Abstract
Background
Pathological gambling (PG), which is characterized by consistent, repetitive gambling and unsuccessful quitting attempts, is classified as an impulse control disorder. PG has also been reported in patients with Parkinson's disease, frontotemporal dementia, and amyotrophic lateral sclerosis.
Pathological gambling (PG) is characterized by consistent and repetitive gambling, losing large amounts of money, unsuccessful quitting attempts, attending illegal gambling sessions, lying, and relying on support from other people to obtain money, with disruptive consequences on familial, occupational, and social functions.1 PG was defined by Kraepelin as "gambling mania" a hundred years ago,2 and in current diagnostic systems it is classified into the category of "impulse-control disorders not otherwise classified".1 The lifetime prevalence of PG is 1-3% in the general population and it is frequently comorbid with other psychiatric disorders such as affective disorders (e.g., depression and hypomania), substance-use disorders, attention deficit and hyperactivity disorder, and personality disorders.3,4
PG, which was associated with frontal lobe dysfunction,5 has also been reported in disorders such as frontotemporal dementia (FTD) and Parkinson's disease (PD). The lifetime prevalence of PG in PD was reported as 3.4%, and 7.2% in patients on any dopamine agonist.6 Three cases of frontal variant FTD with PG have been reported,7-9 but there is no case report of FTD-amyotrophic lateral sclerosis (ALS) with PG in the literature. Moreover, other disinhibition behaviors reflecting prefrontal dysfunction have been reported in patients with ALS. For example, pathological laughing and crying are frequent in ALS patients, with these symptoms being associated with executive dysfunction as indicated by a greater number of total errors in the Wisconsin Card-Sorting Test (WCST).10 Wicks and MacPhee investigated the prevalence of PG using a Web-based community survey and found that 13% of PD patients (n=208) and 3% of ALS patients (n=236) were classified as "problem gamblers."11 However, these data are entirely based on subjective survey reports, and referred cases might not be diagnosed as "pathological gamblers."
ALS is not a pure motor neuron disease, since there is growing evidence that the cognitive impairments range from mild cognitive (especially executive) dysfunction to dementia. It is suggested that ALS and FTD represent a continuum between motor and nonmotor cortical degeneration.12 Recent studies have shown that ALS patients without FTD also present changes in behavior, personality, and cognition,12,13 and that these changes can appear before, after, or at the onset of the ALS symptoms.13 However, the exact clinical relationship between FTD and ALS is still unknown.
This paper presents a FTD-ALS case presenting with PG.
A 53-year-old male retired government employee with a highest education level of graduation from primary school was admitted to the psychiatric outpatient clinic due to excessive gambling, personality changes (lying, selfishness, and not caring for family members), and large financial debts to both other individuals and several banks in October 2007. He had retired 5 years previously, since when he had spent most of his time betting on horse racing. He had gradually become moody, nervous, and childish, and exhibited verbally and physically aggressive behavior toward his wife. He did not care about his personal hygiene. He was first referred to our clinic in May 2007, with symptoms of irritability, anger, and washing his hands frequently. He did not report his gambling behaviors and he was diagnosed as "anxiety disorder, not otherwise specified". He initially received citalopram (40 mg/day), to which olanzapine (2.5 mg/day) was later added. The patient was concurrently admitted to the neurology outpatient clinic due to difficulty in walking resulting from muscle cramps and weakness in his legs. His neurological symptoms had been present for approximately 1 year. He had a nasal voice, bilateral distal upper limb paresis (Grade IV), bilateral positive Hoffmann and Babinski reflexes, and bilaterally increased deep tendon reflexes (both in upper and lower limbs) in a neurological examination. The electromyogram (EMG) revealed normal neuronal conduction, but in needle EMGs there were frequent fasciculations, fibrillations, and high-amplitude polyphasic motor-unit potentials in the upper and lower extremities (biceps, triceps, I.dorsal interosseous, abductor pollicis brevis, vastus medialis, tibialis anterior muscles, and bilateral) and the thoracic paraspinal muscles (T-5, -8, and -10 paraspinals). These findings were considered compatible with the common motor neuron involvement. The results of blood and urine tests were normal, so the case was diagnosed with "clinically probable-laboratory supported ALS" according to the El Escorial Criteria for the Diagnosis of ALS.14
His medical history and his family history were not significant.
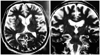
A mental status examination performed in October 2007 was characterized by apathy, irritability, decreased amount of speech, inappropriate affect, and psychomotor retardation. A neurological examination revealed nasal voice, bilaterally decreased gag reflex, increased deep tendon reflexes, bilaterally positive Hoffmann, palmomental, Babinski, and glabellar reflexes, postural instability, and a positive Romberg test. A detailed neuropsychological assessment was performed using the Standardized Mini Mental Test, Clock Drawing Test (CDT), Frontal Assessment Battery (FAB), Alzheimer Disease Assessment Scale-cognitive (ADAS-COG), Trail-Making Test A (TMT-A) and B (TMT-B), WCST, Wechsler Adult Intelligence Test-Revised Form (WAIS-R), and Iowa Gambling Task (IGT).15-23 The scores in the neuropsychological tests are presented in Table 1. He had severe deficiency in frontal lobe functions such as judgement, decision making, planning, concept formation, attention, similarities, verbal fluency (as assessed on the subscales of the WAIS-R, FAB, TMT-A/B, WCST, IGT, and CDT), and mild deficiency in temporal lobe functions such as verbal recall and recognition (as assessed on ADAS-COG subscales). These results were indicative of severe dysfunction of frontal brain regions and mild dysfunction of temporal brain regions. Cranial MRI revealed frontotemporal atrophy with several ischemic gliotic lesions in the posterior periventricular and subcortical white matter. T2-weighted coronal and horizontal MRI images of the patient are shown in Fig. 1.
The case was diagnosed as FTD with ALS. Citalopram and olanzapine were stopped during follow-up since they were not providing any benefit, and were replaced by paroxetine (30 mg/day) for PG and other disinhibition behaviors, and by riluzole (100 mg/day) and baclofen (30 mg/day) for ALS. His inappropriate affect and irritability decreased and he stopped gambling. However, his fasciculations (both in upper and lower limbs), weakness (in lower limbs), and difficulties in walking and talking worsened within 2 years. At his last visit in November 2010 he could not walk without assistance and his score on the ALS Functional Rating Scale24 was 29 out of 40.
FTD is characterized by profound character change, altered social conduct, and executive deficits reflecting a focal degeneration of the frontal and temporal neocortices. According to the consensus criteria suggested by Neary et al.25 FTD is characterized by insidious onset, gradual progression, early decline in social interpersonal contact, early emotional blunting, and early loss of insight. Supportive diagnostic features include a decline in personal hygiene, mental rigidity, distractibility, aspontaneity, and decreased amount of speech. The presence of apathy, inappropriate affect, changes in personality, and decreased amount of speech in the present case support the frontal/behavioral variant of FTD. Neuropsychological test performances also supported frontotemporal dysfunction. The syndrome of FTD-ALS is considered important since it has the potential to shed light on the pathophysiology of FTD, which is a highly heterogeneous disorder.12 More than half of ALS patients exhibit some behavioral or cognitive symptoms,7,8 but not all such patients meet the diagnostic criteria for FTD. Ten percent of ALS patients reportedly have FTD. Some of the patients with classical ALS develop FTD before, after, or at the onset of ALS, while others may present with mild cognitive dysfunction and behavioral changes rather than a fully developed dementia syndrome.26-29
FTD-ALS patients are usually overactive and disinhibited, which indicates the involvement of the orbitofrontal cortex (OFC).26 The OFC is also associated with decision-making processes, emotion-related learning, and representations of reward and punishment.30 OFC impairment can result in the inability to choose between alternatives regardless of their importance because emotional consequences are not differentiable, probably due to deficits in emotional learning.30 Various clinical symptoms, such as changes in personality, emotion, and social conduct, are known to reflect disruptions in either the OFC or the orbitofrontal circuitry.8,30 Cavedini et al.5 compared PG patients (n=20) and healthy controls (n=40) using the Gambling Task and other neuropsychological measures for frontal lobe dysfunction such as the WCST and Weigl's Sorting Test. They found no significant difference between PG patients and healthy controls in the WCST and Weigl's Sorting Test, but PG patients performed worse in the Gambling Task. These data are important since they suggest the presence of OFC dysfunction rather than a generalized frontal deficit in PG patients. In the present case, impulse control disorder presenting as PG may also have been associated with the involvement of the OFC. The initial symptoms of FTD also reflect the early involvement of OFC. Socially inappropriate behaviors such as abnormal sexuality, offensive speech, theft, and public urination or masturbation are common in FTD.
There are three similar cases of FTD presenting with PG in the literature.7-9 The first case was a 49-year-old male patient with disinhibited, overactive subtype of FTD whose initial symptom was PG.7 Nakaaki et al.8 reported a similar patient whose cognitive functions were fully preserved, except decision making as assessed by the IGT. The third case was reported by Manes et al.9 who also highlighted selective impairment in the IGT in a female FTD patient presenting with PG. The present case is the first of FTD-ALS presenting with PG.
Frontotemporal dysfunction, which presented as PG in the present case, may be a characteristic feature of FTD-ALS syndrome.8 It is suggested that some cases of classical ALS have preclinical FTD, such that the early emotional changes and behavioral signs are obscured by or difficult to disentangle from the physical sequelae of classical ALS. In other patients the spread and progression of pathological changes may be conjectured to be sufficient to give rise to deficits on tests of executive function.26 The executive functions were also impaired in the present case, but the IGT-which specifically measures decision making-seems to be a more sensitive tool for assessing orbitofrontal involvement in such patients.
PG and other behavioral disturbances in the present case responded to paroxetine, which is consistent with previous findings in FTD patients.31,32 Anneser et al.33 reported inappropriate sexual behavior in a FTD-ALS patient who was successfully treated with sertraline.
This case report underlines that PG, which is classified as an impulse control disorder in current psychiatric diagnostic systems, can also be seen in patients with neurological disorders involving the OFC. Therefore, neurological and neuropsychological assessments should be considered especially in late-onset PG patients with other behavioral and cognitive symptoms. Furthermore, a differential diagnosis is important in such patients, since PG itself does not diminish the legal responsibility for debt,34 whereas a comorbid FTD does.
Figures and Tables
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. 2000. 4th ed., text rev. Washington, D.C.: American Psychiatric Association.
2. Black DW, Moyer T. Clinical features and psychiatric comorbidity of subjects with pathological gambling behavior. Psychiatr Serv. 1998. 49:1434–1439.

3. Dell'Osso B, Altamura AC, Allen A, Marazziti D, Hollander E. Epidemiologic and clinical updates on impulse control disorders: a critical review. Eur Arch Psychiatry Clin Neurosci. 2006. 256:464–475.
4. Roy A, Adinoff B, Roehrich L, Lamparski D, Custer R, Lorenz V, et al. Pathological gambling. A psychobiological study. Arch Gen Psychiatry. 1988. 45:369–373.
5. Cavedini P, Riboldi G, Keller R, D'Annucci A, Bellodi L. Frontal lobe dysfunction in pathological gambling patients. Biol Psychiatry. 2002. 51:334–341.

6. Voon V, Hassan K, Zurowski M, Duff-Canning S, de Souza M, Fox S, et al. Prospective prevalence of pathologic gambling and medication association in Parkinson disease. Neurology. 2006. 66:1750–1752.

7. Lo Coco D, Nacci P. Frontotemporal dementia presenting with pathological gambling. J Neuropsychiatry Clin Neurosci. 2004. 16:117–118.

8. Nakaaki S, Murata Y, Sato J, Shinagawa Y, Hongo J, Tatsumi H, et al. Impairment of decision-making cognition in a case of frontotemporal lobar degeneration (FTLD) presenting with pathologic gambling and hoarding as the initial symptoms. Cogn Behav Neurol. 2007. 20:121–125.

9. Manes FF, Torralva T, Roca M, Gleichgerrcht E, Bekinschtein TA, Hodges JR. Frontotemporal dementia presenting as pathological gambling. Nat Rev Neurol. 2010. 6:347–352.

10. McCullagh S, Moore M, Gawel M, Feinstein A. Pathological laughing and crying in amyotrophic lateral sclerosis: an association with prefrontal cognitive dysfunction. J Neurol Sci. 1999. 169:43–48.

11. Wicks P, MacPhee GJ. Pathological gambling amongst Parkinson's disease and ALS patients in an online community (PatientsLikeMe.com). Mov Disord. 2009. 24:1085–1088.

12. Irwin D, Lippa CF, Swearer JM. Cognition and amyotrophic lateral sclerosis (ALS). Am J Alzheimers Dis Other Demen. 2007. 22:300–312.

13. Gibbons ZC, Richardson A, Neary D, Snowden JS. Behaviour in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2008. 9:67–74.

14. Brooks BR. Subcommittee on Motor Neuron Diseases/Amyotrophic Lateral Sclerosis of the World Federation of Neurology Research Group on Neuromuscular Diseases and the El Escorial "Clinical limits of amyotrophic lateral sclerosis" workshop contributors. El Escorial World Federation of Neurology criteria for the diagnosis of amyotrophic lateral sclerosis. J Neurol Sci. 1994. 124:Suppl. 96–107.

15. Güngen C, Ertan T, Eker E, Yaşar R, Engin F. Reliability and validity of the standardized Mini Mental State Examination in the diagnosis of mild dementia in Turkish population. Turk Psikiyatri Derg. 2002. 13:273–281.
16. Can SS, Özel Kızıl ET, Varlı M, Turan E, Atlı T. Psychometric properties of the Turkish versions of three different clock drawing tests in patients with dementia. Arch Neuropsychiatry. 2010. 47:91–95.
17. Dubois B, Slachevsky A, Litvan I, Pillon B. The FAB: a Frontal Assessment Battery at bedside. Neurology. 2000. 55:1621–1626.

18. Mavioglu H, Gedizlioglu M, Akyel S, Aslaner T, Eser E. The validity and reliability of the Turkish version of Alzheimer's Disease Assessment Scale-Cognitive Subscale (ADAS-Cog) in patients with mild and moderate Alzheimer's disease and normal subjects. Int J Geriatr Psychiatry. 2006. 21:259–265.

19. Cangöz B, Karakoç E, Selekler K. Trail Making Test: normative data for Turkish elderly population by age, sex and education. J Neurol Sci. 2009. 283:73–78.

20. Karakaş S. Handbook of BİLNOT Battery: Research and Development Studies for Neuropsychological Tests. 2006. 2nd ed. Ankara: Eryılmaz Ofset Matbaacılık Gazetecilik.
21. Wechsler D. WAIS-R Manual: Wechsler Adult Intelligence Scale-Revised. 1981. New York: Psychological Corporation.
22. Bechara A, Tranel D, Damasio H. Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain. 2000. 123:2189–2202.

23. Gregory C, Lough S, Stone V, Erzinclioglu S, Martin L, Baron-Cohen S, et al. Theory of mind in patients with frontal variant frontotemporal dementia and Alzheimer's disease: theoretical and practical implications. Brain. 2002. 125:752–764.

24. The ALS CNTF treatment study (ACTS) phase I-II Study Group. The Amyotrophic Lateral Sclerosis Functional Rating Scale. Assessment of activities of daily living in patients with amyotrophic lateral sclerosis. Arch Neurol. 1996. 53:141–147.
25. Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998. 51:1546–1554.

26. Neary D, Snowden JS, Mann DM. Cognitive change in motor neurone disease/amyotrophic lateral sclerosis (MND/ALS). J Neurol Sci. 2000. 180:15–20.

27. Abrahams S, Leigh PN, Harvey A, Vythelingum GN, Grisé D, Goldstein LH. Verbal fluency and executive dysfunction in amyotrophic lateral sclerosis (ALS). Neuropsychologia. 2000. 38:734–747.

28. Strong MJ, Grace GM, Orange JB, Leeper HA, Menon RS, Aere C. A prospective study of cognitive impairment in ALS. Neurology. 1999. 53:1665–1670.

29. Grossman AB, Woolley-Levine S, Bradley WG, Miller RG. Detecting neurobehavioral changes in amyotrophic lateral sclerosis. Amyotroph Lateral Scler. 2007. 8:56–61.

30. Viskontas IV, Possin KL, Miller BL. Symptoms of frontotemporal dementia provide insights into orbitofrontal cortex function and social behavior. Ann N Y Acad Sci. 2007. 1121:528–545.

31. Perry RJ, Miller BL. Behavior and treatment in frontotemporal dementia. Neurology. 2001. 56:S46–S51.

32. Swartz JR, Miller BL, Lesser IM, Darby AL. Frontotemporal dementia: treatment response to serotonin selective reuptake inhibitors. J Clin Psychiatry. 1997. 58:212–216.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download