Abstract
Introduction
We wanted to evaluate the efficacy of bipolar hemiarthroplasty using Berger's two-incision surgical technique for patients with muscular weakness around the hip joint and/or a high risk of dislocation.
Materials and Methods
We performed bipolar hemiarthroplasty for 15 femoral neck fractures using Berger's two-incision technique between December 2005 and July 2007. The mean age of the patients was 75.2 years old. Four of them had difficulty in walking due to the sequalae after stroke and five have been treated for psychoneurologic disorders. We investigated the operation time, the length of the anterior and posterior incisions, the amount of bleeding, the time untill walking after the operation, the total hospital stay, the recovery to activities of daily living and the complications such as dislocation.
Results
The mean operating time was 93 minutes. The average anterior and posterior skin incision length was 6.4 cm and 7.2 cm, respectively. The mean amount of bleeding was 420 cc at the time of surgery and 230 cc postoperatively through a drain. The patients started walking at a mean of 3.3 (1 to 5) days after the operation and the mean hospitalization was 24.3 days. Fourteen patients went back to their pre-injured activities of daily living, except one case with an intraoperative periprosthetic fracture. As for complications, two cases (13.3%) of femoral fracture were intraoperatively observed and one case of skin necrosis on the anterior incision site occurred. There were not any cases of dislocation or infection.
As our society is aging and the number of elderly people is increasing, so is the incidence of femoral neck fracture. The goal of surgical treatment of femoral neck fracture in the elderly is to enable the patient to walk early, to reduce complications caused with bed rest, and to restore patients to their pre-injured state as soon as possible. We assume hip arthroplasty is the most appropriate therapeutic method for femoral neck fracture to obtain this goal in the elderly1,2).
Minimal invasive total hip arthroplasty performed recently produce lesser soft tissue injury and makes an earlier recovery comparing to conventional methods3-6). We considered that minimal invasive techniques had the advantage of allowing patients to walk earlier and faster rehabilitation in the elderly and in the patients with muscle weakness around the hip joint. We performed bipolar hemiarthroplasty using Berger's surgical technique3) in the elderly and in the patients with muscle weakness and psychoneurologic problems and studied the availability of our new surgical technique.
From December 2005 to July 2007, we performed minimal invasive bipolar hemiarthroplasty using Berger's two-incision technique for 15 femoral neck fractures. There were six male and nine female patients, with a mean age of 75.2 years (57 to 87 years). Of the 15 cases, four had difficulty in walking due to stroke; three used a cane and one used a wheelchair. Five of them have been treated for dementia or other psychogenic disorders. Except patients with stroke, 10 patients walked without walking aids. Our surgical technique was used in the selected patients such as hemiplegia and dementia at the early stage and then it was extended into other patients.
We used cementless femoral stems; including Taperloc stem (Biomet, Warsaw, IN) in thirteen cases, ABG-II stem (Howmedica, UK) in one case and Versys stem (Zimmer, Warsaw, IN) in one case, and UHR bipolar cups (Stryker, NJ, USA) in all cases.
We did not use any restraints for positioning of the legs on the bed after the operation and we allowed the patients to walk after removing the suction drain. We began rehabilitation with a tilting table and parallel bar for the patients who could not walk because of hemiplegia and we let them use a wheelchair if they wanted. We investigated the operation time, the length of the anterior and posterior incision, bleeding amount, the time to walk after operation, the total hospitalization period, the degree of recovery to activities of daily living, and complications such as dislocation. An average of follow-up was 39 months (29~48 months).
Patients were positioned on the radiolucent operation table in a supine position. Five to seven centimeters anterior skin incision began along the femoral neck under fluoroscopy (Fig. 1). In this procedure, we had to be careful not to injure lateral femoral cutaneous nerves. After the skin incision, we could exposure the joint capsule by retracting the tensor fasciae latae laterally and rectus femoris and sartorius medially after approaching between tensor fasciae latae and sartorius (Fig. 2). After ligating the lateral femoral circumflex artery, which runs along the capsule anteriorly, we could expose the femoral neck by incising the capsule vertically along the femoral neck. Taking a double neck cutting, we removed the femoral head after taking out the bone segment of the neck. Posterior incisions of five centimeters in length, which was for insertion of the femoral stem into the femur, was placed posterosuperiorly from the tip of greater trochanter. After reaming and rasping for the femoral stem under fluoroscopy, we inserted the bipolar cup through the anterior incision first; the liner and cup of the UHR (Universal Head Replacement) bipolar cup were assembled in the factory, and then the femoral stem through the posterior incision. And after mounting the hip ball on the stem through the anterior incision, we pushed to insert the hip ball into the bipolar cup to assemble under direct vision (Fig. 3).
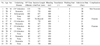
The mean operation time, from skin incision to closure, was 93 minutes (75~130 minutes). The mean incision length was 6.4 cm (6~7 cm) anterior and 7.2 cm (7~8 cm) posterior. The mean amount of total bleeding was 420 cc (300~700 cc) during the operation and 230 cc (70~250 cc) postoperatively. Four patients who showed lower than 8 g/dL of hemoglobin required transfusion. Patients started walking in a mean of 3.3 days (1 to 5 days) after the operation and the mean hospital stay was 24.3 days (15~61 days); other underlying problems made it longer. 14 patients were back to pre-injured activities of daily living, except one case with an intraoperative periprosthetic fracture. Three patients of them with stroke walked with a cane and one patient with a wheelchair in the last follow-up. 10 patients walked without walking aids. Intraoperative periprosthetic fractures happened in two cases and the fractures were treated with circular wiring after extension of the posterior incision distally. One of them had a good outcome with a proper rehabilitation program but the other, with a comminuted fracture, had fair results with some restriction in activities. Skin necrosis on the anterior incision site occurred in one case. There were no dislocation and infection (Table 1).
The numbers of femoral neck fracture have been increasing with age and a proper surgical treatment is required. Arthroplasty is one of recommendable treatment for the elderly and severe osteoporotic patients who are not suitable for internal fixation1,2,5). Arthroplasty makes it possible for the patients to start walking early and to get back to their previous activities, and it reduces complications caused by bed rest.
Recently, minimal invasive surgical techniques, compared to conventional methods, shortened the time of recovery to the pre-injured state. This minimally invasive surgical technique preserves adjacent soft tissue including muscles and tendons, which makes early rehabilitation possible and hospital stay shorter. Berger3) introduced minimal invasive arthroplasty using two-incisions, on the anterior and posterior of the hip joint. As it minimizes muscular injury and reduces pain, it makes the patients begin to walk early and hospital stay shorter. Hur et al.5) reported that elderly patients who received two-incision total hip replacement for femoral neck fractures, in a mean age of 72 years old, started walking with aids in a mean of 2.3 days after the operation and all of them could walk without aid for at least 30 minutes at the final follow-up.
The authors thought that minimally invasive hip replacement is more available for elderly patients and patients with muscular weakness than younger patients. Hip replacement, using the two-incision technique, can reduce or avoid injuries to the anterior muscles as it approaches the joint capsule between the tensor fasciae latae and the sartorius. The gluteus medius and minimus can be injured during femoral procedures7,8), but muscular damage can be minimized. We dissected posterior capsule enough through anterior incision and it allowed appropriate exposure to clean the medial aspect of the greater trochanter and enabled reaming and rasping with a correct position, and then we split gluteal muscles along the direction of the muscular fiber, which minimized muscular injury. In our study, the mean age was 75.2 years old and nine of the 15 had dementia or hemiplegia. Patients started walking in an average of 3.3 days after the operation. There were no significant difference in the time of walking after the operation between the patients with muscular weakness due to stroke and ordinary patients. We assumed that early rehabilitation was possible even in the patients with muscular weakness because of hemiarthroplasty using a minimally invasive surgical technique which produced the least muscle injuries.
Macaulay9) reported that total hip replacement has better results in the treatment of femoral neck fractures in elderly patients than hemiarthroplasty. On the other hand, Iorio10) reported that the incidence rate of dislocation in the group of femoral neck fractures was five times higher than in the group of degenerative osteoarthritis after receiving a total hip replacement. Hur5) reported two cases of dislocation that happened in two incision total hip arthroplasty for femoral neck fracture in elderly patients and both of them had muscle weakness. Ninh11) said central nerve disorders such as dementia, epilepsy and paralysis are risk factors for dislocation after hip arthroplasty in elderly people. In our study, nine of the 15 had low activity because of dementia or hemiplegia. According to the result of the studies of Hur5), Iorio10), and Ninh11), the possibility of dislocation should not be overlooked. Especially in the patients with higher risk factors, extra awareness is required to prevent dislocation. We did not restrict any posture and apply any brace even for three patients with dementia. We also allowed a patient with hemiplegia to use a wheelchair as early as possible after operation. We believe that two-incision hemiarthroplasty gives the hip joint enough stability and makes all theses acceptance possible. In addition, as two-incision hemiarthroplasty is very stable in all directions, the doctors and nurses did not have to spend much time with the patients to prevent dislocation. Without any restraint in their activities the patients had no dislocation. These promising results were owing to the stability of the bipolar cup itself and the minimal muscle injury around the hip joint.
In this study, the mean operating time was 93 minutes (75~130 minutes). The operation time was longer than conventional technique. We think that operation time can be shortened as going through running curve period but we do not think it will be shorter than conventional techniques. Bleeding amount was not increased to the prolonged operation time. Postoperative bleeding was lesser than conventional methods. Only four of 15 patients need blood transfusion after operation. We think that perservation of musculature with minimal muscle injury at the surgery reduced the amount of bleeding.
Intraoperative periprosthetic fractures occurred in two cases. The fractures were fixed with circular wiring through the anterior skin incision. It was difficult to detect intraoperative fractures on fluoroscopic images. It was easy to find fractures through an anterior skin incision. In our first operation using two-incision technique, as too small skin incision gave us poor field of vision, an excessive traction caused skin necrosis on the anterior site. This complication did not happened in the conventional methods until that time, so particular caution is needed in the two-incision technique not to make too small incision and to avoid excessive traction.
The limitations of our study are the small sample size and the lack of general popularity because of confined selection. We think further investigations and researches are essential to develop the new operation technique.
Even though two-incision hemiarthroplasty was not a common surgical procedure for femoral neck fractures, we think this new surgical technique has some advantages in the treatment of femoral neck fracture in the elderly with high risk of dislocation as well as in the patients with psycho-neurological disorders such as dementia and stroke. We recommend this technique for femoral neck fracture in the elderly, especially for the surgeons who are familiar to Berger's two-incision technique.
Figures and Tables
 | Fig. 1Anterior skin incision is placed directly over the femoral neck and posterior skin incision is started from greater trochanter. |
 | Fig. 2After retraction of the tensor facia lata laterally and sartorius and rectus femoris medillay, anterior joint capsule is visible. |
References
1. Jain NB, Losina E, Ward DM, Harris MB, Katz JN. Trends in surgical management of femoral neck fractures in the United States. Clin Orthop Relate Res. 2008. 466:3116–3122.

2. Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fracture: a meta-analysis of 14 randomized studies with 2,289 patients. Acta Orthop. 2006. 77:359–367.

3. Berger RA. Total hip arthroplasty using the minimally invasive two-incision approach. Clin Orthop Relat Res. 2003. 417:232–241.
4. Bal BS, Lowe JA. Muscle damage in minimally invasive total hip arthroplasty: MRI evidence that it is not significant. Instr Course Lect. 2008. 57:223–229.
5. Hur CI, Yoon TR, Park KS, Cho SG, Yim JH. Minimally invasive two-incision total hip arthroplasty for treating acute displaced femoral neck fractures in active elderly patients. J Korean Orthop Assoc. 2008. 43:643–650.

6. Yoon TR, Bae BH, Choi MS. A modified two-incision minimally invasive total hip arthroplasty: technique and short-term results. Hip Int. 2006. 16:Suppl 4. 28–34.

7. Meneghini RM, Pagnano MW, Trousdale RT, Hozack WJ. Muscle damage during MIS total hip arthroplasty: Smith-Petersen versus posterior approach. Clin Orthop Relat Res. 2006. 453:293–298.
8. Woolson ST. In the absence of evidence--why bother? A literature review of minimally invasive total hip replacement surgery. Instr Course Lect. 2006. 55:189–193.
9. Macaulay W, Nellans KW, Iorio R, Garvin KL, Healy WL, Rosenwasser MP. DFACTO Consortium. Total hip arthroplasty is less painful at 12 months compared with hemiarthroplasy in treatment of displaced femoral neck fracture. HSS J. 2008. 4:48–54.

10. Iorio R, Healy WL, Lemos DW, Appleby D, Lucchesi CA, Saleh KJ. Displaced femoral neck fractures in the elderly: outcomes and cost effectiveness. Clin Orthop Relat Res. 2001. 383:229–242.
11. Ninh CC, Sethi A, Hatahet M, Les C, Morandi M, Vaidya R. Hip dislocation after modular uniploar hemiarthroplasty. J Arthroplasty. 2009. 24:768–774.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download