Abstract
Background and Purpose
Exercise is recommended for every patient with Parkinson's disease (PD). The effectiveness of two different forms of exercise for PD, Tai Chi and combined stretching-strengthening exercise, was compared.
Methods
Patients with mild-to-moderate PD were recruited to join either the combined stretching-strengthening exercise group (n=7), the Tai Chi group (n=9), or the control (nonintervention) group (n=7). Exercise was performed three times a week over a period of 8 weeks. The Tai Chi exercise was led by certified instructors based on a Tai-Chi-for-arthritis program. The combined stretching-strengthening exercise comprised folk dancing, stepping, and elastic-band exercises. The subjects' functional fitness, parkinsonian symptoms, quality of life (QoL), and depression were evaluated.
Results
Both exercise groups yielded better results in their overall functional fitness after the intervention. However, no improvement with exercise was found for parkinsonian symptoms, as evaluated using the Unified Parkinson's Disease Rating Scale. With respect to the domains of QoL, the combined stretching-strengthening exercise group fared better in the social domain of QoL, and the Tai Chi group fared better in the emotional domain, while QoL and depression worsened in the control group. The postintervention QoL was improved relative to the control condition only for the Tai Chi group. Although the exercise interventions did not have any effect on depression, the control group was associated with a significant deterioration.
Go to : 
Exercise has been recommended for patients with Parkinson's disease (PD) regardless of their disease status or ongoing management.1 Various types of exercise have been tested, and the results have demonstrated the benefits of exercise relative to no intervention. Studies have also provided evidence for the use of exercise as an adjunctive management strategy for PD.2 Some researchers have suggested that the neuroprotective effects of exercise could contribute to a decrease in the risk of developing PD or could slow down the progression of neurodegeneration.3,4 In spite of the growing attention being given to the notion of exercise as a therapy for PD, only a few practical guidelines for the clinical application of physical therapy have been produced.5 Several exercise types have been recommended for PD, including Tai Chi, yoga, lunges, and Pilates.1,6
Tai Chi is a traditional Chinese martial art that was developed in the 13th century, and it has been widely practiced for centuries with various modifications.7 Tai Chi combines deep breathing and relaxation with slow and gentle movement while maintaining good postures. It also involves slow and graceful stepping movements with full weight-bearing on both lower extremities, which demands a considerable amount of work by the leg muscles.8 The benefits of Tai Chi exercise have been documented for stress reduction, improved agility and balance, postural control, and lower-extremity strength in elderly people.9-12 Tai Chi has been shown to improve measures of quality of life (QoL) and balance in people with PD.13,14 However, better outcomes compared to those in a non-intervention control group have been demonstrated for various types of exercise, but not yet for Tai Chi. Therefore, the benefits of Tai Chi exercise for patients with PD were identified in the present study by measuring functional fitness and QoL for patients with PD carrying out either Tai Chi or combined stretching-strengthening exercise (comprising folk dancing, stepping, and elastic-band exercises).
Go to : 
The patients with PD who were recruited from a university hospital to take part in this study had all been under stable management for more than 6 months. They were diagnosed by movement specialists based on clinical criteria.15 Patients with mild-to-moderate PD were recruited (n=36), while those with severe motor complications, dementia, or psychiatric symptoms that would prevent participating exercise program regularly were excluded. Patients were consecutively assigned to the combined exercise group, the control (nonintervention) group, or the Tai Chi exercise group. The patients' medications were not changed during the 8-week intervention period.
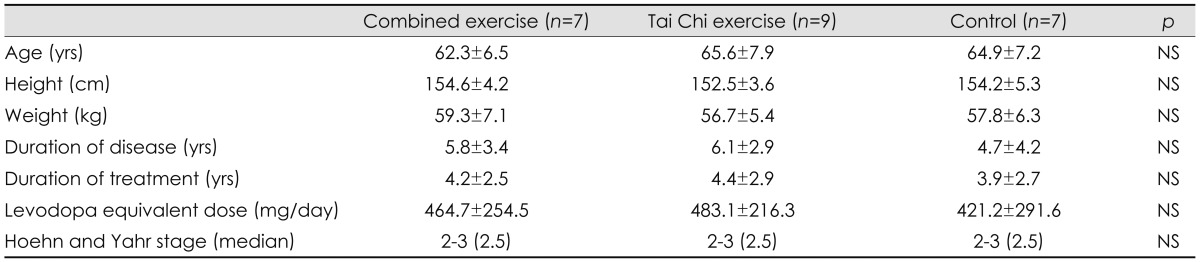
Of the 36 patients who were initially enrolled, 27 participated in more than 80% of the program. However, analysis was only carried out on the data for the 23 female patients, since the number of male patients was too small. Of the nine patients who failed to finish the exercise programs, four withdrew their consent to be involved and stopped the program (due to participation in another clinical trial for two, and unknown reasons for two), and five patients attended less than 80% of the program (due to distance and transportation issues for three patients and motor disability for two patients). The demographic, physical, and clinical characteristics of patients did not differ significantly between the groups (Table 1). All of the patients provided written informed consent to participate in this study, which was approved by the local institutional review board.
The exercise program was performed three times a week for 8 weeks. Each session consisted of 5-10 minutes of warming up, 40-50 minutes of the main exercise, and 5 minutes of cooling down. The combined exercise program was designed to enhance cardiovascular endurance, physical strength and endurance, coordination, and balance. It commenced with rhythmic movements with modified folk dancing and stepping exercises, followed by elastic-band exercises for physical strength and endurance. The intensity of the exercise program increased from a perceived exertion rating of 11-13 (fairly light to somewhat intense) to 11-15 (fairly light to intense), based on Borg's scale.16
The Tai Chi exercise used in this study was based on a Tai-Chi-for-arthritis program, which comprises 12 movements in the Sun style.17 The Tai Chi exercise session also included warm-up, main exercise, and cool-down periods using its own movements. Walking forward and stepping sideways with varying degrees of arm movements were incorporated into the 12 movements. Certified instructors taught each movement with repetition before proceeding to the next movement. After learning the sequence of each movement, patients were asked to focus on an upright posture, weight transfer, and relaxation breathing.
The Unified Parkinson's Disease Rating Scale (UPDRS) was used to evaluate parkinsonian symptoms.18 The Schwab and England scale measuring daily activity was also used to evaluate the daily lives of the patients.19 Depressive symptoms were evaluated using Beck's Depression Inventory.20 Disease-specific QoL was measured using De Bore's PD QoL scale.21 The patients' functional fitness was evaluated based on the method of Rikli and Jones.22 The chair-stand test and arm-curl test were used to evaluate the strength of the lower and upper limbs. The flexibility of the upper and lower limbs was evaluated using the back-scratch and chair sit-and-reach tests. Agility was tested with the 8-foot (1.5 m) up-and-go test, and the 6-minute walk test was used to test cardiovascular endurance.
The SPSS software (ver. 18.0, SPSS Inc., Chicago, IL, USA) was used for statistical analysis. The effects of exercise intervention in each group were analyzed by the Wilcoxon signed-rank test. The Kruskal-Wallis test was used to compare overall group differences, and post-hoc analysis was performed using the Mann-Whitney U test. The level of statistical significance was set at P<0.05, and a Bonferroni-corrected p value of <0.05/3 was used for the post-hoc tests due to multiplicity.
Go to : 
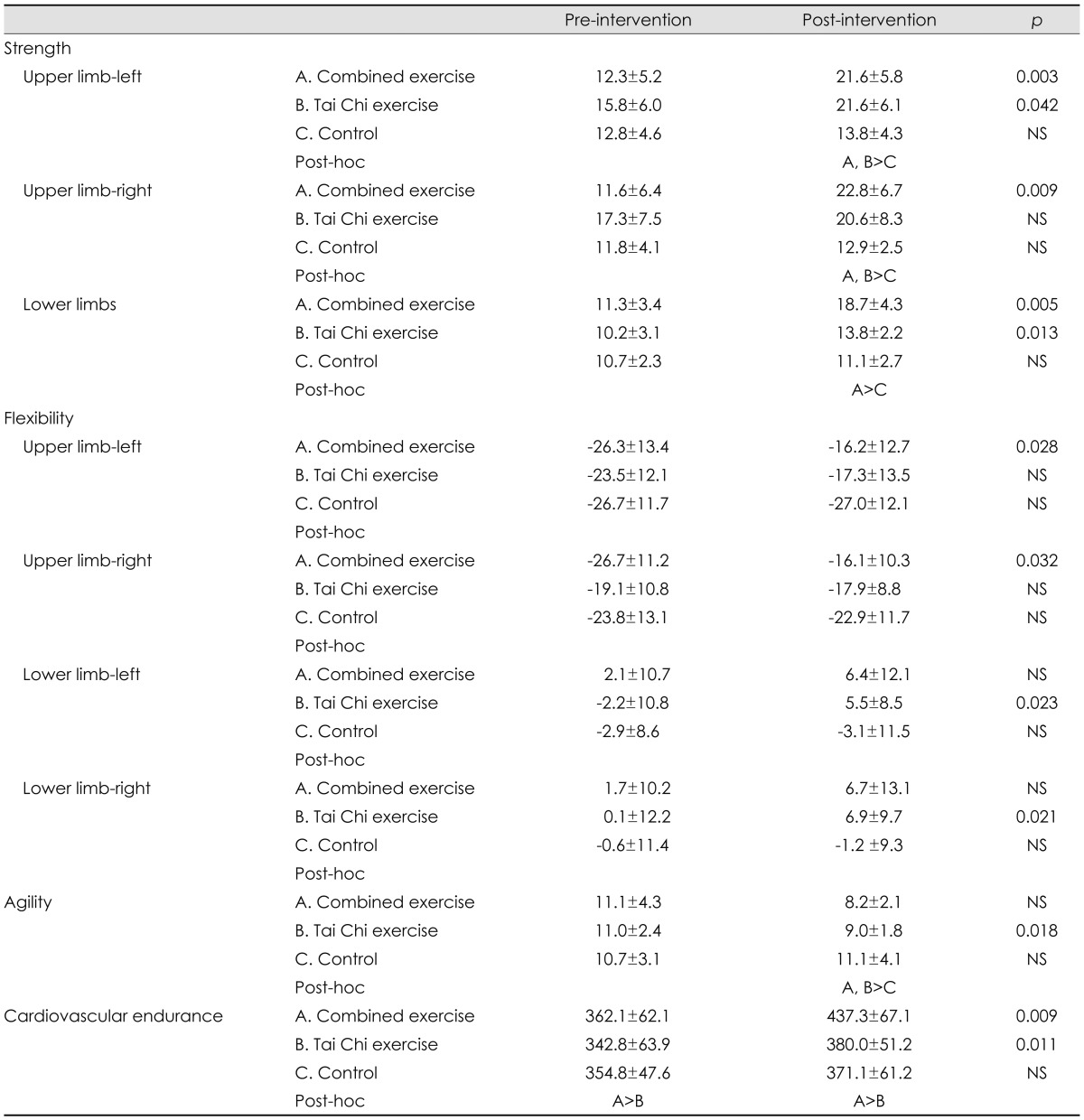
There were improvements in physical function in both exercise groups compared to the control group (Table 2). Specifically, the strength of the upper and lower limbs improved over the intervention period in both exercise groups and was better than that in the control group after the intervention. While postintervention improvements were seen in the flexibility of the upper limbs in the combined exercise group, and in lower-limb flexibility the Tai Chi exercise group, flexibility did not differ significantly between any of the groups after the intervention. Agility appeared to have improved over the intervention period in both exercise groups, but only significantly so for the Tai Chi group. However, agility was significantly better in both exercise groups than in the control group after the intervention. Basal cardiovascular endurance in the combined exercise group was better than in the Tai Chi group; however, both groups did better after exercise intervention, while there was no significant change in endurance over the 8 weeks in the control group.
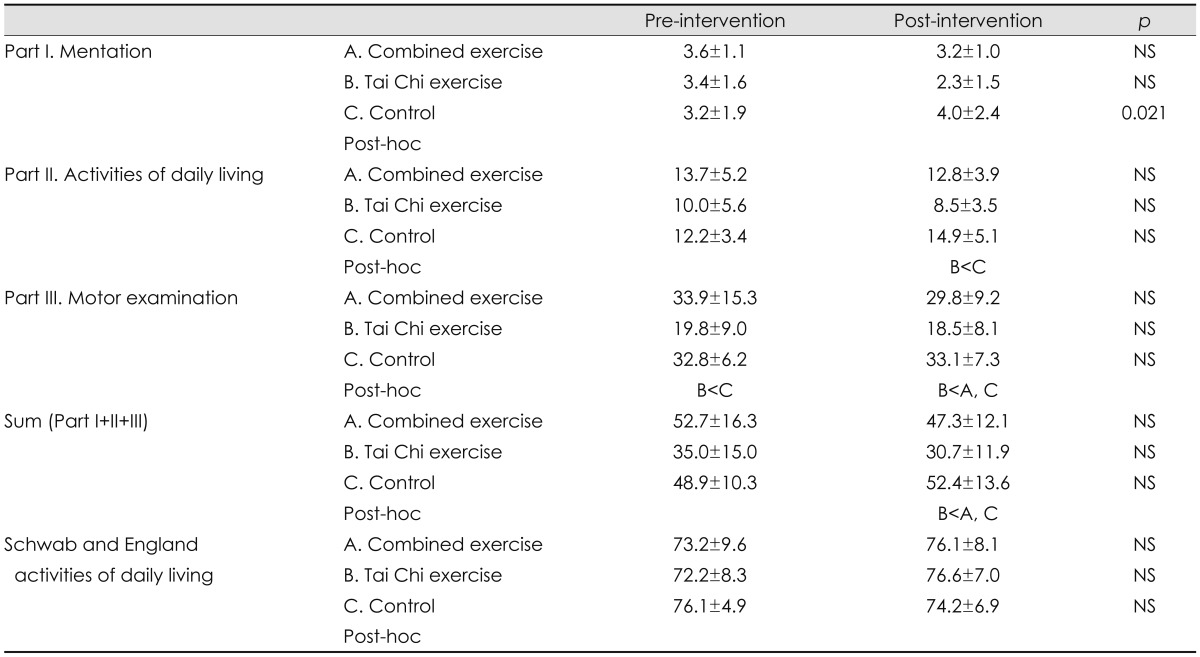
While the basal UPDRS score was lower in the Tai Chi group than in the other two groups, the difference was not statistically significant (Table 3). There was a tendency toward an improvement in UPDRS score in both exercise groups after the intervention, but again, the differences did not reach the statistical significance. Worsening symptoms during the 8-week observation period were observed in the control group, according to part I (mentation) of the UPDRS.
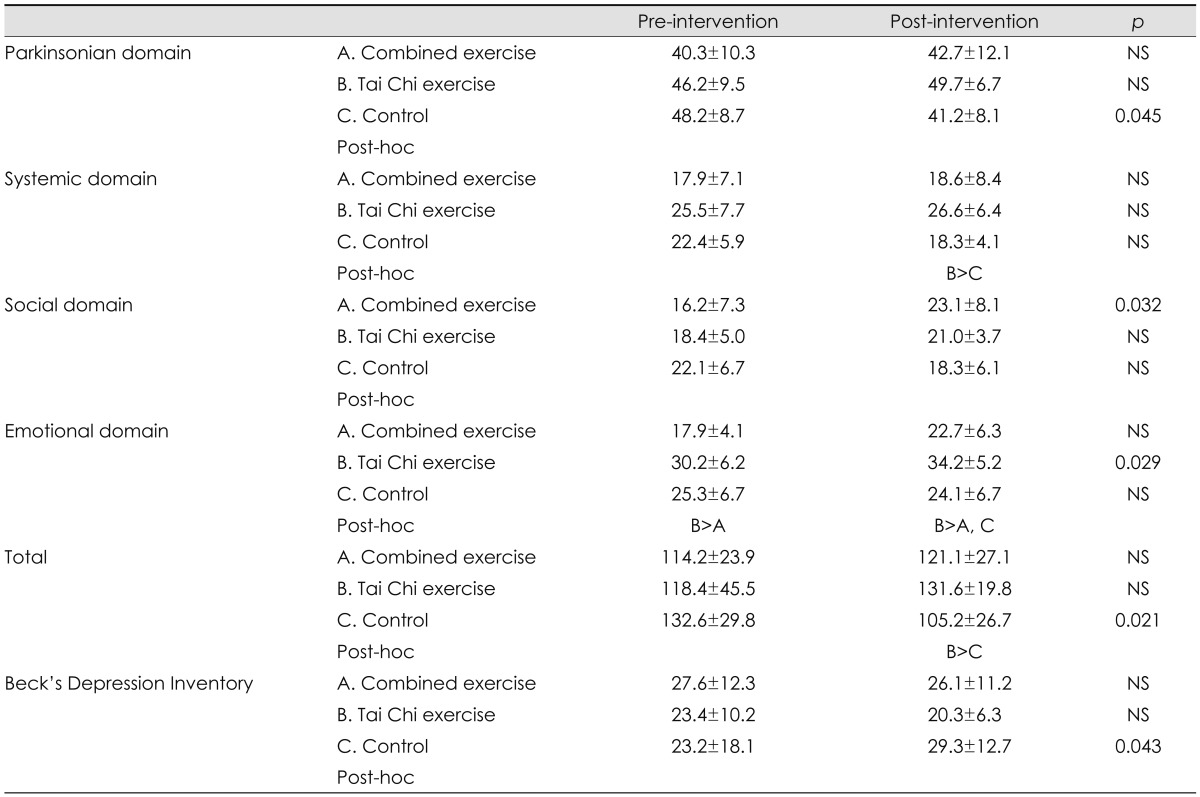
The total scores for the QoL scale in both exercise groups exhibited a tendency to improve, whereas those in the control group worsened significantly during the 8-week intervention (Table 4). The combined exercise group scored better in the social domain, and the Tai Chi group scored better in the emotional domain. Beck's Depression Inventory score increased significantly in the control group but tended to decrease in the exercise groups; however, it did not differ significantly between the groups.
Go to : 
This study found that 24 sessions of exercise performed over 8 weeks could improve the functional fitness of PD patients. Fitness was evaluated by assessing strength, flexibility, agility, and cardiovascular endurance. The combined exercise group performed better than the other groups for measures of strength, flexibility of the upper limbs, and cardiovascular endurance, while the Tai Chi group performed better for measures of flexibility, strength of the lower limbs, agility, and cardiovascular endurance. Those in the combined exercise group mainly experienced benefits pertaining to the strength of the upper and lower limbs; thus, strengthening exercise using an elastic band and rhythmic movements with folk dancing and stepping were effective for some parameters of fitness, but not for flexibility and agility. The strength and flexibility of the lower limbs improved in the Tai Chi exercise group, in line with Tai Chi working the leg muscles, even though the movements were slow and relaxed. The improved agility observed in the Tai Chi exercise group, as shown by the 8-foot up-and-go test, could be attributed both to the observed strengthening of lower limbs and to the weight shifting and transference that is practiced in Tai Chi exercise. These findings suggest that Tai Chi exercise is effective for improving the gait disturbance of the PD. However, better strength and agility results were found for both exercise groups in an intergroup comparison, with an improving tendency shown for all measurements. Therefore, it can be concluded, as from other studies,23-25 that any type of exercise is beneficial for improving the functional fitness of PD patients.
The parkinsonian symptoms had not improved significantly in any group after the intervention. Longer interventions are needed to reveal any benefits of exercise programs on parkinsonian symptoms. However, several studies have demonstrated an improvement in the UPDRS score after 4-6 weeks of intervention.26,27 Unfortunately, these positive results were taken from the intensive interventions in rehabilitation units, and subsequently declined between 6 weeks and 6 months after the intervention. These findings suggest that it is important for patients to be satisfied with the intervention program, and to enjoy it, thereby noticing the difference that it makes to their lives.
QoL measurements showed a tendency toward improvement in both exercise groups, but not a significant one. However, a significant improvement was found in the social domain of QoL in the combined exercise group, and in the emotional domain for the Tai Chi group. One interpretation of these different findings is that they are a direct result of the characteristics of the exercise being performed, such that the intimate contact with a partner or group in an activity such as folk dancing contributed to the improvement in social contact in the combined exercise group, while the quiet environment and slow movements of Tai Chi improved the patients' emotional well-being. A significant worsening in QoL and depression was observed among the control group during the 8-week period. It is well known that depression is prevalent in PD and has a big impact on the daily life of patients.28
Hackney and Earhart29 compared the effects of various exercise interventions, including Tai Chi and several types of dance, on QoL. They held 20 intervention sessions over a period of 10-13 weeks (i.e., 1-2 sessions per week). A better QoL outcome was found only for the partnered-tango sessions. They suggested that it was partnership with a caregiver that made the difference, and that dancing could be a good exercise for patients with PD. Similar improvements in the social domain of QoL were found for the combined exercise group in the present study. The caregiver's burden should be regarded as an important aspect of the management of PD, and dancing together could be good exercise for both the patient and caregiver. Given the findings of the present study, it is perhaps surprising that QoL was not improved for any of the other interventions, including Tai Chi. However, they reported an improvement in balance measurements with a Tai Chi exercise intervention at the same intensity and for the same duration.14 The question arises, then, as to why the patients failed to show any improvement in QoL with Tai Chi despite improvements in other measures. There are several explanations for those results. The first is the pluralism of Tai Chi. Tai Chi is an evolving art, and new styles have been developed based on unique insights.30 The most popular style is the Yang style, and Hackney and Earhart's study was based on 12 forms within the Yang style. However, the Sun style is easier than the Yang style because it involves more-upright postures, the movements are smaller, and there is a greater focus on breathing. In the present study, the Tai Chi for arthritis program based on the Sun style was implemented, which is easy to follow, well known, and has proven efficacy.31,32 The differences in the results between the study of Hackney and Earhart and the present study could be attributable to the different styles and teaching systems used. The program used herein would have been easier for our patients to follow and enjoy, and may therefore have had a greater positive effect on their daily life. Another possibility is the difference in the intensity of the exercise; although there are no guidelines regarding the intensity and duration of exercises recommended for PD, Tai Chi is an aerobic exercise with moderate intensity.33 It was safe, and the patients experienced no problems in practicing Tai Chi exercises three times a week for about 1 hour. Three sessions per week may be a better frequency for PD patients than only once or twice, since it would enable them to learn the exercises more quickly and to practice more. It could give them more confidence and satisfaction than practicing twice in a week, especially when they are learning a brand new and complicated exercise such as Tai Chi.
This study was subject to several limitations. First, there was only a small number of participants and all of them were female, which could limit the generalizability of the results. Furthermore, a blind evaluation was not possible, and the analysis was conducted based on a per-protocol analysis. A randomized, blind study with a larger group of patients is needed to provide more concrete evidence of the effectiveness of exercise programs. Another limitation of this study was the high drop-out rate (9/36 participants). Although no adverse events were recorded during the program, there were various factors that made attending three sessions per week difficult, such as motor disability and transportation problems. The drop-out rates were similar in the two exercise programs, but initially it was not easy to engage the participants' interest in Tai Chi. The development of a simple, easy-to-learn, and enjoyable exercise program that does not require specific equipment or specialized places would be hugely advantageous in this regard.
In summary, the present results show that exercise can improve the functional fitness and QoL of PD patients. Tai Chi yielded comparable improvements in functional fitness and a better outcome for parkinsonian symptoms and QoL than combined exercise, and could thus be a good exercise strategy for patients with PD.
Go to : 
Acknowledgements
This study was supported the Dong-A University Research Fund (to SM Cheon) and Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Education, Science and Technology (NRF-2008-532-E00024).
Go to : 
References
1. Olanow CW, Watts RL, Koller WC. An algorithm (decision tree) for the management of Parkinson's disease (2001): treatment guidelines. Neurology. 2001; 56(11 Suppl 5):S1–S88. PMID: 11402154.

2. Ransmayr G. Physical, occupational, speech and swallowing therapies and physical exercise in Parkinson's disease. J Neural Transm. 2011; 118:773–781. PMID: 21461962.

3. Ahlskog JE. Does vigorous exercise have a neuroprotective effect in Parkinson disease? Neurology. 2011; 77:288–294. PMID: 21768599.

4. Hirsch MA, Farley BG. Exercise and neuroplasticity in persons living with Parkinson's disease. Eur J Phys Rehabil Med. 2009; 45:215–229. PMID: 19532109.
5. Keus SH, Bloem BR, Hendriks EJ, Bredero-Cohen AB, Munneke M. Evidence-based analysis of physical therapy in Parkinson's disease with recommendations for practice and research. Mov Disord. 2007; 22:451–460. quiz 600. PMID: 17133526.

6. King LA, Horak FB. Delaying mobility disability in people with Parkinson disease using a sensorimotor agility exercise program. Phys Ther. 2009; 89:384–393. PMID: 19228832.

8. Han A, Robinson V, Judd M, Taixiang W, Wells G, Tugwell P. Tai chi for treating rheumatoid arthritis. Cochrane Database Syst Rev. 2004; 3:CD004849. PMID: 15266544.

9. Jin P. Efficacy of Tai Chi, brisk walking, meditation, and reading in reducing mental and emotional stress. J Psychosom Res. 1992; 36:361–370. PMID: 1593511.

10. Tse SK, Bailey DM. T'ai chi and postural control in the well elderly. Am J Occup Ther. 1992; 46:295–300. PMID: 1566796.

11. Wolf SL, Barnhart HX, Ellison GL, Coogler CE, et al. The effect of Tai Chi Quan and computerized balance training on postural stability in older subjects. Atlanta FICSIT Group. Frailty and Injuries: Cooperative Studies on Intervention Techniques. Phys Ther. 1997; 77:371–381. discussion 382-384. PMID: 9105340.
12. Li F, Harmer P, McAuley E, Duncan TE, Duncan SC, Chaumeton N, et al. An evaluation of the effects of Tai Chi exercise on physical function among older persons: a randomized contolled trial. Ann Behav Med. 2001; 23:139–146. PMID: 11394556.
13. Klein PJ, Rivers L. Taiji for individuals with Parkinson disease and their support partners: a program evaluation. J Neurol Phys Ther. 2006; 30:22–27. PMID: 16630368.
14. Hackney ME, Earhart GM. Tai Chi improves balance and mobility in people with Parkinson disease. Gait Posture. 2008; 28:456–460. PMID: 18378456.

15. Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Arch Neurol. 1999; 56:33–39. PMID: 9923759.

16. Borg G. Borg's Perceived Exertion and Pain Scales. Champaign, IL: Human Kinetics;1998.
17. Lam P. New horizons ... developing tai chi for health care. Aust Fam Physician. 1998; 27:100–101. PMID: 9503718.
18. Fahn S, Elton RL; UPDRS Program Members. Unified Parkinson's disease rating scale. In : Fahn S, Marsden CD, Goldstein M, Calne DB, editors. Recent Developments in Parkinson's Disease. Vol 2. Florham Park, NJ: Macmillan Healthcare Information;1987. p. 153–163.
19. Schwab JF, England AC. Projection technique for evaluating surgery in Parkinson's disease. In : Gillingham FJ, Donaldson MC, editors. Third Symposium on Parkinson's Disease. Edinburgh: E & S Livingston;1969. p. 152–157.
20. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961; 4:561–571. PMID: 13688369.

21. de Boer AG, Wijker W, Speelman JD, de Haes JC. Quality of life in patients with Parkinson's disease: development of a questionnaire. J Neurol Neurosurg Psychiatry. 1996; 61:70–74. PMID: 8676165.

22. Rikli RE, Jones CJ. Development and validation of a functional fitness test for community-residing older adults. J Aging Phys Act. 1999; 7:129–161.

23. Dibble LE, Hale T, Marcus RL, Gerber JP, Lastayo PC. The safety and feasibility of high-force eccentric resistance exercise in persons with Parkinson's disease. Arch Phys Med Rehabil. 2006; 87:1280–1282. PMID: 16935068.

24. Hirsch MA, Toole T, Maitland CG, Rider RA. The effects of balance training and high-intensity resistance training on persons with idiopathic Parkinson's disease. Arch Phys Med Rehabil. 2003; 84:1109–1117. PMID: 12917847.
25. Scandalis TA, Bosak A, Berliner JC, Helman LL, Wells MR. Resistance training and gait function in patients with Parkinson's disease. Am J Phys Med Rehabil. 2001; 80:38–43. quiz 44-46. PMID: 11138953.

26. Marchese R, Diverio M, Zucchi F, Lentino C, Abbruzzese G. The role of sensory cues in the rehabilitation of parkinsonian patients: a comparison of two physical therapy protocols. Mov Disord. 2000; 15:879–883. PMID: 11009194.

27. Comella CL, Stebbins GT, Brown-Toms N, Goetz CG. Physical therapy and Parkinson's disease: a controlled clinical trial. Neurology. 1994; 44(3 Pt 1):376–378. PMID: 8145901.
28. Hong SK, Park KW, Cha JK, Kim SH, Chun DY, Yang CK, et al. Quality of life in patients with Parkinson's disease. J Korean Neurol Assoc. 2002; 20:227–233.
29. Hackney ME, Earhart GM. Health-related quality of life and alternative forms of exercise in Parkinson disease. Parkinsonism Relat Disord. 2009; 15:644–648. PMID: 19329350.

30. Wayne PM, Kaptchuk TJ. Challenges inherent to t'ai chi research: part II-defining the intervention and optimal study design. J Altern Complement Med. 2008; 14:191–197. PMID: 18446928.

31. Uhlig T, Fongen C, Steen E, Christie A, Ødegård S. Exploring Tai Chi in rheumatoid arthritis: a quantitative and qualitative study. BMC Musculoskelet Disord. 2010; 11:43. PMID: 20205741.

32. Song R, Lee EO, Lam P, Bae SC. Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. J Rheumatol. 2003; 30:2039–2044. PMID: 12966613.
33. Taylor-Piliae RE, Froelicher ES. Effectiveness of Tai Chi exercise in improving aerobic capacity: a meta-analysis. J Cardiovasc Nurs. 2004; 19:48–57. PMID: 14994782.
Go to : 




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download