Abstract
Periprosthetic fracture of the femur is an uncommon complication after total hip arthroplasty (THA), but it appears to be increasing in incidence as a result of the aging population demographics and the increased number of THAs that are being performed. Much interest has been generated regarding low energy fractures in the elderly, but repeated periprosthetic fractures in the same femur are uncommon. The authors present here the case of a 71 year old patient who sustained repeated low energy ipsilateral periprosthetic femur fractures. The initial injury was caused by a road traffic accident, but the subsequent fractures were all caused by low energy falls. The patient sustained proximal and distal femur fractures with implants in situ. The probable causes of such fractures was a combination of systemic and local host factors, such as osteoporosis, cortical stress risers, local osteopenia secondary to bed rest, quiescent infection and altered fracture site vascularity due to the internal fixation devices and multiple re-operations.
The number of periprosthetic fractures associated with total hip arthroplasty (THA) is increasing due to longer life expectancies and the active lifestyles of THA patients. The management of periprosthetic fractures in THA patients requires substantial fracture surgery and arthroplasty expertise. Femoral fractures caused by indirect low energy trauma differ from direct impact fractures in the young, and as indicated by the volume of literature on the subject, they deserve more attention1). Prolonged bed rest and immobilization causes host bones to become more fragile and vulnerable to low energy fractures. Internal fixations further aggravate this weakness by disrupting vascularity at fracture sites and by altering load transmission to affected bone. Reduced bone quality and mechanical strength are common features of the risk factors of these pathological fractures, and may be such that the bone is unable to withstand normal physiological forces. Furthermore, this problem can be compounded by coexisting medical conditions. Here, we describe a case of multiple low energy periprosthetic ipsilateral femur fractures following repeated internal fixation. The patient provided informed consent that case data could be submitted for publication.
In September 2004, a 71 year old female diabetic patient sustained a left unstable intertrochanteric fracture during a traffic accident (Fig. 1A). The fracture was fixed with a compression hip screw at another hospital (Fig. 1B), and then changed to cemented bipolar hemiarthroplasty (Fig. 1C). Subsequently an infection developed, and as part of the treatment, Girdlestone resection arthroplasty was performed at the same hospital. However, the infection was not controlled, though curettage and debridement were performed twice. Finally, in April 2006 she was referred to our institution.
A radiograph of the left hip performed at admission revealed that the proximal femur had migrated proximally and laterally, and there was a bone cement remnant in the medullary cavity (Fig. 1D). Her contralateral femoral neck bone mineral density (BMD) was - 3.8 (T-score). A physical examination of the left hip at admission revealed the following ranges of motion; flexion 0-80°, abduction 0-30°, adduction 0-10°, and internal and external rotation both 0-10°. In addition, levels of inflammatory biomarkers were elevated, that is, white blood cell count 8700 (normal, 4000 to 10800) with neutrophilia (78%; normal, 38 to 75%), erythrocyte sedimentation rate 71 mm/hr (normal, 0 to 22 mm/hr) and C-reactive protein 0.26 mg/L (normal, <0.3 mg/L). There was pus discharge from the wound and Methicillin-resistant Staphylococcus aureus was cultured from pus.
Two-stage reconstruction was planned, and thorough debridement and prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) insertion was performed in May 2006 (Fig. 2A). PROSTALAC insertion was repeated two months later due to residual infection and dislocation of the antibiotic loaded cement cup from the acetabulum (Fig. 2B), and extended trochanteric osteotomy was performed to remove a small remnant of cement in the medullary portion (Fig. 2C). 6 weeks later after 2nd surgery in our institute, the patient fell at home and sustained a transverse periprosthetic fracture of the shaft of the left femur of type C according to the Vancouver classification2) (Fig. 2D). At this time, there was no gross evidence of persistent infection, and this was confirmed by blood investigations.
During revision surgery, there was no evidence of infection according to the frozen biopsy, and thus we proceeded with left revision THA and plating of the shaft with a nine-hole locking compression plate (LCP). The plate was fixed using both screws and Dall-Mile's cables. Her postoperative recovery was uneventful, and she was discharged with non-weight bearing crutches, and followed monthly with serial radiographs at each visit. Progressive fracture healing was noted, and there was no evidence of implant loosening. However, about 1 year after revision THA, she again had a minor fall at home, and subsequently presented at our emergency department, where a work-up revealed a supracondylar fracture of the left femur of Vancouver type C (Fig. 3). During this revision, the fracture was internally fixed with a 5 hole distal femoral LCP; in addition, the previous plate was removed. She was followed as an out patient on a regular basis and serial radiographs taken during each visit indicated fracture healing with a stable prosthesis.
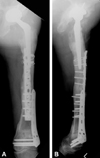
At 4 months after distal femur fracture surgery she experienced a 3rd minor fall. On this occasion, she sustained a transverse fracture of the shaft of the left femur of (Vancouver type C) between the prosthesis and distal femoral plate (Fig. 4). The fracture was internally fixed using an 11 hole LC-DC plate augmented with two Dall-Mile's cables without removing the distal femoral plate.
Patient was last seen in our out-patient clinic in March 2010 (2 year after the last plate fixation), radiographs showed that all fractures had united (Fig. 5). During this visit, a physical examination revealed 1cm of shortening of the left lower limb, but she was ambulating independently.
Periprosthetic femoral fractures are increasing as a result of changes in population demographics and the increased numbers of THAs performed. Its overall incidence has been reported to range from 0.1 to 6% of all THAs. Kavanagh et al. estimated the incidence to be 1% after primary THA and 4.2% after revision THA3).
Many review articles have discussed the incidence of periprosthetic femoral fracture, but the majority of published studies describe one type of fracture treated using a single surgical method and its outcome4,5). The management of these fractures is often demanding, complex, and expensive. In many cases, the surgeon has to solve combined problems of implant loosening, bone loss, and fracture. Optimal management strategies remain unclear, as evidenced by the large number of treatment options described in the literature and by a lack of consensus.
Osteoporosis caused by reduced structural bone strength is the main cause of these fractures, and is associated with age, disuse, and an altered bone metabolism fracture sites resulting from internal fixation. In the present patient, BMD at time of admission was -3.8 (T-scores). Eventhough this patient have had osteoporosis medication (Bisphosphonate, Calcium and VitD) since initial fracture, reductions in BMD are probably enhanced due to prolonged bed rest and decreased mobility, and these factors evidently contribute to the happening of refractures. Hence, early ambulation and increased physical therapy would improve prognosis in such patients.
Gracia et al6) reported an incidence of 1.57% for femoral shaft fractures following THA, whereas Kanavagh3) reported an incidence of less than 1%. However, the incidence is higher after revision THA, at about 4.2%3). Bethea et al. reported that 75% of periprosthetic fractures show implant loosening. Femoral fractures after THA are caused by low energy trauma, and the fracture sites are invariably between flexible and rigid areas. Between 1~2 years after THA the edges of prostheses act as stress risers, and may cause osteolysis and loosening7). Larsen et al. described factors that possibly increase the risk of secondary fracture, such as, implant loosening, osteoporosis, varus angulation of the femoral stem, calcar resorption, major capsular calcification, and cortical defects at stem tips. Accordingly, the importance of correct prosthesis insertion and of earliest mobilization after internal fracture fixation has been emphasized.
Hidaka and Gustillo reported 6 cases of refracture among 23 reported cases (4 cases with an inadequate fixation period and 2 case of non-protection). They suggested the following reasons for refracture; a) decreased load transfer at the implant site leading to thinning of the cortex, b) a compromised blood supply around the plate, and c) an altered bone metabolism around the plate. In both types of cases fractures occurred between proximal and distal implants, presumably due to the bone-weakening effect of stress concentration in these areas8).
All fractures in our patient were internally fixed using locking plates modified with the Dall-Mile's cable system. Locking plates are increasing in popularity for the treatment of low energy fractures9). These plates have two main theoretical advantages; a) improved fixation biomechanics, and b) less disruption of blood supply at fracture sites.
Complication rates for the modified cable plate system vary between 25 to 57%10). In elderly patients, general weakness may lead to trauma during ambulation and decreasing BMD, and in such patients low energy trauma can lead to fractures of this nature.
Surgeons must occasionally address fractures adjacent to fixation devices previously used for fracture management, which may require removal of the old implant, bypassing it, or incorporating it into a new construct. If an old implant is no longer functional and the old fracture has healed, the implant can be removed and a more conventional technique used to stabilize the new injury. However, if the old injury has not healed, the old device must be incorporated in the new fixation or otherwise maintained.
Inevitably, surgeons continue to produce ingenious solutions to interesting new problems, in addition to addressing the various factors discussed above. The aims of treatment are to achieve and maintain best possible reduction, ensure implant stability, accelerate bone healing, and allow earliest possible mobilization and protection to prevent further injury.
Figures and Tables
Fig. 1
(A) Anteroposterior radiograph of both hips showing an unstable left femur intertrochanteric fracture. (B) Postoperative radiograph after internal fixation with compression hip screw. (C) Postoperative radiograph after conversion to cemented bipolar hemiarthroplasty. (D) Postoperative radiograph after Girdle stone operation showing residual bone cement in the femoral canal.
Fig. 2
(A) Immediate postoperative radiograph after debridement and PROSTALAC insertion performed at our institution. Residual cement in the left femoral canal can be seen. (B) Acetabular component dislocation evident on radiograph two months after PROSTALAC insertion. (C) Osteotomy was performed, with revision and PROSTALAC change, to remove residual cement. Postoperative radiograph showing no residual cement. (D) Radiograph showing Vancouver type C periprosthetic fracture, incurred after 1st minor trauma.
Fig. 3
(A) Anteroposterior and (B) lateral radiographs of left femur after 2nd minor trauma showing comminuted distal femur supracondylar fracture. Shaft fracture shows signs of good union.

References
1. Salminen S, Pihlajamäki H, Avikainen V, Kyrö A, Bostman O. Specific features associated with femoral shaft fractures caused by low-energy trauma. J Trauma. 1997. 43:117–122.

2. Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995. 44:293–304.
3. Kavanagh BF. Femoral fractures associated with total hip arthroplasty. Orthop Clin North Am. 1992. 23:249–257.

4. Ahuja S, Chatterji S. The Mennen femoral plate for fixation of periprosthetic femoral fractures following hip arthroplasty. Injury. 2002. 33:47–50.

5. Serocki JH, Chandler RW, Dorr LD. Treatment of fractures about hip prostheses with compression plating. J Arthroplasty. 1992. 7:129–135.

6. Garcia-Cimbrelo E, Munuera L, Gil-Garay E. Femoral shaft fractures after cemented total hip arthroplasty. Int Orthop. 1992. 16:97–100.

7. Bethea JS 3rd, DeAndrade JR, Fleming LL, Lindenbaum SD, Welch RB. Proximal femoral fractures following total hip arthroplasty. Clin Orthop Relat Res. 1982. 170:95–106.

8. Hidaka S, Gustilo RB. Refracture of bones of the forearm after plate removal. J Bone Joint Surg Am. 1984. 66:1241–1243.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download