Abstract
Purpose
The purpose of this study was to analyze the cause of failure of acetabular component cases after metal-on-metal primary total hip arthroplasty using RB Wagner acetabular cup.
Materials and Methods
Between January 1993 and January 2005, we retrospectively studied failure cause of 27 patients who underwent acetabular revision surgery among 468 consecutive cementless total hip arthroplasties using RB Wagner acetabular component. The duration of primary arthroplasty to revision ranged from 5.1 years to 11.5 years (mean 9.2 years). The clinical evaluation was performed using preoperative and last follow-up modified Harris hip scores. The radiological evaluation was performed in terms of the stability, such as inclination, anteversion, cup size, acetabular bone coverage, osteolysis, radiolucency and gap.
Results
The average Harris hip scores was 49.6 preoperatively and 91.3 at the most recent follow-up. In revision cases, the score was 41.2 to 51.7. Among 468 cases, 27 patients underwent revision surgery (7%, 27/468) and there was no osseointegration in all cases. The radiological evaluation in revision cases revealed inclination (46.04±5.328, p=0.0031), anteversion (14.14±2.95, p=0.584), cup size (54 mm±2.5, p=0.042) and acetabular bone coverage (67.9%±4.77, p=0.003). Focusing on the relation between disease entities, there was relatively high risk in patients with hip dysplasia (Fisher's exact test, p=0.0095).
The total hip arthroplasty using metal on metal articulation with stainless steel was first introduced in 1938 by Wiles1) and the modification of this articulation with cobalt-chrome has been performed by many other orthopedic surgeons. After the McKee's report on the poor result as high as 50% of failure rate during 15 years follow-up in 1972, the use of metal on metal articulation was decreased. Metal on metal articulation had a major problem focusing on aseptic loosening which shortened the longevity of the prosthesis. So, second generation metal on metal articulation to reduce polyethylene debris which increased osteolysis and total amount of wear rate was developed2,3). Many authors4,5) have reported good results of a new metal on metal articulation consisted with a Cobalt-Chrom-Molybdenum alloy (Metasul®: Sulzer Medica, Winterthur, Switzerland) especially in young active and middle aged patients.
We performed total hip replacement arthroplasty with second generation metal on metal articulation on 468 hips and analyzed the clinical and radiologic outcomes and the failure cause in revision cases. We experienced modern metal on metal total hip arthroplasty using roughly blasted Wagner acetabular cup. In some cases, we used grit-blasted CLS® or Wagner cone prosthesis®.
The purpose of this study was to evaluate the clinical results with modified Harris hip score and radiologic assessments with inclination, anteversion, cup size, acetabular bone coverage, radiolucency, gap and osteolysis and the factors affecting the failure rate in middle-aged patients with second generation metal on metal prosthesis designed to promote the osseointegration between bone and implant interface.
Between January 1993 and January 2005, 386 consecutive patients (468 hips) underwent primary total hip arthroplasty with the metal on metal prosthesis by single surgeon. 254 patients were male and female were 132. The mean age of the patients at the arthroplasty was 48.9 years (range, 26 to 73 years). The mean duration of follow-up to revision was 9.2 years (range, 5.1 to 11.5 years). The primary diagnosis was osteonecrosis in 268 hips, osteoarthritis in 111, sequelae of dysplastic hip in 21, femoral neck fracture in 35, sequelae of pyogenic arthritis of hip in 16, ankylosing spondylitis in 13, sequelae of tuberculous hip arthritis in 2, giant cell tumor in femoral head and neck in 2. Among 31 patients who performed revision surgery, 4 patients (4 hips) were excluded because all the components had been removed and antibiotic cement beads inserted to control deep infection.
The total hip prosthesis used for this study was the Metasul® metal on metal articulation, which consisted of 28 mm size metal femoral head with CoCrMo alloy, titanium shell with UHMWPE and CoCrMo articular surface(Protasul®-21 WF) and CLS® or Wagner cone® femoral stem. The RB Wagner acetabular cup is a modular acetabular implant which consists of a hemispherical titanium shell and a polyethylene insert with a CoCrMo inlay (Metasul®, Sulzer Medica). The acetabular cup had a 2.4-mm-thick CoCrMo alloy articular surface molded into ultrahigh molecular weight polyethylene with titanium of the back side. The titanium shell has characteristic structure of the outer sandblasted surface to promote the osseointegration, which has a thin metal back with multiple screw holes on the superior half surface and the small projected pegs on the other side around the equator. Cementless anchorage of the shell into the acetabulum is achieved by press-fit technique and subsequent osseointegration. On the femoral side, we used 2 types of femoral stem, such as CLS® stem and Cone prosthesis®. CLS® stem (Sulzer Medica, Winterthur, Switzerland) was a proximally fluted, grit-blasted titanium alloy prosthesis intended for press-fit only and was used routinely to almost patients. The other stem was cone stem (Cone prosthesis®, Protek AG, Berne, Switzerland). Cone prosthesis® was a collarless cone-shaped titanium stem with a coarse-blasted surface on whole length of the stem and spindle-shaped distally with 8 longitudinal ribs to provide stable fixation against rotational torque during femoral stem insertion and initial stability before osseointegration. It has advantages of even distribution of axial loading into the femoral shaft and less shear stress due to its unique feature. We used this type of femoral stem to the patients with narrow femoral canals.
All operations were performed by one surgeon using anterolateral hip approach with supine position. The acetabular component was inserted by press-fit methods after under-reaming by 2 mm, checked the intraoperative stability and reinforced by one or more screws if needed. Postoperatively, the patients were laid to the bed with skin traction in hip abduction position during postoperative one week. The patients were instructed to bear 50% of their weight with the aid of 2 crutches for 1 week. In the following 4 weeks, the patients were allowed to bear weight as tolerated with the aid of 2 crutches.
Clinical evaluations were performed at three, six, and twelve months and yearly thereafter. We assessed modified Harris hip scores preoperatively and at each follow up examination and at any change in the situations. Modified Harris hip scores6) were classified as excellent (90 to 100 points), good (80 to 89 points), fair (70 to 79 points) and poor (less than 70 points). We closely observed the development of inguinal pain maybe due to the unstable acetabular components.
Radiologic evaluation was performed by inclination, anteversion, cup size, acetabular bone coverage, radiolucency, gap and osteolysis. Radiolucency was defined as an 2 mm radiolucent change between the bone-implant interface which had not been present on the immediate postoperative radiograph and we defined it was clinically significant when it was over 50% of each zone. Gap7) was any linear radiolucency that was observed on the immediate postoperative radiograph. Periprosthetic cystic or scalloped lesions exceeding 2 mm in diameter that had not been present on the immediate postoperative radiograph were defined as osteolysis8). Any change at the bone-implant interface and in dimension and location of osteolytic lesions were recorded according to the 3 zones described by DeLee and Charnley on the acetabular side9) and 7 zones of the femoral side by Gruen10). The femoral stem was defined as neutral position within 5° angulation between the long axis of femoral shaft and implant and varus position on medial inclination over 5° and valgus on lateral. The stem was considered to be unstable when there was over 4 mm differences of the length from the tip of greater trochanter of the femur to the tip of femoral stem compared with immediate postoperative radiograph, any change in stem position and continuous widening of radiolucent line over 2 mm8). The analyses were perfomed using the SAS 9.1(SAS Institue, Cary, NC) and statistically significant association was assumed if p<0.05.
The mean preoperative modified Harris hip score of 49.6 points improved to 91.3 points. But, in patients who underwent revision surgery, the mean modified Harris hip score was 41.2 points preoperatively and 51.7 points postoperatively. All of them suffered inguinal pain in 17 hips, buttock pain in 7 and limping gait in 14.
The revision rate of primary total hip arthroplasty was 7% (27/468) in total patients, 4% (11/254) in male and 12%(16/132) in female (P<0.05). The cases which were performed revision arthroplasty due to deep infection were all males. Preoperative diagnoses who underwent revision surgery were osteonecrosis in 9 hips (3%, 9/268), osteoarthritis in 5(5%, 5/109), sequelae of dysplastic hip in 9(43%, 9/21) (P<0.05), femoral neck fracture in 2(3%, 1/35), sequelae of pyogenic arthritis in 1(6%, 1/16), ankylosing spondylitis in 1(7.6%, 1/13). This statistical analysis was made by Mann-Whitney test and Fisher's exact test (Table 1).
The mean inclination was 38° in non-performed revision arthroplasty, and 46° in performed revision arthroplasty (P<0.05). The mean anteversion was 13° in non-performed revision arthroplasty, and 14° in performed revision arthroplasty (P>0.05). The mean cup size was 56 mm in non-performed revision arthroplasty, and 54 mm in performed revision arthroplasty (P<0.05). The mean acetabular bone coverage rate was 82% in non-performed revision arthroplasty, and 68% in performed revision arthroplasty (P<0.05). 5 acetabular components has initial gaps, 2 in zone I and 3 in zone III. There were 38 radiolucent lines more than 2 mm around 19 acetabular components. Only one radiolucent line was located in zone II, the other 37 radiolucent lines were located in either zone I or zone III.
Almost femoral stem were inserted into neutral position and nine cases into varus position ranged from 6° to 8°. There was no change of stem position during follow up periods. Radiolucent line was observed around femoral stem in 12 patients (12/468, 3%). All of them were found in zone I (9 cases) and zone VII (3 cases) of Gruen's seven zones, but there were no interval change in follow up radiographs and no clinical symptoms or signs. 2 cases has subsidences over than 4 mm, but we have closely observed because they had no significant clinical symptoms (Table 2).
The reason for acetabular revision was radiolucency or osteolysis in 22 hips, protrusio acetabuli in 2, hip dislocation in 1, periprosthetic fracture in 1, broken screw in 1.
We focused on 22 radiolucency or osteolysis cases. In operative field, all retrieved acetabular components easily dropped out and had not osseointegration but fibrous ingrowth. Also, They had focal osteolysis on acetabular side which was not seen on follow up radiographs and a little metallosis around joint capsule and periprosthetic tissue. Microbiologic study was performed during surgery and the results were negative findings. The patients underwent revision surgery with acetabular reinforcement ring, such as Ganz ring(Protek AG, Berne, Switzerland).
Nowadays total hip replacement arthroplasty is commonly performed surgical options to improve pain, functional result and social activity for the patients with disable hip diseases after the introduction of cemented hip prosthesis by Charney7). As the development of modern cementing technique, the aseptic loosening decreased and longevity of femoral components increased, but loosening of acetabular component is the major problem in cemented implants19). So non-cemented acetabular component was widely used after 1980's.
The main goal of this non-cemented fixation method is osseointegration. The osseointegration is defined as a direct structural and functional connection between living bone and the surface of a load-carrying implant by Branemark4). There are several factors determining the interfacial response to foreign material and osseointegration including 1) material biocompatibility, 2) implant design, 3) implant surface, 4) state of the host bed, 5) surgical technique used at insertion and 6) loading conditions. Albrektsson et al1) have demonstrated that it is possible to osseointegrate bone cell into the surface of titanium, zirconium, and niobium metals without interference of fibrous or cartilaginous tissue. Threaded implants have a good initial resistance to shear stress if inserted with a proper technique. The implant surface is important for osseointegration. A noninfected and bloody bone bed seems to be more imperative for proper osseointegration. Premature loading will stimulate the formation of fibrous tissue instead of the desired interfacial bone formation9,21).
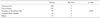
The RB Wagner acetabular cup consists of a hemispherical titanium shell and a polyethylene insert within CoCrMo inlay. The shell has a convex outer surface which is rough-blasted in order to promote osseointegration. The proximal half of the shell has openings for optional countersunk cancellous bone screws for initial stability. The distal half of the shell has sharp-edged pyramid-like pegs which penetrate into the cancellous bone during impaction(Fig. 1). Although the characteristic design of RB Wagner acetabular cup is considered to promote the osseointegration, there was no osseointegration in all of our revision cases(Fig. 2).
Many factors affecting the longevity of prosthesis are the condition of acetabular subchondral bone, material of acetabular components, patient factors, such as age, weight, leg-length and social activity, contact area of cup and acetabulum, fixation method of acetabular components, abductor offset and a kind of femoral stem.
Our study shows relatively high failure rate in women as similar to Brujin's report5). It is explained by the higher prevalence of osteoporosis in women18). In our revision cases, the acetabular inclination has the statistical significance, but generally accepted inclination of acetabular component is ranged from 30° to 50°. Focusing on the acetabular coverage, Anderson and Harris2,14) suggested that for stable fixation of acetabular components, 70 to 80% of acetabular coverage was needed. Our revision cases have revealed 68% of acetabular bone coverage, that implied to use slightly large acetabular components for the real acetabular size, it may be a technical problem on the other hand. But, there was no differences in cases with or without additional screw fixation in follow-up.
Especially patients whose initial diagnosis was sequelae of dysplastic hip had relatively high revision rate in comparison with other disease criteria in our cases (P<0.05). One of the major problem during the performance of total hip arthroplasty for sequelae of dysplastic hip is reconstruction of the true acetabulum. Several method to achieve sufficient acetabular bone coverage for sequelae of dysplastic hip is to perform more reaming medially, to shift high hip center and to use a small cup and so on. In the situation we could not regain sufficient acetabular bone coverage, the simple method to resolve this problem is to use a small cup15). Comparing to the Japanese whose physique is similar to us, acetabular components with a diameter of less than 50 mm are frequently used in many cases. But we used 50 mm to 54 mm sized acetabular cup (mean 53.2 mm) for the sequelae of dysplastic hip, it was presumed our acetabular components was a little big or medialization of acetabulum was slightly insufficient on that point of view. Azhar3) have reported that to enhance the osseointegration of porous coated implant, impaction of periphery area of acetabular component rather than polar region was important, which led to limit access of wear particle to the retroacetabular bone and resist osteolysis. This may result in smaller acetabular bone coverage and this is maybe another technical demanding problem.
Demmelmeyer et al23). have reported that the overall survival rate of the RB Wagner cup was 93.1%(95/102) at 12 years. Also, we believe that Metasul® metal on metal articulation has many benefits to reduce the wear particles and improve the longevity of the implants through our results. But RB Wagner acetabular cup has its characteristic feature as sandblasted outer-surface with multiple elevated screw holes and projected pegs. Although multiple screw holes make a surgeon fix it toward more desirable direction into large bone stock and the pegs increase initial stability, but these unique features might work as a potential defect of own. In our experience, outer prominences of these screw holes and pegs disturb intimate initial contact between acetabular bony surface and outer shell of the cup. It is prominent when hard subchondral bone is underreamed or subchondral sclerosis is more severe.
When a cup is not impacted and immerged into the cancellous bone enough, these prominences are act as a fulcrum on the hard bony surface and make it difficult to get a primary mechanical stability due to micromotion. On the contrary to the inventor's intention, their ace acts as a adverse effect. We guess that such a phenomenon is exaggerated when bony coverage is insufficient with cup malposition such as inappropriate inclination or dysplastic acetabulum. This explanation shows why our failure cases are related to dyspalstic hip.
We recommend that when a RB Wagner cup is applied, care should be taken to expose cancellous part of the acetabular base with enough reaming to accept these prominences of the outer shell and also to get a correct cup position. In our point of view, this type of the cup design is not suitable for dysplastic hip with shallow and deformed acetabulum.
Figures and Tables
 | Fig. 1A RB Wagner acetabular cup has a titanium shell with sandblasted outer surface for promotion of osseointegration. The proximal half has openings for optional screws for initial stability and distal half has sharp-edged pegs for penetration into cancellous bone. |
 | Fig. 2A 66 years old woman with hip dysplasia underwent primary total hip arthroplasty using RB Wagner acetabular cup and cone stem. After 6 years, she visited us with symptom of limping and inguinal pain. Modified Harris hip score was 42 point at postoperative one year and it was shift to 52 point at last follow up. On plain radiographs, inclination was 45, anteversion was 15.5, acetabular coverage was 68% and cup size was 54mm at one year after surgery. At last follow up, the cup showed migration into superolaterally and increased inclination. She was performed revision surgery and we have taken close observation to her. (A) preoperative radiograph of left side dysplastic hip (B) postoperative one year follow up radiograph (C) postoperative 6 year follow up radiograph in failure (D) after revision with Ganz cup with cemented technique. |
References
2. Chan FW, Bobyn JD, Medley JB, Krygier JJ, Yue S, Tanzer M. Engineering issue and wear performance of metal on metal hip implants. Clin Orthop Relat Res. 1996. 333:96–107.
3. Renawat CS, Deshmukh RG, Peters LE, Umlas ME. Prediction of the long-term durability of all-polyethylene cemented sockets. Clin Orthop Relat Res. 1995. 317:89–105.
4. Dowdy PA, Rorabeck CH, Bourne RB. Uncemented total hip arthroplasty in patients 50 years of age or younger. J Arthroplasty. 1997. 12:853–862.

5. Fye MA, Huo MH, Zatorski LE, Keggi KJ. Total hip arthroplasty performed without cement in patients with femoral head osteonecrosis who are less than 50 years old. J Arthroplasty. 1998. 13:876–881.

6. Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969. 51:737–755.

7. Schmalzried TP, Harris WH. The Harris-Galante porous-coated acetabular comoponent with screw fixation. Radiographic analysis of eighty-three primary hip replacements at a minimum of five years. J Bone Joint Surg Am. 1992. 74:1130–1139.

8. Kim SY, Kyung HS, Ihn JC, Cho MR, Koo KH, Kim CY. Cementless Metasul metal-on-metal total hip arthroplasty in patients less than fifty years old. J Bone Joint Surg Am. 2004. 86-A:2475–2481.

9. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976. 121:20–32.

10. Gruen TA, McNeice GM, Amstutz HC. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979. 141:17–27.
11. Charnley J. Total hip replacement by low-friction arthroplasty. Clin Orthop Relat Res. 1970. 72:7–21.

12. Morscher E, Schmassmann A. Failures of total hip arthroplasty and probable incidence of revision surgery in the future. Calculations according to a mathematical model based on a ten years' experience in total hip arthroplasty. Arch Orthop Trauma Surg. 1983. 101:137–143.

13. Bra-nemark PI, Zarb GA, Albrektsson T, Rosen HM. Tissue-integrated prostheses. Osseointegration in clinical dentistry. Plastic and Reconstructive Surgery. 1986. 77:496–497.

14. Albrestsson T, Albrestsson B. Osseointegration of bone implants. A review of an alternative mode of fixation. Acta Orthop Scand. 1987. 58:567–577.

15. Uhthoff HK. Mechanical factors influencing the holding power of screws in compact bone. J Bone Joint Surg Br. 1973. 55:633–639.

16. Schatzker J, Horne JG, Sumner-Smith G. The effect of movement on the holding power of screws in bone. Clin Orthop Relat Res. 1975. 111:257–262.

17. Bruijin JD, Seelen JL, Feenstra RM, Hansen BE, Bernoski FP. Failure of the Mecring screw-ring acetabular component in total hip arthroplasty. A three to seven-year follow-up study. J Bone Joint Surg Am. 1995. 77:760–766.

18. Linder L, Carlsson A, Marsal L, Bjursten LM, Branemark PI. Clinical aspects of osseointegration in joint replacement. A histological study of titanium implants. J Bone Joint Surg Br. 1988. 70:550–555.

19. Anderson MJ, Harris WH. Total hip arthroplasty with insertion of the acetabular component without cement in hips with total congenital dislocation or marked congenital dysplasia. J Bone Joint Surg Am. 1999. 81:347–354.

20. Hartofilakidis G, Karachalios T. Total hip arthroplasty for congenital hip disease. J Bone Joint Surg Am. 2004. 86-A:242–250.

21. Jasty M, Anderson MJ, Harris WH. Total hip replacement for developmental dysplasia of the hip. Clin Orthop Relat Res. 1995. 311:40–45.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download