Abstract
Background and Purpose
Treatment with atorvastatin (80 mg) in stroke secondary prevention for patients with prior intracranial hemorrhage (ICH) has been associated with a higher frequency of ICH. The aim of this study was to determine whether 20 mg/day atorvastatin is linked to stroke recurrence in Chinese ischemic stroke patients with prior ICH.
Methods
A single-center retrospective cohort study was conducted, involving 354 cases from 395 Chinese in-patients who had ischemic stroke with prior ICH history in Beijing Chaoyang hospital from May 1, 2005 to October 31, 2010. Survivors were followed by telephone interviews for 12-60 months. Cox regression and Kaplan-Meier plot analysis were used to evaluate the effect of 20 mg/day atorvastatin on cerebral infarction and ICH recurrence.
Results
The overall rate of stroke recurrence was lower in the 20 mg/day atorvastatin group (χ2=6.687, p=0.022) than in the control group. The incidence of cerebral hemorrhage was increased by 20 mg/day atorvastatin for ischemic stroke cases with a history of ICH compared to those not receiving the drug, but the difference was not significant [hazard ratio (HR)=1.097, 95% confidence interval (CI)=0.800-1.243, p=0.980]. The incidence of ischemic stroke recurrence was significantly reduced in subjects receiving atorvastatin (HR=0.723, 95% CI=0.578-0.862, p=0.028), and the mean duration of all stroke recurrences was significantly prolonged, compared with those not exposed to the drug (χ2=5.351, p=0.021). The mean duration of ICH recurrence appeared to have shortened with atorvastatin, but the difference was not significant (χ2=0.680, p=0.480), and the mean duration of cerebral infarction recurrence was significantly prolonged (χ2=8.312, p=0.004).
The Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial1 found that stroke outcome was affected in patients randomized to receive atorvastatin (80 mg), and that increasing incidences of intracranial hemorrhage (ICH) were attributable mainly to the patients' history of ICH, which resulted in some of the patients refusing statin therapy. The possibility that a lower dose of atorvastatin (20 mg/day) reduces the likelihood of cerebral infarction recurrence, and thus alleviates the fear of ICH recurrence among Chinese patients with ischemic stroke and a history of ICH, has yet to be examined. We investigated two hypotheses: 1) patients with ischemic stroke and a history of ICH taking 20 mg/day atorvastatin are less likely to suffer a recurrence of ischemic stroke, 2) and the rate of ICH recurrence does not differ between patients who do and do not take atorvastatin.
The hospital records of 395 Chinese ischemic stroke patients with a history of ICH at Beijing Chaoyang hospital between May 1, 2005 and October 31, 2010 were studied. The clinical condition (pertaining to stroke and ICH) of all of the subjects was validated by cranial computed tomography (CT) or magnetic resonance imaging (MRI). The hospital's institutional review board approved the study and all subjects gave their informed consent to participate. All of the patients were followed up for a mean period of 38 months. They were aged between 41 and 80 years, had been diagnosed with ischemic stroke, and had a history of ICH. Patients with hemorrhage attributable to trauma, tumor, aneurysm, vascular malformation, or hemorrhagic conversion of arterial or venous infarction were excluded. Of the 395 patients, 41 cases were found to be ineligible for the study: 15 cases had cerebral hemorrhage secondary to cerebral vascular malformations and aneurysms, 7 cases had ischemic stroke secondary to hereditary diseases and vascular malformations, and 19 cases denied access to their clinical details. Ultimately, 354 patients or caregivers were interviewed by telephone, of whom 13 were lost to follow-up due to death (6 due to ischemic stroke recurrence, 2 due to hemorrhagic stroke recurrence, and 5 due to other diseases). The author performed the data collection during the follow-up period.
The following data were collected: blood pressure, heart rate and rhythm, body temperature, serum glucose level, brain imaging characteristics, and details of other accompanying risk factors [hypertension, diabetes, smoking, myocardial infarction (MI) and carotid angioplasty, atrial fibrillation (AF) and coronary heart disease, history of smoking and alcohol intake, management of the risk factors, family history, and locations of previous ICH(s)]. All of the following characteristics were also recorded: medication use (including atorvastatin use), duration of 20 mg/day atorvastatin administration (some of the patients refused to take it, mostly because they were concerned about the possibility of an increased risk of ICH recurrence), recurrent stroke, death, and readmission. Recurrent ICH and cerebral infarction were confirmed by cranial CT or MRI. ICH could be divided into lobar hemorrhage and infralobar hemorrhage by location based on the initial imaging reports: lobar hemorrhage included hemorrhage of the cerebral lobes and white matter below the lobes, while infralobar hemorrhage included hemorrhage of the basal ganglia, brainstem, and cerebellum.2
All statistical analyses were performed using SPSS version 17.0 (SPSS, Chicago, IL, USA). The level of statistical significance in the final model was set at p<0.05. Pearson's chi-square two-tailed test was performed to analyze the general categorical variables, while the unpaired t-test was applied to analyze continuous variables. We used Kaplan-Meier plots with significance testing by the log-rank test to determine univariate predictors of exposure to 20 mg/day atorvastatin and stroke recurrence. The independent contribution of each risk factor to ischemic stroke outcomes was estimated using a Cox proportional-hazards regression model. The forward LR method was applied. Clinical covariates with a univariate probability value of 0.05 were entered into the Cox proportional-hazards regression model to adjust for potential confounders.
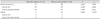
Overall, 161 patients received 20 mg/day atorvastatin. Recurrent stroke occurred during a median follow-up period of 38 months in 47 of the subjects taking atorvastatin (23 for recurrent ICH) and 88 of the control group (29 for recurrent ICH). Sixty-nine subjects were treated with 20 mg/day atorvastatin without delay after ischemic stroke, and the remaining 92 began taking 20 mg/day atorvastatin at a later date (at a median of 1.6 months after the ischemic stroke). The baseline data of the two groups are presented in Table 1.
At the endpoint, stroke recurrence was less prevalent in the 20 mg/day statin group than in the control group (χ2=6.687, p=0.022) (Table 2). Although the incidence of cerebral hemorrhage was slightly increased with 20 mg/day atorvastatin therapy for the secondary prevention of ischemic stroke in patients with a history of ICH, the difference was not statistically significant [hazard ratio (HR)=1.097, 95% confidence interval (CI)=0.800-1.243, p=0.980]. Poorly controlled high blood pressure and lobar hemorrhage were risk factors for ICH recurrence (Table 3). The incidence of ischemic stroke recurrence was significantly reduced with the use of 20 mg/day atorvastatin (HR=0.723, 95% CI=0.678-0.862, p=0.028).
The mean durations of all stroke recurrences for ischemic stroke patients with a history of ICH were 19.8 and 15.5 months for those treated and not treated with atorvastatin, respectively (χ2=5.351, p=0.021), as shown in Fig. 1. The mean durations of cerebral infarction recurrence were 21.4 and 14.7 months with and without atorvastatin, respectively (χ2=8.312, p=0.004), as shown in Fig. 2. Five out of the ten patients who died of cerebral infarction recurrence had received 20 mg/day atorvastatin (Table 2), but there was no significant difference in mortality between the with- and without-atorvastatin groups (χ2=0.208, p=0.649). The mean durations of cerebral hemorrhage recurrence were 16.6 and 17.5 months among those receiving and not receiving atorvastatin, respectively. Although the duration of ICH recurrence appeared to have been reduced by 20 mg/day atorvastatin therapy (Fig. 3), the difference was not statistically significant (χ2=0.680, p=0.480). Six of the 11 patients who died of cerebral hemorrhage recurrence had been treated with 20 mg/day atorvastatin (Table 2); the mortality rate did not differ significantly between the two groups (χ2=0.680, p=0.410).
A randomized trial in persons with stroke showed that 80 mg of atorvastatin per day dramatically reduced stroke recurrence while simultaneously increasing the risk of ICH,1 especially in those with a history of ICH. However, the use of 20 mg/day atorvastatin to prevent secondary stroke in Chinese ischemic stroke patients with a history of ICH history yielded a trend favoring a reduction in stroke recurrence. Experts in Japan3 found that this dose of statins reduced the risk of coronary heart disease in Japan to the same degree as higher doses did in both Europe and the USA. This difference may be attributable to race and dietary habits.
The findings of the present study suggest that lobar hemorrhage recurrence was more common than recurrent infralobar hemorrhage. The reason for this is unclear, but a possible explanation is different pathogeneses of lobar and infralobar cerebral hemorrhage. It was demonstrated in neuropathology studies that lobar cerebral hemorrhage was closely related to amyloid vascular degeneration.4-7 The data revealed that patients with a history of MI and AF were more likely to take the daily 20 mg dose of atorvastatin agents than were other patients. This may be because their cardiologists paid more attention to the incidence of ischemia recurrence after stenting, despite the higher rates of ICH recurrence with statin agents.8,9 This could also explain the trend toward a reduction in recurrent cerebral infarction in patients with MI and AF, which may be related to the administration of 20 mg/day statins.
Observational clinical studies also provide data reflecting the potential impact of statins on ischemic stroke recurrence, although the results have been inconsistent. Most of these studies found that statins taken before the index stroke had no clear impact on ICH stroke recurrence.10-12 One study found that statins were associated with a lower rate of recurrent stroke in White but not Black patients,13 demonstrating that their effects vary with race. However, few studies have assessed Chinese populations, and the type and dose of statins administered varied between them. All of our patients took 20 mg/day atorvastatin, and a significant effect of this treatment on stroke recurrence was observed, although this study was constrained by its retrospective design.
The aim of this analysis was primarily to assess the potential protective effect of 20 mg/day atorvastatin therapy against the recurrence of ischemic events and hemorrhagic stroke. It was previously shown that prior statin use was associated with a higher risk of ICH recurrence in a series of patients with nontraumatic intracerebral hemorrhage.14 Analysis of SPARCL data revealed that statin treatment was associated with an increased risk of hemorrhagic stroke in subjects with prior stroke that was independent of other factors.1,15 Although limited by the small cohort the received 20 mg/day atorvastatin, a retrospective analysis of 629 consecutive patients from a single-center longitudinal cohort study of primary intracerebral hemorrhage found no effect of prior statin use on ICH recurrence.16 We also found that the overall benefit of atorvastatin on all stroke recurrence rates was maintained if the analysis was carried out for all events.
As we noted, statin treatment reduced the recurrence of ischemic stroke. To control for the possibility of confounding by indication, we also used a Cox regression model to adjust for other characteristics associated with exposure to 20 mg/day atorvastatin for ischemic stroke recurrence. The effect is likely to be associated with its potent lipid-lowering properties. In addition, statin up-regulates the synthesis of endothelial nitric oxide, thereby increasing cerebral blood flow,17-20 and users of statins have more extensive arterial collaterals than nonusers.21 More extensive arterial collaterals might also be beneficial in reducing ischemic stroke recurrence.
The present retrospective study had some potential limitations. The study population was small and selection bias was inevitable, in common with previous studies of patients with ICH.7 For example, physicians might avoid the use of statins in subjects perceived to be at higher risk of recurrence, which could lead to an underestimation of the risk associated with these agents. Furthermore, some of the patients refused consent to participate during the follow-up period. However, the baseline characteristics of these data were consistent with those of a randomized control group.2 Therefore, the probability of selection bias was minimal.
Our results have potential implications for the treatment of ICH survivors who are also at risk of recurrent ischemic diseases. They suggest that 20 mg/day atorvastatin can be used in ICH survivors without substantially increasing the risk of recurrent ICH. However, its use at this dose for the secondary prevention of patients with ICH history needs to be verified by further prospective randomized double-blind controlled trials.
Figures and Tables
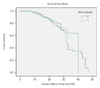 | Fig. 1Relationship between stroke recurrence and exposure to 20 mg/day atorvastatin in ischemic stroke patients with a history of intracranial hemorrhage (log-rank test; χ2=5.351, p=0.021). |
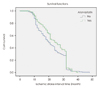 | Fig. 2Relationship between ischemic stroke recurrence and exposure to 20 mg/day atorvastatin in ischemic stroke patients with a history of intracranial hemorrhage (log-rank test; χ2=8.312, p=0.004). |
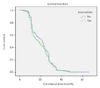 | Fig. 3Relationship between ICH recurrence and exposure to 20 mg/day atorvastatin in ischemic stroke patients with a history of lobar hemorrhage (log-rank test; χ2=0.680, p=0.480). ICH: intracranial hemorrhage. |
Table 1
Characteristics of the ischemic stroke patients with intracranial hemorrhage history treated (n=161) and not treated (n=193) with atorvastatin

Acknowledgements
This study was supported by funding from Wu Jieping Medical Foundation Special Assistance Fund to Clinical Research.
References
1. Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, Rudolph AE, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006; 355:549–559.

2. Morgenstern LB, Hemphill JC 3rd, Anderson C, Becker K, Broderick JP, Connolly ES Jr, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2010; 41:2108–2129.

3. Nakamura H, Arakawa K, Itakura H, Kitabatake A, Goto Y, Toyota T, et al. Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial. Lancet. 2006; 368:1155–1163.

4. Biffi A, Greenberg SM. Cerebral amyloid angiopathy: a systematic review. J Clin Neurol. 2011; 7:1–9.

5. Thoonsen H, Richard E, Bentham P, Gray R, van Geloven N, De Haan RJ, et al. Aspirin in Alzheimer's disease: increased risk of intracerebral hemorrhage: cause for concern? Stroke. 2010; 41:2690–2692.
6. Coutts SB, Hill MD, Simon JE, Sohn CH, Scott JN, Demchuk AM. VISION Study Group. Silent ischemia in minor stroke and TIA patients identified on MR imaging. Neurology. 2005; 65:513–517.

7. Kimberly WT, Gilson A, Rost NS, Rosand J, Viswanathan A, Smith EE, et al. Silent ischemic infarcts are associated with hemorrhage burden in cerebral amyloid angiopathy. Neurology. 2009; 72:1230–1235.

8. Jia W, Zhou L. Use of antiplatelets. A survey of secondary prevention of ischemic stroke with intracranial hemorrhage history in Chinese patients. Neurosciences (Riyadh). 2011; 16:335–339.
9. Weimar C, Benemann J, Terborg C, Walter U, Weber R, Diener HC. German Stroke Study Collaboration. Recurrent stroke after lobar and deep intracerebral hemorrhage: a hospital-based cohort study. Cerebrovasc Dis. 2011; 32:283–288.

10. Moonis M, Kane K, Schwiderski U, Sandage BW, Fisher M. HMGCoA reductase inhibitors improve acute ischemic stroke outcome. Stroke. 2005; 36:1298–1300.

11. Elkind MS, Flint AC, Sciacca RR, Sacco RL. Lipid-lowering agent use at ischemic stroke onset is associated with decreased mortality. Neurology. 2005; 65:253–258.

12. Bushnell CD, Griffin J, Newby LK, Goldstein LB, Mahaffey KW, Graffagnino CA, et al. Statin use and sex-specific stroke outcomes in patients with vascular disease. Stroke. 2006; 37:1427–1431.

13. Reeves MJ, Gargano JW, Luo Z, Mullard AJ, Jacobs BS, Majid A. Paul Coverdell National Acute Stroke Registry Michigan Prototype Investigators. Effect of pretreatment with statins on ischemic stroke outcomes. Stroke. 2008; 39:1779–1785.

14. Rocco A, Sykora M, Ringleb P, Diedler J. Impact of statin use and lipid profile on symptomatic intracerebral haemorrhage, outcome and mortality after intravenous thrombolysis in acute stroke. Cerebrovasc Dis. 2012; 33:362–368.

15. Goldstein LB, Amarenco P, Szarek M, Callahan A 3rd, Hennerici M, Sillesen H, et al. Hemorrhagic stroke in the Stroke Prevention by Aggressive Reduction in Cholesterol Levels study. Neurology. 2008; 70(24 Pt 2):2364–2370.

16. FitzMaurice E, Wendell L, Snider R, Schwab K, Chanderraj R, Kinnecom C, et al. Effect of statins on intracerebral hemorrhage outcome and recurrence. Stroke. 2008; 39:2151–2154.

17. Kawashima S, Yamashita T, Miwa Y, Ozaki M, Namiki M, Hirase T, et al. HMG-CoA reductase inhibitor has protective effects against stroke events in stroke-prone spontaneously hypertensive rats. Stroke. 2003; 34:157–163.

18. Ortego M, Bustos C, Hernández-Presa MA, Tuñón J, Díaz C, Hernández G, et al. Atorvastatin reduces NF-kappaB activation and chemokine expression in vascular smooth muscle cells and mononuclear cells. Atherosclerosis. 1999; 147:253–261.

19. Endres M, Laufs U, Huang Z, Nakamura T, Huang P, Moskowitz MA, et al. Stroke protection by 3-hydroxy-3-methylglutaryl (HMG)-CoA reductase inhibitors mediated by endothelial nitric oxide synthase. Proc Natl Acad Sci U S A. 1998; 95:8880–8885.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download