Abstract
Pyomyositis is a primary bacterial infection of skeletal muscle and this is on the increase worldwide among children as well as young adults. We report herein on a case of a 29-year-old male with pyomyositis of the obturator internus. The fact that pyomyositis predominantly affects the muscles of the lower limb and it is confined to the obturator internus muscle has been poorly recognized. CT with an enhancement was an accurate imaging modality to image the obturator internus muscle and to ascertain the diagnosis for this case. The patient was managed with antibiotics and surgical intervention was not necessary. Pyomyositis of the obturator internus muscle needs to be differentiated from septic arthritis of the hip. The present study reports the clinical signs and treatments of pyomyostis and we review the relevant literature.
The incidence of pyomyositis, initially considered to be a disease of the tropic, has been growing worldwidely, mainly affecting children and young healthy adults even in temperate climates1-3). It predominantly affects quadriceps, iliopsoas, and gluteal muscles of the lower limb in sequence4). The involvement of obturator muscles has rarely been reported and difficult to diagnosis. We report a rare case of obturator internus pyomyositis in a 29-year-old male of teraplegic condition with highlighting its importance of awareness and the relevant radiological investigations in the form of CT enhancement.
A 29-year-old male presented an acute episode of fever, body temperature of 38.2℃ and pulse of 108 per minute. He denied other systemic symptoms. Two months prior to presentation, he underwent fourth to sixth cervical anterior interbody fusion due to cervical fractures. He had a C4 ASIA (American Spinal Injury Association) impairment scale B tetraplegia with tracheostomy and foley catheter insertion. No definite abnormality was found in his chest and abdomen on physical examination. There was a mild limitation of internal rotation of the left hip. Examinations such as Patrick, Freiberg and Pace test were impossible to run due to tetraplegia. Sensory or motor deficit of his left lower limb were also unexaminable. However, all the other joints had a full range of motion and were symptom-free.
Initial laboratory studies revealed white blood cell count 13.21× 103/µℓ (neutrophils 90%), ESR (erythrocyte sedimentation rate) 36 mm/hr (reference value: 0~9 mm/hr), CRP (C-reactive protein) 85 mg/L (reference value: 1.45 mg/L). There wasn't any evidence suggesting altered immunity. Intravenous vancomycin was initiated empirically after blood cultures were taken. The blood and urine culture showed no growth of organisms. Methicillin resistant Staphylococcus aureus (MRSA) was confirmed on sputum culture. Despite intravenous vancomycin, his fever persisted.
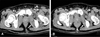
An abdomen CT demonstrated ill defined hypodense lesion with faint rim enhanced in the left obturator internus muscle (Fig. 1-A). Fat suppressed MR image only showed mild thickening with rim enhancing lesions (Fig. 2). 99 mTc CT-scan revealed nonspecific activity in the region of the left ischium, pubis and the ipsilateral acetabulum. Antibiotics regime was replaced with 3rd generation cephalosporin and metronidazole on 7th day, as from the first dose of injection. His condition improved gradually after replacing the antibiotic regime for 2 weeks. He became apyrexial, ESR and CRP dropped to reference value (Fig. 3). A follow-up of abdominal CT after two weeks revealed a diminished swelling in obturator internus muscle. It also demonstrated a calcific change and no abscess cavity in the obturator internus muscle (Fig. 1-B).
Pyomyositis is a primary, subacute and deep bacterial infection of the skeletal muscle that manifests itself as localized abscess formation, a diffuse inflammatory or a rapidly progressing myonecrotic process5). During the past decades, its incidence has been increasing in non-tropical areas also5). The usual micro-organisms are Staphylococcus aureus and Streptococcus pyogenes6). Blood cultures were positive in 31% cases of pyomyositis and purulent material obtained by needle aspiration was positive for S. aureus in 70% to 90% of patients6). Local trauma to the hip, such as a fall or strenuous exercise, seems to be the initiating factor for pyomyositis4,5). Obturator internus pyomyositis is exceptionally rare and is more common in females1). One possible explanation is the close proximity of the obturator internus muscle to the female reproductive organs1,3). We also speculate that poor personal hygiene of tetraplegic condition of the present case may contribute to pyomyositis in his pelvis. In addition, the patient can not feel pain and more attention is required because it is difficult to diagnose.
Obturator internus muscle is deep seated so that local inflammatory signs are not obvious. The clinical presentation includes fever, hip or thigh pain and inability of full weight-bearing which mimic that of septic hip or osteomyelitis7,8). However, the lack of familiarity with this entity frequently leads to a delayed diagnosis or misdiagnosis, causing severe morbidity such as septic arthritis and very rarely septicemia2,5). However, there are a number of distinguishing features between obturator internus pyomyositis and septic arthritis of hip: pyomyositis does not limit the range of motion of the hip joint dramatically with more discrete areas of tenderness including pain on rectal examination7). There may be pain radiating to the leg and there may be edema of the ipsilateral labia3,9). As laboratory findings are not highly specific, early radiological evaluation is essential: MRI seems to be the most sensitive4,7). Although MRI is superior to CT scanning, initial MRI was not diagnostic in this case7,10). CT can be also used to guide pus aspiration7,9). The present case showed that CT with enhancement also can be a diagnostic modality to detect obturator internus pyomyositis with non-obvious MR findings. Therefore for its diagnosis, surgeon needs to try careful history taking and clinical examination. In addition previous negative investigations should be repeated if clinical suspicion remains7).
In a majority of patients, treatment with appropriate antibiotics alone is sufficient4). Surgical drainage is rarely indicated if the patient fails to respond to medical therapy with unusual organism4). Antibiotics of choice should be efficient against S. aureus. Blind coverage for immunocompromised patients should include broader spectrum coverage for gram negative organisms and anaerobic organisms3,6). The duration of antibiotics has not been established and can vary from 2 to 6 weeks, depending on the clinical severity and response to antibiotics3,6). With appropriate therapeutic modality, most individuals recover completely without long-term sequelae. Therefore, early and accurate diagnosis and management based on the awareness of this unusual entity is important as obturator internus pyomyositis is curable.
Figures and Tables
Fig. 1
(A) Axial computed tomography with enhancement show ill-defined hypodense lesion in obturator internus muscle (arrow). (B) Diminished swelling and calcific change in obturator internus muscle (arrow) on follow-up computed tomography with enhancement.
References
1. Chiedozi LC. Pyomyositis. Review of 205 cases in 112 patients. Am J Surg. 1979. 137:255–259.
2. Nikolopoulos DD, Apostolopoulos A, Polyzois I, Liarokapis S, Michos I. Obturator internus pyomyositis in a young adult: a case report and review of the literature. Cases J. 2009. 2:8588.

3. Birkbeck D, Watson JT. Obturator internus pyomyositis. A case report. Clin Orthop Relat Res. 1995. 316:221–226.
4. Bansal M, Bhaliak V, Bruce CE. Obturator internus muscle abscess in a child: a case report. J Pediatr Orthop B. 2008. 17:223–224.

5. Orlicek SL, Abramson JS, Woods CR, Givner LB. Obturator internus muscle abscess in children. J Pediatr Orthop. 2001. 21:744–748.

6. Christin L, Sarosi GA. Pyomyositis in North America: case reports and review. Clin Infect Dis. 1992. 15:668–677.

7. King RJ, Laugharne D, Kerslake RW, Holdsworth BJ. Primary obturator pyomyositis: a diagnostic challenge. J Bone Joint Surg Br. 2003. 85:895–898.
8. Hakim A, Graven M, Alsaeid K, Ayoub EM. Obturator internus abscess. Pediatr Infect Dis J. 1993. 12:166–168.

9. Chatwani A, Shapiro T, Mitra A, LevToaff A, Reece EA. Postpartum paravaginal hematoma and lower-extremity infection. Am J Obstet Gynecol. 1992. 166:598–600.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download