Abstract
Purpose
This study attempted to evaluate the pattern of change of the pain after total hip arthroplasty (THA) and to confirm the effect of periarticular multimodal drug injection (PMDI) on controlling the early postoperative pain.
Materials and Methods
Of the total patients who underwent primary THA at our hospital because of osteonecrosis of the femoral head from March to October 2008, 60 patients were enrolled in this study. The subjects were divided into three groups. Groups 1 & 2 received periarticular injection. Group 1 included the patients who were injected with a combination of opioid, long-acting local anesthetics, a non-steroidal anti-inflammatory drug and epinephrine. Group 2 received a combination of morphine and ropivacaine and group 3 was not injected with any analgesics. The visual analogue scale (VAS) at 4 hours, 8 hours, 12 hours, 24 hours, 2 days, 3 days, 5 days, 14 days and 1 month after surgery, the frequency that patients pushed the self-controlled pain medication machine for 2 days after surgery and the amount of clonac that was injected according to the needs of the patients were used as objective measures.
Results
The VAS score at postoperative 4 hours to 3 days among the groups showed a significant difference (P<0.05), but the VAS scores at postoperative 5 days to 1 month among the groups showed no significant difference (P>0.05). The frequency of pushing the self-controlled pain medication machine among the groups and the amount of clonac according to the needs of the patients among the groups showed that there were significant decreases at the operation day, the postoperative 1, 2 day and the 3 days (P<0.05).
Many recent researches and studies report the good result of THA with long term follow-up2-5). Because of that, too much attention about THA is increasing. Therefore, more and more people are interested in pain and pain control after operation. Especially, effective control of pain can reduce arthrofibrosis and postoperative limitation of motion. Moreover, it can help for patients to return to early ambulation and normal walk. Like that, controlling pain after THA does not only affect on postoperative rehabilitation after surgery but also on the overall results6-8).
Various types of methods to control pain before, on and after surgery such as epidural anesthesia, intravenous dosage, intra-articular injection and oral dosage of opioid have been used after THA. In addition, recent literatures have issued the effects of multimodal pain control based on the concepts of multiple pain pathway block theory9). Periarticular injection of analgesic agent is really effective for controlling postoperative pain and can reduce the requirement of other anodynes and side effects10,11). However, there have been many controveries about the most effective combination of injection drugs for pain control after THA7,12,13) and few reports about referring the effective period of periarticular multimodal drug injection by comparing pain control patterns between injection and non-injection groups.
The purpose of this study was to systemically examine the effect of the early postoperative pain control by periarticular multimodal drug injection and define the early effective period for pain control by comparing pain control pattern among groups. Our hypothesis was that (1) combination of opioid (morphine), a long-acting local anesthetics (ropivacaine), nonsteroidal anti-inflammatory drug (ketoroloc) and epinephrine would be superior to the no injection group and combination of opiod and long-acting local anesthetics group on postoperative pain control, (2) after early effective period for pain control, no injection groups would not show significant difference compared with injection groups in the pain control pattern, (3) during early effective period for pain control, VAS score has correlation with the frequency of self-pain-control for 2 days after surgery and the amount of Clonac which was injected depending on the needs of patients.
Of the patients who underwent primary THA performed in our hospital because of osteonecrosis of femoral head from March to October 2008, 60 patients were enrolled in this study. Inclusion criteria were (1) Ficat stage III, IV patients who complained of hip pain (2) MRI grade 3, 4 by modified Kerboul method14) (3) primary THA Patients who showed an overreaction and suffered a side effect or were subjects of contraindication when using combined drugs were excluded. The subjects were divided into three groups. (1) the Group 1 included patients who were injected combination of opioid (morphine), a long-acting local anesthetics (ropivacaine), nonsteroidal anti-inflammatory drug (ketorolac) and epinerphrine into periarticular tissue, (2) the Group 2 was defined patients who were injected combination of opioid (morphine) and a long-acting local anesthetics (ropivacaine) into periarticular tissue, (3) the Group 3 was defined patients who were not injected any analgesics. The prospective randomized controlled study model was carried out.
Two-drug combination were made up with morphine HCL (5 mg) 0.5 cc, ropivacaine (400 mg) 53.3 cc and four-drug combination were made up with morphine HCL (5 mg) 0.5 cc, ropivacaine (400 mg) 53.3 cc, ketorolac (30 mg) 1cc and Epinephrine 0.6 cc. They were all diluted by normal saline (0.9%) as much as 100 ml for injection.
All the operations were carried out by single operator. Posterior approach method in lateral decubitus position was used. Proximal fitting cementless femoral stem, cementless acetabular cup and ceramic on ceramic bearing surface were used in this study. After insertion of acetabular cup and femoral stem, half of the injection (50 ml) was inoculated into anterior articular capsules, iliopsoas muscles and its insertion site before reduction. After reduction, the other 50 ml were injected into abductors, fascia lata, gluteus maximus, its insertion, posterior articular capsule, short external rotator muscle and synovial membrane before irrigation and suturing. For exact evaluation about the effects of periarticular multimodal drug injection, the self-pain-control that keromin (210 mg), fentanyl (1000 ug), zofran (8 ug) and normal saline (100 ml) were combined has been used for all the groups until the second day after surgery, under discussion with anesthesiologists. The self-pain-control was constantly injected as 15 ug/hr and the amount of volume which was injected when a patient pushed a button was 30 ug. It was Clonac (diclofenac beta-dimethylaminoethanol) that was injected following needs of patients and it was injected into muscle column as 1 ample (90 mg/2 ml) at once.
The degree of subjective pain was checked before surgery and 4 hours, 8 hours, 12 hours, 24 hours, 2 days, 3 days, 5 days, 14 days and 1 month after surgery with Visual Analogue Scale (VAS). The frequency that patients pushed self-pain-control for 2 days after surgery and the amount of Clonac which was injected depending on the needs of patients were used as objective measures.
We evaluated the VAS score and objective measures among groups on regular interval and defined the period of time that VAS score among the three groups was not shown statistical difference and named as "early effective period for pain control". Moreover, the relationship of VAS score during early effective period for pain control with the total frequency of self-pain-control for 2 days after surgery and the total amount of Clonac which was injected depending on the needs of patients. Pain control pattern and difference in each group during early effective period for pain control was also evaluated.
One-way Analysis of variance (ANOVA) test was used to analyze the change of VAS score, the frequency of self-pain-control push and cloncac in three groups. When the results showed statistical significance, Tukey B test was applied for multiple comparisons. Student's t-test was used to analyze the difference the VAS score in each group according to time. Analysis was conducted with SAS 9.1.3 system in this study. Also, the significance probability was 5%.
60 patients were enrolled in the subjects. They consisted of 24 men and 36 women and the mean age was 67.95 years(53 to 82, SD 8.31). The mean preoperative pain score (VAS) of all patients are 6.7 ± 1.39. Demographic data of each group are listed in Table 1. There were no differences in gender, age, presumed cause, height, weight, and BMI between the two groups.
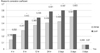
As subjective pain methods, immediate postoperative VAS scores in the group 1, 2 and 3 were 7.7 ± 1.17, 7.7 ± 0.80 and 7.5 ± 0.72, respectively. There was no significant statistical difference among groups (P=0.98). Postoperative 4 hour,8 hour,12 hour, 24 hour, 2 days and 3 days VAS scores were 6.75±1.48, 6.1±1.59, 5.6±1.50, 5.3±1.45, 4.4±1.47 and 3.75±1.29 in the group 1, 7.2±0.62, 6.8±0.52, 6.8±0.77, 6.15±0.93, 5.75±0.91 and 5.4±0.88 in the group 2 and 7.8±0.77, 7.75±0.79, 7.95±0.69, 7.85±0.59, 7.25±0.44 and 6.85±0.59 in the group 3. There was significant statistical difference among groups (P=0.008, P<0.001, P<0.001, P<0.001, P<0.001, P<0.001 respectively). VAS scores on postoperative 5 days, 2weeks and 1 month were 3.75±1.29, 3.35±1.09 and 2.95±0.94 in the group 1, 4.15±0.75, 3.60±0.75 and 3.15±0.49 in the group 2 and 4.25± 0.85, 3.65±0.59 and 3.25±0.55 in the group 3. Interestingly, there was no statistical difference at postoperative 5 days, 2 weeks and 1 month among groups (P=0.249, P=0.483, P=0.383, respectively) (Table 2). Postoperative day, postoperative 1day, postoperative 2days the frequency of PCA push were 1.6±0.99, 1.3±0.73 and 0.55±0.60 in the group 1, 2.85±0.81, 1.95±0.83 and 1.45±0.94 in the group 2 and 4.5±1.43, 3.9±1.02 and 2.7±0.80 in the group 3. The frequency of PCA push in the group 1,2 and 3 at operation day, postoperative 1 day and postoperative 2 day showed significant statistical difference (P<0.001, P<0.001, P<0.001) (Table 3). Postoperative day, postoperative 1day, 2days, 3days and 5days, the amount of Clonac which was injected depending on the needs of patients were 0.95±0.15, 0.85±0.30, 0.4±0.15, 0.25±0.5 and 0.2±0.85 in the group 1, 1.8±0.85, 1.2±1.7, 0.75±1.23, 0.4±0.43 and 0.25±0.66 in the group 2 and 2.5±1.23, 1.9±0.88, 1.2±0.56, 0.7±0.45 and 0.3±0.78 in the group 3. The amount of Clonac which was injected depending on the needs of patients in the group 1,2 and 3 at operation day, postoperative 1 day, 2 day, 3 day showed statistical difference (P<0.001, P=0.001, P=0.013, respectively) but no statistical difference at postoperative 5 day (P=0.775)(Fig. 1)
During postoperative 3 days, that is early effective period for pain control by our definition, multiple comparisons among groups were performed by the method of Tukey's B test as post-hoc test. The mean VAS score in the group 1, 2 and 3 at postoperative 4 hour were 6.75±0.54, 7.20±1.32 and 7.80±0.81 respectively. The mean VAS score in the group 1, 2 and 3 at postoperative 8 hour were 6.10±1.89, 6.80±0.29 and 7.75±1.54 respectively. No statistical difference was founded between group 1 and 2. But group 3 showed that statistical difference was founded. The mean VAS score in the group 1, 2 and 3 at postoperative 12 hour, 24 hour, 2 days and 3 days were 5.6±1.25, 5.3±0.73, 4.4±0.7, and 3.75±1.15 in the group 1, 6.8±1.27, 6.15±1.17, 5.75±1.03 and 5.4±0.3 in the group 2 and 7.95±1.7, 7.85±1.13, 7.25±0.72 and 6.85±0.34 in the group 3. At postoperative 12 hour, 24 hour, 2 days and 3 days, the mean VAS score in group 1, 2 and 3 showed statistical difference between each other groups (Fig. 2).
Pearson's correlation coefficient between the total amount of Clonac which was injected depending on the needs of patients and the mean VAS scores during postoperative 5 days were 0.146, 0.287, 0.369, 0.406, 0.426, 0.501 and 0.066. There were statistically significant relationship at postoperative 8hour, 12 hour, 24 hour, 2 days and 3 days (P<0.05). In addition, Pearson's correlation coefficient between the total frequency of self-pain-control push and the mean VAS scores during postoperative 5 days were 0.232, 0.443, 0.485, 0.581, 0.597, 0.603 and 0.070 (Fig. 3). There were also statistically significant relationship at postoperative 8 hour, 12 hour, 24 hour, 2 days and 3days (P<0.05).
Because of the prominent innovations in arthroplasty such as computer-assisted procedures15), minimally invasive technique16,17) and advanced rehabilitation protocol18), many patients underwent the major orthopaedic operation, such as THA. THA is a major orthopaedic operation associated with considerable postoperative pain. Almost all patients complain of a variety of postoperative pain because THA needed wide surgical exposure and direct trauma to the soft tissue and bone structure19). Nearly half of patient would experience severe pain immediate postoperatively and all of them wanted enough pain control20). Effective pain control will make it possible to early joint motion and it will help to prevent arthrofibrosis and return to daily life and walk. So pain control after THA will not only affect postoperative rehabilitation, but also result of operation21). Varieties of method of Postoperative pain control such as continuous epidural anesthesia, continuous infusion of local anesthetics into joint, patient controlled analgesics and peripheral nerve block have been developed and used22). Although continuous epidural anesthesia provides superior analgesia, technical difficulty and complications such as headache due to leakage of cerebrospinal fluid, neurogenic bladder, low blood pressure, respiratory depression, pulmonary hypotension and infection on the site of spinal puncture weaken the significant effect of continuous epidural anesthesia23). The continuous intra-articular local anesthetics injection is excellent on the effect of the pain control but the risk of prolonged wound drainage and intraarticular infection is high24). Patient controlled analgesia of opidoid drug is good for pain control, but complications such as nausea, vomiting, respiratory depression, drowsiness, skin hypersensitivity and neurogenic bladder will be developed25). Peripheral nerve block is difficult to do process and to block exactly26).
Periarticular multimodal drug injection for pain control in THA do act on directly on the operated lesion and decrease the local inflammation, prevent releasing pain inducing mediator, so can control effective pain. In addition the risk of systemic complication of drug will decrease. In the current literature, as the concept of Kligman et al.23) that direct injection into the synovial membrane and tendon insertion site will increase the bonding in the soft tissue, for maximizing the effect of injection, not only intra-articular injection, but also psoas, abductor, iliotibial band, gluteus maximus and it's insertion site, posterior capsule and short external rotator and synovium also was injected. Periarticular multimodal drug injection (e.g. combinations of more than two drugs, including different adjuvant agents) may reduce or even prevent postoperative pain with different mechanisms of action and reduce side effects28). That made the satisfaction of patient increased and had the purpose of promoting rehabilitation and recovery. Periarticular multimodal drug injection for pain control has been known recently10). But there are few studies of pain control for postoperative THA than total knee arthroplasty. Parvataneni et al.11) studied on 71 patients who had been operated as THA were randomly divided into two groups, 35 patients received periarticular intraoperative injection of multimodal analgesic drugs, and the others use patient-controlled analgesia. They injected periarticular area by the combination of 0.5% bupivacaine 200~400 mg, morphine sulfate 8 mg, epinephrine 1/1.000 0.3 cc, methylprednisolone acetate 40 mg, cefuroxime 750 mg. They issued on their literature that pain scores of the periarticular injected group was lower significantly than control group at poetoperative 2 and 3 days. In addition, Weng et al.27) studied seventy-six patients underwent total hip arthroplasty were randomly divided into two groups, 38 patients received periarticular intraoperative injection of multimodal analgesic drugs, and others do not. Compared to the control group, VAS for pain of the patients of injected group had significantly lower in the post-anesthetic-care unit and four hours after surgery. Patients of the injected group used significantly less patient-controlled analgesia at 6, 12 hours, and over the first 24 hours after surgery than the control group. No adverse effects resulted from the multimodal analgesic drugs were noted in the injected group. Lee et el.30) studied on 60 patients undergoing unilateral THA were randomized to undergo either a multimodal pain control protocol or a conventional pain control protocol. The following parameters were compared: the preoperative and postoperative visual analogue scales (VAS), hospital stay, operative time, postoperative rehabilitation, additional painkiller consumption, and complication rates. Although both groups had similar VAS scores in the preoperative period and on the fifth postoperative day, there was a significant difference between the groups over the four-day period after surgery. There were no differences in the hospital stay, operative time, additional painkiller consumption, or complication rate between the groups. The average time for comfortable crutch ambulation was 2.8 days in the multimodal pain control protocol group and 5.3 days in the control group.
In our study, the subject was divided into no injection group (Group 3), two drugs (morphine and long-acting local anesthetics) combined group (Group 2), and four drugs (morphine, long-acting local anesthetics, NSAID and epinephrine) combined group (Groupe 1) and evaluated the pain by subjective and objective method from immediate postoperation to 2 weeks after operation on the regular time interval. Postoperative 4 hour,8 hour,12 hour, 24 hour, 2 days and 3 days VAS score among the groups showed that there was significant difference (P<0.05), but VAS scores at postoperative 5 days, 2 weeks and 1 month among the groups showed no significant difference (P>0.05). The frequency of self-pain-control push among the groups at operation day, postoperative 1 day and 2 day showed significant statistical difference (P<0.05). The amount of Clonac by the needs of patients among groups showed that there was significant difference at operation day, postoperative 1 day, 2 day and 3 day (P<0.05).
Interestingly, we could find that after postoperative 5days, no statistical difference was found among three groups. Periarticular multimodal drug injection has effect on early period until postoperative 3 days in our study, similarly, postoperative 2, 3 days in Parvataneni's9,10) report and postoperative 1 day in Weng's7) report. That means that we can postulate the effect of periarticular multimodal drug injection would last until postoperative 3 days and this period would be important for pain control in case of periarticular injection.
The four ingredients of injection mixtures that we used were morphine, ropivacaine, ketorolac and epinephrine. Morphine exerts its analgesic effects centrally, regionally, and locally by its effect on opioid receptors. Local administration allows sustained effect with a minimum of the typical opioid adverse effects (sedation, nausea, and respiratory depression), which occur through central opioid receptors10). Its half-time is 2hours, has late onset of action time (30~60 min) but has long effect time (3~7 hour). On the contrary, ropivacaine, its half-time is 1.5 hour, has early onset (10~20 min), mean duration is short (2~5 hours) and not only block afferent peripheral nociceptive activity but also have some anti-inflammatory properties in human mucosal cells29). On the idea of the opposite effect of these two drugs, we mixed these two drugs, given that the anesthetic effect will be prompt and durable. Epinephrine which was used in the multiple drugs will have effect on decreasing movement into the systemic circulation, increasing local absorption and increase the effect time. Additionally, because of it's effect on local bleeding control, drug washed out effect while massive bleeding will be decreased10,11). Ketorolac is non-steroidal anti-inflammatory drug, half-time is 5 hour, and has onset of action time is under 60 min, mean duration is 8~12 hour, and has the effect by blocking the eicosanoid pathway which evoked the creating of inflammatory mediator29). So peripheral nerve desensitization and nociceptor activities inhibition will make the effect of pain decreasing effect29).
In the current study, for postoperative 8 hours, there were no significant statistical different VAS scores with Group 1 and Group 2. But for these 8 hours, Group 3 which do not use short acting drugs like morphine and ropivacaine was significant statistical difference with other groups. After these 8 hours, VAS score of Group 1 was significant difference with Group 2. This difference may be affected by ketorolac, as relatively long acting drug and epinephrine decreasing moving into the systemic circulation, increasing local absorption and the effect time. But we cannot tell the reason that there was no short acting drug's effect, why there were still differences with Goup 2 and Group 3 until postoperative 3 days. About this, it needs more additional study in the future.
The relationship with VAS score and the total amount of Clonac injection during early effective period for pain control was analyzed by simple correlation analysis. In same method, the relationship with VAS score and the total frequency of self-pain-control push during the early effective period for pain control was analyzed. During the early effective period for pain control, the VAS scores and the total amount of Clonac injection has the close relationship and the relationship of VAS scores and the total frequency of self-pain-control push is also, at same times. It means the higher VAS score of patients, the much Clonac use and self-pain-control push and the lower VAS score of patients, and the less Clonac use and self-pain-control push, especially, at early effective period for pain control.
There are several limitations to this study. First, there is the possibility that the analgesic effect of the periarticular multimodal drug injection was masked by the patient controlled analgesia and Clonac by needs of patients. Second, because functional evaluation was not included in the study, effect of early pain control on the function was not evaluated. Third, we did not stratify the result as to type of implant and duration of operation time. We thought that the influence of these factors seems to be low. But, we cannot eliminate the relationship between these factors and pain control pattern.
The power of this literature will be that our study was processed by blind prospective control model. Moreover, we evaluated the effectiveness of periarticular multimodal drug injection after THA by the results according to different drug combination groups. We also tried to define the early effective period for pain control.by comparing the pain control pattern and analyze the difference of pain control pattern among group.
The present study suggests that periarticular multimodal drug injection has effect on the early pain control after THA. Especially, for postoperative 3 days, namely, early effective for pain control, periarticular multimodal drug injection can has effect on the pain control and significantly reduce the requirements for PCA push and another analgesics like Clonac. In addition, the combination of morphine, ropivacaine, ketorolac and epinephrine will increase and last pain control effect during early effective period after THA.
Figures and Tables
Fig. 1
The frequency of cloncac injection following needs of patients. The amount of clonac which was injected depending on the needs of patients in the group 1,2 and 3 at operation day, postoperative 1 day, 2 day, 3 day showed statistical difference (P=0.000,0.001,0.013, respectively) but no statistical difference at postoperative 5 day (P=0.775)
* There was significant statistical difference among groups

Fig. 2
VAS score changes during postoperative 5 days. Immediate postoperative VAS scores in the group 1, 2 and 3, there was no significant statistical difference among groups(P=0.98). Postoperative 4 hour,8 hour,12 hour, 24 hour, 2 days and 3 days VAS scores were significant statistical difference among groups(P<0.05). VAS scores on postoperative 5 days, interestingly, there was no statistical (P=0.249).
* There was significant statistical difference among groups.
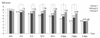
Fig. 3
The Pearson's correlation coefficient for the total amount of Clonac which was injected depending on the needs of patients and the total frequency of self-pain-control push. The relationship with VAS score-the total Clonac injection and VAS score-the total frequency of self-pain-control push was analyzed by simple correlation analysis.
* There was significant statistical difference (P<0.05)
References
1. Donald SM. Sir John Charnley (1911-1982): inspiration to future generations of orthopaedic surgeons. Scott Med J. 2007. 52:43–46.

2. Berry DJ. Long-term follow-up studies of total hip arthroplasty. Orthopedics. 2005. 28:8 Suppl. s879–s880.

3. Eswaramoorthy V, Moonot P, Kalairajah Y, Biant LC, Field RE. The Metasul metal-on-metal articulation in primary total hip replacement: clinical and radiological results at ten years. J Bone Joint Surg Br. 2008. 90:1278–1283.
4. Mullins MM, Norbury W, Dowell JK, Heywood-Waddington M. Thirty-year results of a prospective study of Charnley total hip arthroplasty by the posterior approach. J Arthroplasty. 2007. 22:833–839.

5. Yoon TR, Rowe SM, Kim MS, Cho SG, Seon JK. Fifteen- to 20-year results of uncemented tapered fully porous-coated cobalt-chrome stems. Int Orthop. 2008. 32:317–323.

6. Illgen RL, Pellino TA, Gordon DB, Butts S, Heiner JP. Prospective analysis of a novel long-acting oral opioid analgesic regimen for pain control after total hip and knee arthroplasty. J Arthroplasty. 2006. 21:814–820.

7. Maheshwari AV, Blum YC, Shekhar L, Ranawat AS, Ranawat CS. Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Relat Res. 2009. 467:1418–1423.

8. Ranawat AS, Ranawat CS. Pain management and accelerated rehabilitation for total hip and total knee arthroplasty. J Arthroplasty. 2007. 22:7 Suppl 3. 12–15.

9. Parvataneni HK, Ranawat AS, Ranawat CS. The use of local periarticular injections in the management of postoperative pain after total hip and knee replacement: a multimodal approach. Instr Course Lect. 2007. 56:125–131.
10. Parvataneni HK, Shah VP, Howard H, Cole N, Ranawat AS, Ranawat CS. Controlling pain after total hip and knee arthroplasty using a multimodal protocol with local periarticular injections: a prospective randomized study. J Arthroplasty. 2007. 22:6 Suppl 2. 33–38.

11. Andersen LJ, Poulsen T, Krogh B, Nielsen T. Postoperative analgesia in total hip arthroplasty: a randomized double-blinded, placebo-controlled study on peroperative and postoperative ropivacaine, ketorolac, and adrenaline wound infiltration. Acta Orthop. 2007. 78:187–192.

12. Ritter MA, Koehler M, Keating EM, Faris PM, Meding JB. Intra-articular morphine and/or bupivacaine after total knee replacement. J Bone Joint Surg Br. 1999. 81:301–303.

13. Ha YC, Jung WH, Kim JR, Seong NH, Kim SY, Koo KH. Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am. 2006. 88:Suppl 3. 35–40.

14. Ybinger T, Kumpan W. Enhanced acetabular component positioning through computer-assisted navigation. Int Orthop. 2007. 31:Suppl 1. S35–S38.

15. Sculco TP, Jordan LC, Walter WL. Minimally invasive total hip arthroplasty: the Hospital for Special Surgery experience. Orthop Clin North Am. 2004. 35:137–142.

16. Willems MM, Kooloos J, Gibbons P, Minderhoud N, Weernink T, Verdonschot N. The stability of the femoral component of a minimal invasive total hip replacement system. Proc Inst Mech Eng H. 2006. 220:465–472.

17. Mont MA, Seyler TM. Advanced techniques for rehabilitation after total hip and knee arthroplasty. Clin Orthop Relat Res. 2009. 467:1395.

18. Rawal N, Hylander J, Nydahl PA, Olofsson I, Gupta A. Survey of postoperative analgesia following ambulatory surgery. Acta Anaesthesiol Scand. 1997. 41:1017–1022.

19. Filos KS, Lehmann KA. Current concepts and practice in postoperative pain management: need for a change? Eur Surg Res. 1999. 31:97–107.

20. Ryu J, Saito S, Yamamoto K, Sano S. Factors influencing the postoperative range of motion in total knee arthroplasty. Bull Hosp Jt Dis. 1993. 53:35–40.
21. Mahoney OM, Noble PC, Davidson J, Tullos HS. The effect of continuous epidural analgesia on postoperative pain, rehabilitation, and duration of hospitalization in total knee arthroplasty. Clin Orthop Relat Res. 1990. 260:30–37.

22. DeWeese FT, Akbari Z, Carline E. Pain control after knee arthroplasty: intraarticular versus epidural anesthesia. Clin Orthop Relat Res. 2001. 392:226–231.
23. Stein C. The control of pain in peripheral tissue by opioids. N Engl J Med. 1995. 332:1685–1690.

24. Allen HW, Liu SS, Ware PD, Nairn CS, Owens BD. Peripheral nerve blocks improve analgesia after total knee replacement surgery. Anesth Analg. 1998. 87:93–97.

25. Kligman M, Bruskin A, Sckliamser J, Vered R, Roffman M. Intra-synovial, compared to intra-articular morphine provides better pain relief following knee arthroscopy menisectomy. Can J Anaesth. 2002. 49:380–383.

26. Rasmussen ML, Mathiesen O, Dierking G, et al. Multimodal analgesia with gabapentin, ketamine and dexamethasone in combination with paracetamol and ketorolac after hip arthroplasty: a preliminary study. Eur J Anaesthesiol. 2010. 27:324–330.

27. Weng WJ, Wang F, Chen DY, Yuan T, Xu ZH, Jiang Q. Observation of the efficacy of local multimodal analgesic drugs injection in total hip arthroplasty. Zhongguo Gu Shang. 2008. 21:834–836.
28. Karmakar MK, Ho AM, Law BK, Wong AS, Shafer SL, Gin T. Arterial and venous pharmacokinetics of ropivacaine with and without epinephrine after thoracic paravertebral block. Anesthesiology. 2005. 103:704–711.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download