Abstract
Background and Purpose
Stroke imposes a major burden on patients, their families, and the national healthcare system. The purpose of this study was to determine the itemized hospital charges in acute ischemic stroke patients according to their severity by partitioning the charges in detail and then examining whether stroke severity was a significant contributor to these charges.
Methods
This study analyzed data of first-time acute ischemic stroke patients who had been admitted to an academic medical center between September 2003 and April 2009. The patients' demographic and clinical characteristics were analyzed descriptively, and then eight categorized hospital charges as well as the total charge were compared among patients grouped according to stroke severity, using analysis of variance. Multiple regression analyses were conducted to test the influence of stroke severity on itemized hospital charges as well as the total charge, while controlling for other related factors.
Results
More-severe strokes were associated with a higher total charge. Significantly higher charges were associated with patients with more-severe strokes regarding all charged items except imaging studies. The charges for imaging studies were similar across all severities of stroke. While controlling for other factors, a significant impact of stroke severity was found in both the total hospital charge and most itemized charges.
The economic burden of stroke on the healthcare system has been studied in several countries.1-5 Typically more than half of the economic burden is attributed to direct medical costs,1,4 and a major component of this burden is inpatient services for acute hospital admission.3,6 Previous studies found that the total cost of hospitalization due to stroke was significantly associated with the length of stay (LOS), stroke severity, clinical subtype, and certain sociodemographic factors,3,6-10 of which LOS was found to be the most decisive factor in determining the total cost of hospitalization of stroke patients.3,7,11 This has led to suggestions that shortening the LOS would be an effective and critical strategy for managing healthcare costs.12,13
With regard to the clinical factors, stroke severity was clearly observed to have a significant impact on hospital charges in stroke patients.6,9,10,14-18 Thus, it is recommended that stroke severity should be included in any decisions regarding the allocation of healthcare resources, especially when the impact of certain therapeutic approaches is assessed in stroke patients.9 Although stroke severity is known to be an important factor in determining the total charges of acute hospitalization for ischemic stroke patients, the detailed pattern of itemized charges relative to stroke severity has not been fully explored; more specifically, there needs to be a greater understanding of how stroke severity differentiates specific items of charges and how this influences the distribution of itemized charges.
Thus, this study focused on investigating the itemized hospital charges in ischemic stroke patients according to stroke severity by dividing the charges in greater detail, and then determining whether the stroke severity was a significant contributor to these itemized hospital charges when the major factors influencing those charges were controlled.
This was a retrospective study that involved analyzing the itemized hospital charges of cerebral infarction patients hospitalized in an academic medical center. The subjects comprised 1600 consecutive patients with acute, first-time ischemic stroke, who were admitted within 7 days of stroke onset to the neurology ward between September 2003 and April 2009. The patients were diagnosed based on the results of anamnesis, neurological testing, computed tomography, magnetic resonance imaging, magnetic resonance angiography, and other neuroradiological findings. The study was approved by the institutional review board of the Kyung Hee University Medical Center, Seoul, Korea. The board permitted a waiver of informed consent because the study involved anonymous data collected for nonresearch purposes.
The data comprised two parts: 1) each patient's demographic and clinical characteristics, and 2) information on hospital charges. The data for the first part were collected from a database of the hospital's stroke registry, and those for the second part were retrieved from the hospital's Patient Management Information.
The demographic characteristics included age, gender, and risk factors (e.g., prior history of transient ischemic attack, smoking, and comorbid conditions such as hypertension, diabetes mellitus, and heart diseases). The clinical characteristics consisted of the severity of each patient's stroke at admission, treatment methods, admission and discharge route, intensive care unit (ICU) admission, and LOS at the hospital. These variables were selected based on previous studies finding that they directly impact on the hospital charges of stroke patients.
At the time of admission, each patient's stroke severity was evaluated using the National Institutes of Health Stroke Scale (NIHSS) and was classified into one of three groups using the criteria reported by Schlegel et al.:19 mild (NIHSS score ≤5), moderate (NIHSS score 6-13), or severe (NIHSS score >13). With regard to the stroke subtype, each patient was classified according to the Trial of Org 10172 in Acute Stroke Treatment criteria.
The data on hospital charges were categorized into 24 detailed items that were then grouped into the following 8 categories to simplify the analysis and subsequent comparisons: physicians' fees, room and board, medication, injections, operations and procedures, laboratory tests, imaging studies, and other charges.
The patients' demographic and clinical characteristics were analyzed descriptively using frequencies, percentages, means, and medians. The means of total and itemized hospital charges among stroke severity groups were compared using analysis of variance. Multiple regression models, which controlled for other factors influencing inpatient charges such as the patients' gender, age, treatment methods, LOS, and referral status at both admission and discharge were developed. The regression models excluded other charges due to heterogeneous properties. In the multiple regression analysis, the logarithm of the hospital charges was a dependent variable because the hospital charges showed an asymmetric distribution, with a large difference between the mean and median. The variance inflation factor for each predictor for all given cases was computed to detect the existence of multicollinearity. All analyses were performed using the Statistical Analysis System (version 9.1).
Along with the analysis, inpatient charges were converted to US dollars to enable comparison of the results of this study with those of others, with the exchange rate US$ 1=1192 Korean won (valid in December 2003) being used. In addition, based on the official medical fee schedules from 2003 to 2009, all monetary values were adjusted to their 2003 equivalents.
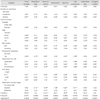
The mean and median NIHSS scores at admission were 5.7 and 4, respectively; 65% of strokes were mild, 24% of strokes were moderate, and 10% of strokes were severe. The strokes were distributed among the different subtypes of the Trial of Org 10172 in Acute Stroke Treatment classification as follows: large-artery sclerosis (34%), small-vessel occlusion (35%), cardioembolism (10%), undetermined etiology (20%), and other determined etiology (2%). The mean and median LOSs were 15 and 10 days, respectively. Deaths during hospitalization occurred in 1% of the cases, and 15% and 84% were referred to other medical institutions and returned to home at discharge, respectively (Table 1).
The mean total charge for a hospital stay was US$ 3595 (median US$ 2787). This was divided into room and board charges (30.7%), imaging studies (29.9%), laboratory tests (13.2%), injections (11.4%), operations and procedures (7.7%), medication (3.8%), and physicians' fees (1.1%) (Table 2).
The total charge differed significantly with the stroke severity (F=122.9; p<0.001): US$ 2859 for mild stroke, US$ 4444 for moderate stroke, and US$ 6242 for severe stroke (Table 2). Detailed analysis also showed that significantly higher charges were associated with patients with more-severe strokes for all charge items except for imaging studies. The charges for imaging studies were similar across the patient stroke severity groups (F=1.4; p=0.242): US$ 1069 for mild strokes, US$ 1110 for moderate strokes, and US$ 1029 for severe strokes. Accordingly, the proportion of the total charge attributable to imaging studies decreased significantly with increasing stroke severity: 37.4% for mild strokes, 25.0% for moderate strokes, and 16.5% for severe strokes. The proportions of the charges associated with injections and with operations and procedures relative to the total charge increased noticeably for patients with more-severe strokes.
After controlling for other factors influencing inpatient charges, stroke severity at admission was a significant factor related to increasing the total charge, as were diabetes mellitus, surgical operation, ICU admission, and LOS; in contrast, gender (female), age, and referral for admission were significant factors in reducing the total charge (Table 3).
Multiple regression models for itemized charges revealed that stroke severity was a significant factor for charges involving physicians' fees, medication, injections, operations and procedures, laboratory tests, and imaging studies. Higher charges were imposed on patients with higher stroke severity in four models, with the exceptions of medication and imaging studies.
Female gender and old age were significant factors reducing both the total charge and the laboratory test charge, but old age was also a significant factor associated with increasing the medication charge. Diabetes mellitus was a significant factor in increasing the total charge as well as all itemized charges, with the exception of physicians' fees and the charge for imaging studies. Surgery and ICU admission were found to be significant factors increasing the total charge and four of the itemized charges. Although thrombolytics use was a significant factor in reducing the charge for medication while increasing the charges for injections, operations and procedures, laboratory tests, and imaging studies, it did not have a measurable impact on the total charge. A longer LOS was associated with an increased total charge as well as all itemized charges except those related to imaging studies. Death at discharge was a significant factor in reducing the charges for room and board and for medication, while increasing those for physicians' fees, injections, operations and procedures, and laboratory tests. Referral after hospital discharge increased the charges for room and board, operations and procedures, and laboratory tests.
With regard to the variance inflation factors for the multiple regression models, there was no indication of the presence of multicollinearity - a value greater than 10 is often regarded as indicating multicollinearity, but the largest value was 1.87 in this study. This value satisfies the condition that estimated regression coefficients will not reveal any linear dependencies between variables.
This study found that the total inpatient charge and itemized hospital charges differed according to stroke severity in first-ever acute ischemic stroke patients, and that stroke severity was a significant determinant of several itemized hospital charges as well as the total charge after controlling for the major factors influencing hospital charges.
Higher stroke severity was associated with a higher total hospital charge, and patients with severe strokes paid 2.2 times more in total inpatient charges than did patients with mild strokes. This variation in the total hospital charge with stroke severity was consistent with the findings of previous studies.6,7,9,10,15,18
The charges and their distribution among eight of the categories varied with the stroke severity, with only the charge for imaging studies not varying significantly. The proportion of the total charge allocated to imaging studies decreased considerably in the moderate and severe groups. This finding suggests that most imaging studies are performed for diagnostic purposes at a very early stage of hospitalization regardless of stroke severity. Further studies are needed to obtain a greater in-depth understanding of the utilization of major imaging techniques such as computed tomography, magnetic resonance imaging, and sonography.
Stroke severity was a significant determinant of the total charge and six itemized charges, with a higher stroke severity increasing the total and the itemized charges. The exceptions were the charges for room and board, medication, and imaging studies. Results from bivariate analysis suggest that in spite of a trend toward increasing charge for room and board with increasing stroke severity, the impact of severity on charge for room and board was not statistically significant when LOS was included in the multivariate regression model. The charge related to medication decreased in the severe-stroke group in multivariate analysis, while it was observed to increase in the same patients in bivariate analysis. The same routine imaging studies tended to be applied to evaluate and diagnose the condition of patients regardless of stroke severity.
The elderly were found to pay lower total and laboratory test charges. This could have been due to younger stroke patients requiring more examinations.20 Diabetes mellitus and smoking have previously been found to be significant factors in determining medical costs,9,10 and their inclusion in the regression model revealed that smoking did not significantly increase medical charges, while diabetes mellitus increased the total hospital charge and all itemized charges except for the physicians' fees and imaging studies charge.
The findings of this study are consistent with those of previous studies,3,7,11 in that LOS was found to be the most important factor in influencing the hospital charges of stroke patients. LOS was a significant factor in increasing not only the total charge but also all itemized charges other than that for imaging studies. ICU admission and surgery, which were significant determinants of the medical cost along with the LOS and stroke severity in previous studies,10,15,17,18 were also significant factors increasing the total and four of the itemized hospital charges. The imaging studies and laboratory test categories followed room and board as the next largest inpatient charges. These two categories contributed more than 40% of the total inpatient charges for ischemic stroke patients.
While it is difficult to directly compare this study with previous studies due to the use of different categories of charge (or cost) data,3,7,12,18,21 comparison was made possible by reorganizing the charges of similar items. In particular, three categories - pharmaceutical care, laboratory tests, and imaging studies - were comparable. Along with the variation in total charge per patient across countries, there were different proportional distributions of itemized charges for pharmaceutical care (3-49%), laboratory tests (5-13%), and imaging studies (9-30%). The present study revealed a higher proportional charge for these three items, and especially for imaging studies. These discrepancies may be at least partial due to healthcare delivery systems differing between countries, in terms of the medical reimbursement system, utilization pattern of healthcare services, and categories of hospital charges. This is particularly true of Korea, whose special characteristic of a regulated fee-for-service system has a significant impact on the composition of hospital charges. Other special characteristics include unusually low physicians' fees, relatively high laboratory test charges, and high-priced uninsured medical services and high-technology imaging studies.22 Furthermore, pharmaceutical care represents a higher proportion of the total charge in Korea. The differences in healthcare and reimbursement systems between countries warrant more detailed studies of itemized hospital charges for the purposes of international comparison to achieve a greater understanding of healthcare in different countries (Table 4).
Despite the large included sample, the subjects in this study were from only one hospital. This might have adversely affected the external validity, preventing us from making generalizations to other populations. Therefore, expanded research conducted across multiple hospitals is necessary. The utilization of charge data, rather than cost data, might not be a shortcoming of this study. Although Finkler indicated a potential problem of using charge data as a proxy of costs in efficiency-related research,23 the present study focused only on the level of healthcare utilization and charges, not those related to efficiency. In addition, the findings of this study are consistent with those of previous studies that analyzed the charge data of ischemic stroke patients in Japan and China.3,16 Moreover, especially in the fee-for-service reimbursement system of Korea, using charge data is considered to be permissible in comparative studies of healthcare utilization because hospital charges are itemized in detail.
This analytical study has detailed the hospital charges of the inpatient services of our local population with acute ischemic stroke. The findings (from a small study cohort) suggest that hospital charges differ according to stroke severity and that stroke severity is a significant contributing factor in several itemized charges as well as the total charge. More specifically, the findings suggest that stroke severity is a statistically significant factor influencing the composition of hospital charges for ischemic stroke patients, after controlling for major factors such as treatment methods, LOS, and other demographic factors. The results suggest that severity levels should be considered when developing fee schedules for health insurance reimbursement, when planning more-efficient and effective treatment strategies, and when evaluating the appropriateness of healthcare resource utilization, especially for ischemic stroke patients.
Figures and Tables
References
1. Matchar DB, Duncan PW. Cost of stroke. Stroke Clin Updates. 1994. 5:9–12.
2. Dewey HM, Thrift AG, Mihalopoulos C, Carter R, Macdonell RA, McNeil JJ, et al. Cost of stroke in Australia from a societal perspective: results from the North East Melbourne Stroke Incidence Study (NEMESIS). Stroke. 2001. 32:2409–2416.

3. Tu F, Anan M, Kiyohara Y, Okada Y, Nobutomo K. Analysis of hospital charges for ischemic stroke in Fukuoka, Japan. Health Policy. 2003. 66:239–246.

4. Gerzeli S, Tarricone R, Zolo P, Colangelo I, Busca MR, Gandolfo C. The economic burden of stroke in Italy. The EcLIPSE Study: Economic Longitudinal Incidence-based Project for Stroke Evaluation. Neurol Sci. 2005. 26:72–80.

5. Lim SJ, Kim HJ, Nam CM, Chang HS, Jang YH, Kim S, et al. [Socioeconomic costs of stroke in Korea: estimated from the Korea national health insurance claims database]. J Prev Med Public Health. 2009. 42:251–260.

6. Caro JJ, Huybrechts KF, Duchesne I. Management patterns and costs of acute ischemic stroke: an international study. For the Stroke Economic Analysis Group. Stroke. 2000. 31:582–590.

7. Diringer MN, Edwards DF, Mattson DT, Akins PT, Sheedy CW, Hsu CY, et al. Predictors of acute hospital costs for treatment of ischemic stroke in an academic center. Stroke. 1999. 30:724–728.

8. Claesson L, Gosman-Hedström G, Johannesson M, Fagerberg B, Blomstrand C. Resource utilization and costs of stroke unit care integrated in a care continuum: a 1-year controlled, prospective, randomized study in elderly patients: the Göteborg 70+ Stroke Study. Stroke. 2000. 31:2569–2577.

9. Chang KC, Tseng MC. Costs of acute care of first-ever ischemic stroke in Taiwan. Stroke. 2003. 34:e219–e221.

10. Chang H, Yoon SS, Kwon YD. Determinants of inpatient charges of acute stroke patients in two academic hospitals: comparison of intracerebral hemorrhage and cerebral infarction. J Korean Neurol Assoc. 2009. 27:215–222.
11. Mamoli A, Censori B, Casto L, Sileo C, Cesana B, Camerlingo M. An analysis of the costs of ischemic stroke in an Italian stroke unit. Neurology. 1999. 53:112–116.

12. Ma Y, Liu Y, Fu HM, Wang XM, Wu BH, Wang SX, et al. Evaluation of admission characteristics, hospital length of stay and costs for cerebral infarction in a medium-sized city in China. Eur J Neurol. 2010. 17:1270–1276.

13. Wei JW, Heeley EL, Jan S, Huang Y, Huang Q, Wang JG, et al. Variations and determinants of hospital costs for acute stroke in China. PLoS One. 2010. 5:pii: e13041.

14. Caro JJ, Huybrechts KF, Kelley HE. Predicting treatment costs after acute ischemic stroke on the basis of patient characteristics at presentation and early dysfunction. Stroke. 2001. 32:100–106.

15. Reed SD, Blough DK, Meyer K, Jarvik JG. Inpatient costs, length of stay, and mortality for cerebrovascular events in community hospitals. Neurology. 2001. 57:305–314.

16. Tu F, Tokunaga S, Deng Z, Nobutomo K. Analysis of hospital charges for cerebral infarction stroke inpatients in Beijing, People's Republic of China. Health Policy. 2002. 59:243–256.

17. Sekimoto M, Kakutani C, Inoue I, Ishizaki T, Hayashida K, Imanaka Y. Management patterns and healthcare costs for hospitalized patients with cerebral infarction. Health Policy. 2008. 88:100–109.

18. Gioldasis G, Talelli P, Chroni E, Daouli J, Papapetropoulos T, Ellul J. In-hospital direct cost of acute ischemic and hemorrhagic stroke in Greece. Acta Neurol Scand. 2008. 118:268–274.

19. Schlegel D, Kolb SJ, Luciano JM, Tovar JM, Cucchiara BL, Liebeskind DS, et al. Utility of the NIH Stroke Scale as a predictor of hospital disposition. Stroke. 2003. 34:134–137.

20. Putaala J, Metso AJ, Metso TM, Konkola N, Kraemer Y, Haapaniemi E, et al. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: the Helsinki young stroke registry. Stroke. 2009. 40:1195–1203.

21. Dodel RC, Haacke C, Zamzow K, Paweilik S, Spottke A, Rethfeldt M, et al. Resource utilization and costs of stroke unit care in Germany. Value Health. 2004. 7:144–152.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download