambulation and day 10 postoperatively he was discharged without any particular complications.
On last follow up in our out patients department (postoperative day of 12 months) he could walk normally, and has no difficulty on his daily life. Harris Hip Score improved from 68 points before surgery to 90 points on last follow up (Fig. 4).
Annually more than 5,000 liver transplantations are performed in the United States. The overall long-term survival has apparently improved despite coexisting morbidities, old age and high BMI of the operated patients, higher degree of HLA mismatch and long waiting time5). In Korea, 2,345 orthotopic liver transplantations were performed in 24 institutes form March 1988 to December 2004. One year survival after liver transplantation, deceased donor liver transplantation was 62%, and living donor was 80% in 1998, but the survival has improved to 76% in deceased donor liver transplantation and 83% in living donor liver transplantation6). In the literature review, we find that there are a few studies which reported on the prevalence of osteonecrosis of the femoral head and results of total hip arthroplasty following liver transplantation (Table 1). Papagelopoulos et al.7) reported that 23 (8.1%) of 285 liver transplant recipients developed symptomatic osteonecrosis of the femoral head following liver transplantation, and only 5 patients required total hip arthroplasty. There were no serious complication of THA. Taillandier et al.1) reported a 1 case of THA which was done for osteonecrosis of the femoral head. Levitsky et al.8) reported 3 cases of THA following liver transplantation, and there were no complication. Lieberman et al.9) reported that 4 (2%) of 203 patients were diagnosed with osteonecrosis of the hip after that surgery and there was no patients who required total hip arthroplasty, and these authors noted that this condition was rare and would not require MRI screening. Tannenbacum et al.3) reported that 4 cases of total hip arthroplasty for degenerative osteoarthritis of the hip joint following liver transplantation and 1 case of them required revision arthroplasty because of aseptic loosening.
Aseptic necrosis of the femoral head is also disabling complication of renal transplantation. Although its incidence has markedly decreased during the last decades as a result of the lowered steroid dosage secondary to the introduction of cyclosporine in immunosuppressive regimens, it still occurs in 4.5% of renal transplantation recipients10).
Management of osteonecrosis of the femoral head following solid organ transplantation procedures is based on the stage of the disease. Treatment regimens for osteonecrosis of the femoral head include nonsurgical management, arthrodesis, bone grafting and muscle pedicled bone graft, rotational osteotomy and total hip arthroplasty. As the success rate of solid organ transplantation continues to rise, more patients will be expected to become a candidate to joint replacement surgery. However, concerns still exist regarding the vulnerability of these patients to certain complications such as postoperative infection due to chronic immunosuppression and mechanical implant failure due to poor bone quality.
The immunosuppressive medication should be given at the scheduled times and no dose should be withheld. In a case of sepsis, a decrease in the immunosuppressive regimen is recommended. In patients who are stable after surgery, daily levels of cyclosporine and tacrolimus and liver function tests are unnecessary. It is sufficient to control the immunosuppressive medication level after surgery and to repeat in patients with variation greater than 25% of the baseline.
Corticosteroids are considered as first line armamentarium in the post-transplant immunosuppression. The introduction of azathioprin, which is a purin synthesis inhibitor, and cyclosporin A, which is a potent cytotoxic T-cells inhibitor, in early 1980s minimized the need for high corticosteroid doses and improved the overall graft survival and reducing the rejection rate. Further advancement was achieved by the discovery and the use of agents such as Tacrolimus which inhibits T-lymphocyte signal transduction and interleukin-2 transcription, and Sirolimus which inhibits the response to interleukin-2 thereby blocking the activation of T- and B-cells. In our cases, first case patent has been administrated 2.5 mg of tacrolimus and 3,000 mg of mycophenolate mofetil per day as immunosuppressive agents and second case patient has been administrated 15 mg of prednisolone per day as immunosuppressive agents.
Hamburg et al.4) reports that the bone mass decreases following liver transplantation, especially in the first 3 months, and with an accompanying high fracture rate in the first 6 months. This accelerated bone loss occurring in the early period after transplantation depends on several factors : initial high-dose steroid therapy, malnutrition, immobilization, and cyclosporine therapy. However, vertebral bone marrow density is gradually restored to normal within 2 or 3 years after liver transplantation, resulting in normalization of hepatic function. The transplanted liver can be taken to be the most important factor in the improvement of bone marrow density, a general catabolic state having been replaced by an anabolic state by successful liver transplantation.
These patients have traditionally been approached with great hesitancy because of their compromised immune status and poor bone stock secondary to the use of prednisone. However, total joint arthroplasty of the hip to date has been safe and effective in the management of symptomatic osteonecrosis in liver transplant recipients5). Despites the theoretical risks of high infection rates and inferior bone quality associated with joint arthroplasties in solid organ transplant recipients, good to excellent results of knee, shoulder and ankle replacements performed in patients with renal, hepatic, cardiac or lung transplantation have been reported. Although there was no infection in our cases, Papagelopoulos et al.7) reported 1 case of wound infection after THA in liver transplantation patients. It seems that special perioperative preparations is not necessary for wound infection, but there are still risk of wound infection in liver transplantation patients exist, so much caution for these complications are needed. Antibiotics and thrombosis prophylaxis would be given as in standard arthroplasty operations. The relatively young age of patients should be considered when choosing the type of implants and the method of fixation. Levitsky et al.8) performed a retrospective analysis on 203 liver transplant recipients who had joint arthroplasty at a single teaching institution between 1986 and 2002, and the authors concluded that joint arthroplasties may be safely and successfully performed in liver transplant recipients. These patients are certainly at increased risk for anesthesia, but with proper management and careful monitoring using the standard patient anesthesia protocol, the risk of anesthesia can be reduced to reasonable levels.
Increased numbers of liver transplantations and improved patient longevity are likely to cause a sustained increase in the incidence of osteonecrosis of the femoral head. Hence the number of relatively young patients for total hip arthroplasty will increase. This is a rare report where mini-2-incision total hip arthroplasty was done for osteonecrosis of the femoral head following liver transplantation in an Asian patient.
Figures and Tables
 | Fig. 1Preoperative radiologic evalulation of the first case. (A, B) Anteroposterior and lateral radiographs of pelvis showing a subchondral sclerosis and femoral head collapse. (C, D) MRI shows the double line sign on right femoral head at T2 weighted coronal view and the hyperintense signal change of right femoral head at T2 weighted axial view. |
 | Fig. 2Radiologic evaluation of the first case at last follow up. (A, B) Postoperative 35-month anteroposterior and lateral radiographs of pelvis showing stable bony ingrowth without radiolucent lines or migration. |
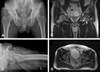 | Fig. 3Preoperative radiologic evalulation of the second case. (A, B) Anteroposterior and lateral radiographs of pelvis showing a subchondral sclerosis and femoral head collapse. (C, D) MRI shows hypointensie signal change of left femoral head at T2 weighted coronal and axial view. |
References
1. Taillandier J, Alemanni M, Samuel D, Bismuth H. Rheumatic complications following liver transplantation. Transplant Proc. 1999. 31:1717–1718.

2. Porayko MK, Wiesner RH, Hay JE, et al. Bone disease in liver transplant recipients: incidence, timing, and risk factors. Transplant Proc. 1991. 23:1462–1465.
3. Tannenbaum DA, Matthews LS, Grady-Benson JC. Infection around joint replacements in patients who have a renal or liver transplantation. J Bone Joint Surg Am. 1997. 79:36–43.

4. Hamburg SM, Piers DA, van den Berg AP, Slooff MJ, Haagsma EB. Bone mineral density in the long term after liver transplantation. Osteoporos Int. 2000. 11:600–606.

5. Mehrabi A, Fonouni H, Müller SA, Schmidt J. Current concepts in transplant surgery: liver transplantation today. Langenbecks Arch Surg. 2008. 393:245–260.

6. Lee SG. Current status of liver transplantation in Korea. Korean J Gastroenterol. 2005. 46:75–83.
7. Papagelopoulos PJ, Hay JE, Galanis EC, Morrey BF. Total joint arthroplasty in orthotopic liver transplant recipients. J Arthroplasty. 1996. 11:889–892.

8. Levitsky J, Te HS, Cohen SM. The safety and outcome of joint replacement surgery in liver transplant recipients. Liver Transpl. 2003. 9:373–376.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download