Abstract
Background and Purpose
The aims of this study were to determine the 28-day and 1-year survival rates after first-ever ischemic stroke and to identify their baseline predictors.
Methods
We prospectively and consecutively collected data on 300 patients with first-ever acute ischemic stroke admitted to 2 major neurological institutions for cerebrovascular diseases in Belgrade during March 2008. The Kaplan-Meier method was used to estimate the cumulative 28-day and 1-year survival rates, and the predictive values of different variables were assessed by Cox proportional-hazards regression model.
Results
The cumulative 28-day and 1-year survival rates of ischemic stroke patients in the cohort were 81.0% and 78.3%, respectively. The multivariate predictive model revealed that hypertension (p=0.017), National Institutes of Health Stroke Scale score (p=0.001), and in-hospital medical complications (p=0.029) were significant unfavorable independent outcome predictors, while early physical therapy (p=0.001) was a significant favorable prognostic factor for the 28-day mortality in our patients. Multivariate Cox regression analysis showed that age (p=0.001), National Institutes of Health Stroke Scale score (p=0.001), and in-hospital complications (p=0.008) remained significant predictors of 1-year mortality.
Stroke is a major health problem in Serbia, being the leading cause of mortality in females (20.8% of all deaths) and the second leading cause in males (15.5%).1-3 Stroke mortality rates are known to vary greatly between countries and geographic regions,4 hence requiring country-specific prevention and therapy strategies focused on mortality risk.5
The 28-day case-fatality ratio (CFR) in patients with ischemic strokes reportedly varies from 10% to 26% in different populations, while the 1-year CFR varies from 26% to 32%.6 The ability to accurately predict the outcome in stroke victims is very important for clinical practice and research,6-9 and it could also be used to select specific management strategies and set realistic therapeutic goals, to improve discharge planning, and anticipate the need for rehabilitation and community support.10 The outcome of ischemic stroke is influenced by many factors, especially the stroke subtype, and in general the prognosis for short-term survival is better for patients with small-artery occlusion (SAO).6,7 The CFR was highest for cardioembolic (CE) and large-artery atherosclerosis (LAA) subtypes of ischemic stroke [according to Trial of Org 10172 in Acute Stro-ke Treatment (TOAST) criteria].7,8
Despite the large number of clinical studies, there are still many open questions regarding the importance of the determinants of outcome after stroke. Age and severity of stroke are well established predictors of stroke survival,11,12 but many other less-reliable prognostic factors have also been suggested by various studies. The most commonly reported predictors have included the presence of atrial fibrillation, diabetes, hypertension, decreased level of consciousness, glucose level on admission, and previous transient ischemic attacks.6,11-13 Long-term survival is also influenced by several cardiovascular risk factors, but the highly variable reports have prevented a consensus.11,14,15
The purposes of this study were to determine the 28-day and 1-year survival rates after first-ever ischemic stroke and to identify their baseline predictors in the population of Belgrade, Serbia.
The study included 300 consecutive patients with first-ever acute ischemic stroke who were admitted to 2 major neurological institutions for cerebrovascular diseases in Belgrade during March 2008: 1) the Department for Emergency Neurology, Clinic of Neurology, Clinical Center of Serbia, and 2) the Hospital for Prevention and Treatment of Cerebrovascular Diseases St. Sava. All patients were residents of the Belgrade municipality and were participants of a population-based stroke-incidence study organized in Belgrade during 2008. Belgrade covers an area of 3222 km2 and consists of 17 municipalities with approximately 1.6 million inhabitants. More than 90% of all stroke patients in Belgrade area are treated in the two hospitals included in this study.
All cases had undergone a standardized neurological assessment at admission (which was the baseline point of this study). The evaluation included information on demographic characteristics, personal and family histories, and common vascular risk factors. A neurological examination (performed by S.M. and L.J.B.B.), biochemical blood tests, and computed tomography or magnetic resonance angiography of the brain were performed in all patients at admission. The following imaging procedures were performed in order to detect possible stroke mechanisms: ultrasound examination of blood vessels of the neck (n=290), echocardiography (n=110), Holter electrocardiography (n=52), transcranial Doppler ultrasonography (n=200), and computed tomography or magnetic resonance angiography of blood vessels of the head and neck (n=110). Stroke severity at baseline was assessed with the National Institutes of Health Stroke Scale (NIHSS).16 The degree of disability or dependence in activities of daily living in stroke victims was assessed during the first 2 hours of admission with the modified Rankin Scale.17 The decreased level of consciousness was assessed on the Glasgow Coma Scale (score <15).16
Each stroke was classified into subtype groups based on etiopathogenetic mechanisms using TOAST criteria. The TOAST classification denotes five subtypes of ischemic stroke: 1) LAA, 2) CE, 3) SAO, 4) stroke of other determined etiology (OC), and 5) stroke of undetermined etiology (UND).8
We investigated whether patients had received early physical therapy during admission, which was defined as the initiation of kinesitherapy or early mobilization within 24 hours after admission. In-hospital medical complications defined as nonneurologic complications requiring intervention during the hospitalization were also documented.18 The treatment variables were excluded from the analysis since only eight patients (2.7%) received tissue plasminogen activator during the enrollment phase of the study.
Data on the course and outcome of stroke were obtained directly from patients and their families and physicians (by phone, by mail, or during their regular checkups) at 28 days and 1 year after stroke onset. For deceased patients, the medical records (in cases where the death occurred in hospital) or other relevant documentation associated with the fatal outcome were reviewed. In cases when patients were unavailable, general practitioners in public health centers were contacted and asked for additional information.
The study was approved by the Ethics Committee of the Faculty of Medicine, University of Belgrade.
Survival analysis was performed in the total stroke cohort and patient subgroups according to the TOAST classification. The Kaplan-Meier method was used to estimate the cumulative 28-day and 1-year survival rates. We defined the stroke onset as time zero and death as the end point. The log-rank test was used to assess differences in survival according to the different categories of variables.
The predictive value of different variables for the 28-day and 1-year survival rates was assessed using the univariate Cox proportional-hazards regression model. Since prognostic factors are often interrelated, the Cox proportional-hazards model was also used in a multivariate analysis. The factors that contributed to the outcome in the univariate analyses at p≤0.05 were included in the multivariate model. The associations are presented as hazard ratios with their corresponding 95% confidence intervals. At the 1-year follow-up, data were analyzed only for 28-day survivors in order to explore potential different contributions of prognostic factors to 28-day and 1-year survival rates.
In total, 300 first-ever acute ischemic stroke patients were included in the study. They were aged 71.3±9.8 years (mean±SD) and there were slightly more males (50.7%) than females (49.3%). The baseline characteristics of the study population are given in Table 1. The following complications occurred during hospitalization: 53 urinary tract infections (17.7%), 29 chest infections (15 pneumonia and 14 acute bronchitis) (9.7%), 3 pulmonary edemas (1.0%), 5 cases of sepsis (1.7%), 7 pressure sores (2.3%), and 14 deep venous thromboses (4.7%). Among 253 patients with a medical history of hypertension, 104 (34.7%) did not have adequate control of blood pressure (≥140/90 mm Hg) due to not receiving medication, missing medication doses, or taking medication only occasionally.
Complete survival data during the 1-year follow-up period were available for 97.7% of the patients.
Fifty-seven (19%) patients died during the 28-day period after stroke. Between 28 days and 1 year after stroke, we determined the outcome for 236 patients (7 patients lost during follow-up). Fifty-two of the 236 survivors at 28 days (22%) did not survive to 1 year after the stroke. The cumulative 28-day and 1-year survival rates for ischemic stroke patients in the cohort were 81.0±2.3% and 78.3±2.7%, respectively. During the 1-year follow-up, 109 patients died due to following causes: 65 index fatal ischemic strokes (59.6%), 19 recurrent fatal ischemic strokes (17.4%), 14 cardiovascular events (12.8%), 9 of other determined causes (8.4%), and 2 of undetermined causes (1.8%).
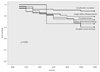
Cumulative 28-day and 1-year survival rates among the different subtypes of ischemic stroke according to TOAST classification are presented in Figs. 1 and 2. The cumulative 28-day survival rate (Fig. 1) was highest in patients with SAO (94.1±2.9%), followed by those with LAA (88.1±3.1%), UND (69.0±7.1%), and CE (65.4±5.4%) (p=0.001). The difference in 1-year survival among TOAST subtypes (Fig. 2) did not reach statistical significance (p=0.058): 88.9±4.0% for SAO, 79.3±4.2% for LAA, 73.5±6.3% for CE, and 60.7±9.2% for UND. Since there were only three patients in the OC subgroup, they were excluded from the further analysis.
The results of univariate Cox proportional-hazards analyses of predictors for 28-day and 1-year mortality rates are presented in Table 2 and 3. All baseline characteristics of patients were included in the analyses, but the tables list only the significant ones.
Variables identified as significant predictors of 28-day mortality in the initial univariate analysis and the multivariate model are listed in Table 2. The multivariate predictive model revealed that hypertension (p=0.017), NIHSS score ≥11 (p=0.001), and in-hospital medical complications (p=0.029) were significant unfavorable independent outcome predictors, while early physical therapy (p=0.001) was a significant favorable prognostic factor for 28-day mortality in our first-ever ischemic stroke patients.
Significant predictors of 1-year mortality are listed in Table 3. In the final multivariate model, age (p=0.001), NIHSS score ≥11 (p=0.001), and in-hospital complications (p=0.008) remained significant predictors of 1-year mortality in our cohort.
This is the first study analyzing short- and long-term mortality rates after first-ever acute ischemic stroke in Serbia. The results demonstrate that patients are at the highest risk of death during the first 28 days after stroke, which has also been reported previously.10-13 Furthermore, the 28-day CFR of 19% in our study is higher than that found in other cohort studies.12,18 The 28-day CFR is regarded as a quality marker of the effectiveness of stroke management. However, it should be noted that CFR may differ with demographic and risk-factor profiles that change the distribution of ischemic stroke subtypes and thus also the stroke severity and risk of death.6 The contribution of economic and social factors to stroke CFR in Serbia which limit access to effective treatment and stroke prevention2 cannot be excluded. Additionally, the long-term survival rates in our study are also lower than those reported previously.11,13,19
Most patients included in this study had hemiparesis and a high NIHSS score at admission, which may be associated with higher mortality during a long-term follow-up. Delayed recognition of stroke onset was also related to low survival rates in this population. Similarly to some other countries,20 delays in acute stroke management have been identified at different levels in Serbia: at the population level, due to a failure to recognize the symptoms of stroke; at the level of the emergency services, due to a failure to prioritize transportation of stroke patients; and at the hospital level, due to delays in neuroimaging and inefficient in-hospital care. Studies that identify demographic, social, cultural, behavioral, and clinical factors associated with a longer prehospital time may provide targets for population-based educational campaigns.20
It is well known that the etiology of acute ischemic stroke significantly influences its management, prognosis, and risk of recurrence.7 The distribution of ischemic stroke subtypes according to the TOAST classification based on etiopathogenetic mechanisms in our study population indicated that the most frequent was LAA, followed by CE, SAO, UND, and OC, in proportions that are comparable to those in a French stroke population.21 We found that the 28-day survival rate differed significantly with the stroke subtype (p=0.001), with it being highest in SAO and lowest in CE. Previously published studies also identified patients presenting with stroke due to CE as a particularly high-risk group, especially relative to patients with SAO.15,22 Identifying patients with high-risk stroke subtypes allows more accurate determination of the appropriate treatment and preventive strategies. However, the 1-year survival rate did not differ with the TOAST subtype in our study (p=0.058).
The multivariate Cox proportional-hazards models confirmed that severity of stroke and in-hospital complications were ordinary independent predictors of both 28-day and 1-year mortality rates in our study. Additional independent prognostic factors for short-term mortality were hypertension and early physical therapy, while being older was an independent prognostic factor for long-term mortality.
An almost universal finding is that stroke severity is the leading determinant of death in the early post-stroke phase and remains important for long-term survival.6,11,12 Our results provide further support for this notion.
The overall frequency of in-hospital medical complications in this study was 37.0%. This rate is higher than that found in the study of Bae et al.,18 which also only considered nonneurologic medical complications. In some other studies23,24 the percentage of complications exceeded 40%, although this higher rate may be attributed to those studies including both neurologic and nonneurologic complications. Bae et al.18 found that the difference in mortality between patients with and without in-hospital complications was statistically significant even among those surviving more than 3 years. Several mechanisms have been proposed to explain why medical complications that occur during hospitalization affect patient mortality far beyond the acute stage: 1) such complications may aggravate the original neuronal impairment, affect overall health, and reduce the potential for recovery; 2) they may delay or prevent rehabilitation and its beneficial effect on survival and recovery; 3) they could increase stroke comorbidity and thereby have a negative impact on outcome; and 4) in-hospital complications may indicate an increased risk of their recurrence after discharge and thus increase the probability of a poor outcome.18,23,24
Previous reports on the influence of hypertension on stroke mortality have been inconsistent.6,9,25 More than 80% of our patients had a diagnosis of hypertension, and the control of hypertension was inadequate in around one-third of them (34.7%). Discrepancies in risk-factor control may explain why most recent studies have not found hypertension to be predictive, contrary to the results of our study.
In our study, early physical therapy with mobilization as its fundamental component was a favorable prognostic factor for short-term mortality, as also demonstrated in other studies.26 Besides the early initiation of physical treatment being a key element of stroke-unit care, there is a lack of consensus on the definition of early physical therapy27; we consider early physical therapy (kinesitherapy and mobilization) to be that initiated within 24 hours of admission in hospital.
In the present study, being at least 71 years old was a significant predictor of mortality, which is in agreement with the results of some previous studies.9,12,25 Old age was found to be associated with strokes of greater severity, a higher frequency of atrial fibrillation, pre-existing disability, and residence in nursing homes.28 In Belgrade, public nursing home residents are mostly elderly people with social and medical problems that require continuous medical care.
A possible explanation for the discrepancy between short-term and long-term prognoses is that most of the above-mentioned short-term prognostic factors could be modified through intensive secondary prevention that would then reduce their negative impact on long-term mortality.
The present study was subject to several limitations. Its hospital-based design may limit the generalizability of our results, although in Belgrade almost all acute stroke patients are admitted to the two hospitals where the survey was performed. We did not include patients who died before admission to the hospitals, did not have an adequate diagnosis, and did not have the opportunity to receive treatment. Furthermore, other potentially significant factors including treatment variables or adherence to medication after discharge were not included in the analysis. Although survival data were available for 97.7% of the patients, the 1-year follow-up time may be too short for the manifestation of certain influencing factors.
In conclusion, our study was performed to gain more insight into the factors that predict mortality following a first-ever ischemic stroke in the population of Belgrade and to identify possible treatable factors. The findings indicate that improving short-term and long-term prognoses after an ischemic stroke requires 1) optimal control of vascular risk factors, 2) careful treatment of atherosclerotic vascular disease, and 3) appropriate interventions to prevent and manage in-hospital complications.
Figures and Tables
Fig. 1
Survival probabilities for ischemic stroke patients at 28 days according to TOAST classification. TOAST: Trial of Org 10172 in Acute Stroke Treatment.
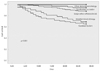
Fig. 2
Survival probabilities for ischemic stroke patients at 1 year according to TOAST classification. TOAST: Trial of Org 10172 in Acute Stroke Treatment.
Acknowledgements
This investigation was supported by the Ministry of Education and Science of the Republic of Serbia (Grant No 175087).
References
1. Pekmezovic T, Vlajinac H, Sipetic-Grujicic S, Kocev N, Tepavcevic DK, Bumbasirevic LB. Preedy VR, Watson RR, editors. Burden of cerebrovascular diseases (stroke) in Serbia. Handbook of Disease Burdens and Quality of Life Measures. 2010. New York: Springer;950–964.

2. Pekmezovic T, Tepavcevic DK, Jarebinski M, Kostic M, Bumbasirevic L. Stroke mortality in Belgrade, Serbia: age, period, and cohort analyses. Cerebrovasc Dis. 2007. 24:191–195.
3. Pekmezovic T, Tepavcevic DK, Jarebinski M, Kostic M, Bumbasirevic L. Trends in mortality from different subtypes of stroke in the population of Belgrade (Serbia). Clin Neurol Neurosurg. 2008. 110:51–57.

4. Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009. 8:345–354.

5. Endres M, Heuschmann PU, Laufs U, Hakim AM. Primary prevention of stroke: blood pressure, lipids, and heart failure. Eur Heart J. 2011. 32:545–552.

6. Olsen TS. Fisher M, editor. Stroke recurrence and prognosis after stroke. Handbook of Clinical Neurology. 2009. 92. New York: Elsevier;406–421.
7. Kolominsky-Rabas PL, Weber M, Gefeller O, Neundoerfer B, Heuschmann PU. Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke. 2001. 32:2735–2740.

8. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993. 24:35–41.

9. Counsell C, Dennis M. Systematic review of prognostic models in patients with acute stroke. Cerebrovasc Dis. 2001. 12:159–170.

10. Hakkennes SJ, Brock K, Hill KD. Selection for inpatient rehabilitation after acute stroke: a systematic review of the literature. Arch Phys Med Rehabil. 2011. 92:2057–2070.

11. Koton S, Tanne D, Green MS, Bornstein NM. Mortality and predictors of death 1 month and 3 years after first-ever ischemic stroke: data from the first national acute stroke Israeli survey (NASIS 2004). Neuroepidemiology. 2010. 34:90–96.

12. Saposnik G, Hill MD, O'Donnell M, Fang J, Hachinski V, Kapral MK, et al. Variables associated with 7-day, 30-day, and 1-year fatality after ischemic stroke. Stroke. 2008. 39:2318–2324.

13. Andersen KK, Andersen ZJ, Olsen TS. Predictors of early and late case-fatality in a nationwide Danish study of 26,818 patients with first-ever ischemic stroke. Stroke. 2011. 42:2806–2812.

14. Appelros P, Nydevik I, Viitanen M. Poor outcome after first-ever stroke: predictors for death, dependency, and recurrent stroke within the first year. Stroke. 2003. 34:122–126.
15. Vemmos KN, Bots ML, Tsibouris PK, Zis VP, Takis CE, Grobbee DE, et al. Prognosis of stroke in the south of Greece: 1 year mortality, functional outcome and its determinants: the Arcadia Stroke Registry. J Neurol Neurosurg Psychiatry. 2000. 69:595–600.

16. Goldstein LB, Bertels C, Davis JN. Interrater reliability of the NIH stroke scale. Arch Neurol. 1989. 46:660–662.

17. van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988. 19:604–607.

18. Bae HJ, Yoon DS, Lee J, Kim BK, Koo JS, Kwon O, et al. In-hospital medical complications and long-term mortality after ischemic stroke. Stroke. 2005. 36:2441–2445.

19. Katzenellenbogen JM, Vos T, Somerford P, Begg S, Semmens JB, Codde JP. Excess mortality rates for estimating the non-fatal burden of stroke in Western Australia: a data linkage study. Cerebrovasc Dis. 2010. 30:57–64.

20. Kwan J, Hand P, Sandercock P. A systematic review of barriers to delivery of thrombolysis for acute stroke. Age Ageing. 2004. 33:116–121.

21. Bejot Y, Caillier M, Ben Salem D, Couvreur G, Rouaud O, Osseby GV, et al. Ischaemic stroke subtypes and associated risk factors: a French population based study. J Neurol Neurosurg Psychiatry. 2008. 79:1344–1348.

22. Stead LG, Gilmore RM, Bellolio MF, Jain A, Rabinstein AA, Decker WW, et al. Cardioembolic but not other stroke subtypes predict mortality independent of stroke severity at presentation. Stroke Res Treat. 2011. 2011:281496.

23. Kumar S, Selim MH, Caplan LR. Medical complications after stroke. Lancet Neurol. 2010. 9:105–118.

24. Langhorne P, Stott DJ, Robertson L, MacDonald J, Jones L, McAlpine C, et al. Medical complications after stroke: a multicenter study. Stroke. 2000. 31:1223–1229.
25. Appelros P, Nydevik I, Seiger A, Terént A. Predictors of severe stroke: influence of preexisting dementia and cardiac disorders. Stroke. 2002. 33:2357–2362.
26. Diserens K, Michel P, Bogousslavsky J. Early mobilisation after stroke: Review of the literature. Cerebrovasc Dis. 2006. 22:183–190.

27. Quinn TJ, Paolucci S, Sunnerhagen KS, Sivenius J, Walker MF, Toni D, et al. Evidence-based stroke rehabilitation: an expanded guidance document from the European stroke organization (ESO) guidelines for management of ischaemic stroke and transient ischaemic attack 2008. J Rehabil Med. 2009. 41:99–111.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download