Abstract
Background and Purpose
Migraine patients are particularly prone to the complication of medication-overuse headache (MOH). Although it has been shown that A allele carriers for the tumor necrosis factor (TNF)-β gene G252A polymorphism are at high risk of the development of migraine without aura, the relationship between the TNF-β gene G252A polymorphism and MOH is unknown. We investigated whether the TNF-β gene G252A polymorphism is involved in the aggravation of migraine by overuse of medications.
Methods
Forty-seven migraine patients (6 males and 41 females; age 36.4±10.3 years, mean±SD) and 22 MOH patients (1 male and 21 females; age 39.6±9.9 years) who had migraine were included in this study. The genotype for the TNF-β gene G252A polymorphism was determined by polymerase-chain-reaction restriction-fragment-length polymorphism analysis.
Migraine is a common neurological disease that affects approximately 8.4% of the general population.1 Migraine patients are particularly prone to the complication of medication-overuse headache (MOH).2,3 Previous studies have shown that a high percentage of MOH patients have migraine as a primary headache.4,5 Moreover, 56.8% of migraine sufferers use over-the-counter medicines (combination analgesics) alone,1 and 85.1% of MOH patients overuse combination analgesics.4 Although most patients return to the episodic migraine pattern after drug withdrawal, MOH dramatically decreases the quality of life for patients.3 In addition, MOH patients, in contrast to migraine patients, have a higher percentage of comorbidity with depression.5,6 Therefore, it is important to prevent the aggravation of migraine by overuse of medications.
The pathogenesis of migraine is known to be related to the presence of genetic polymorphisms, including those of cytokine-related genes.7 It has been shown that cytokines such as tumor necrosis factor (TNF)-α and interleukin (IL)-1 play an important role in neurogenic inflammation.8 A previous study demonstrated that serum levels of TNF-α IL-1β, and IL-10 are higher during attacks than during the interattack period in patients with migraine.9 A genotyping approach revealed that A allele carriers for the TNF-β gene G252A polymorphism are at high risk of the development of migraine without aura (MO).10,11 Moreover, MOH patients who have migraine for primary headache frequently initially have MO.3 Therefore, it is possible that the TNF-β gene G252A polymorphism contributes to the pathogenesis of both MO and MOH. However, we found no reports on studies showing the relationship between cytokine-related gene polymorphisms and MOH.
The aim of the present study was therefore to determine the association between the TNF-β gene G252A polymorphism and MOH.
We enrolled 47 migraine and 22 MOH patients who were admitted to the Department of Neurology in an outpatient clinic of Showa University East Hospital, Tokyo, Japan, between May 2010 and January 2011. Migraine was diagnosed according to the International Classification of Headache Disorders, 2nd Edition (ICHD-II) in 2004.12 Moreover, we confirmed by interview that the migraine patients had no experience of medication overuse. The revised ICHD-II criteria were used for diagnosing MOH.3 MOH patients were asked about their primary headache by headache specialists, who also confirmed the primary headache after curing the patient of MOH, according to the ICHD-II criteria. Although the cohort included not only patients with migraine but also those with both migraine and tension-type headaches, the latter were excluded from this study. The diagnosis of major depressive disorder was confirmed using the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.13
All patients were Japanese and gave their informed consent to participate in this study. We enrolled all patients with migraine and patients with MOH; the patients were not actively selected. The clinical study was approved by the Ethics Committee for Genome Research of Showa University.
Genomic DNA was extracted from the patients' whole blood using NucleoSpin Blood QuickPure (NIPPON Genetics, Tokyo, Japan). The TNF-β gene G252A (rs909253) polymorphism was determined using a polymerase chain reaction (PCR)-based method in accordance with the method of Asuni et al.11 The sense oligonucleotide primer for TNF-β gene G252A was 5'-GGT TTC CTT CTC TGT CTC TGA CTC TCC-3', and the antisense primer was 5'-GAG AGA GAT CGA CAG AGA AGG GGA C-3'. PCR products were digested for 10-12 h at 37℃ with Nco I. The 173-bp fragment indicates the presence of the A allele (no Nco I restriction site) and the 102- and 71-bp fragments indicate the presence of the G allele (presence of Nco I restriction site). Nco-I-treated PCR fragments were run on 3% agarose gels and stained with ethidium bromide (Fig. 1).
Post-hoc analysis was performed with an α error of 5% (http://www.dssresearch.com/toolkit/spcalc/power_a1.asp). Categorical variables were analyzed by the χ2 test or Fisher's exact test using SPSS 11.0 J software (SPSS, Tokyo, Japan). Probability values of p<0.05 were considered statistically significant.
The study population comprised 69 patients, including 47 with migraine (6 males and 41 females aged 36.4±10.3 years, mean±SD): 5 had migraine with aura (MA), 36 had MO, and 6 had MA+MO. Of the entire cohort, 22 had MOH (1 male and 21 females aged 39.6±9.9 years): 1 with MA and 21 with MO (Table 1). Although the difference was not significant, MOH patients who had MO as the primary headache tended to be more common than MO patients in the migraine group (MO vs. MA and MA+MO, p=0.087) (Table 1). The experience of depression was significantly more frequent in MOH patients than in migraine patients (p<0.001). The overused medication was combination analgesic in 14 patients (64%), analgesic in 9 patients (41%), and triptan in 2 patients (9%) (Table 1).
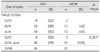
The TNF-β gene G252A genotype frequencies of the cohort are listed in Table 2. The frequencies of the 252G/A and A/A genotypes were significantly higher in patients with MOH than in patients with migraine (G/G vs. G/A+A/A, p=0.013) (Table 2). While the frequency of the G/G genotype was 23% in migraine patients, it was absent in MOH patients (Table 2). As listed in Table 3, the frequencies of the 252G/A and A/A genotypes were significantly higher in patients with MOH who had MO than in patients with MO (G/G vs. G/A+A/A, p=0.021) (Table 3).
This study is the first to reveal that the TNF-β gene G252A polymorphism contributes to the complication of MOH in patients with migraine, and especially those with MO, and that G/G genotype carriers appear to be less susceptible to the aggravation of migraine by overuse of medications.
Cytokines are important mediators of inflammatory pathways, and the serum levels of cytokines such as TNF-α are higher during attacks than in the interattack period in patients with migraine.9 The genes for TNF-α and TNF-β are located in tandem within the major histocompatibility complex on the short arm of chromosome 6 (6p21.3). Interestingly, the A/A genotype for the TNF-β gene G252A polymorphism is known to be associated with higher TNF-α production.14 On the other hand, Abraham et al.15 showed that the G allele is associated with higher TNF-α production in lymphoblastoid cell lines. Messer et al.16 reported that the A allele is related to increased TNF-β production. Thus, the association between the TNF-β gene G252A polymorphism and TNF production is controversial. However, it can be stated that since the TNF-β gene G252A gene polymorphism is a silent mutation, it may have linkage disequilibrium with other functional mutations. Future research should determine the relationships between TNF-α, TNF-β and the complications of MOH in patients with migraine, and investigate both the TNF-related gene polymorphisms and the serum levels of their proteins in patients.
In this study we did not collect data from healthy control subjects, because the aim was to determine the involvement of the TNF-β gene G252A polymorphism in the aggravation of migraine by overuse of medications. Hagiwara et al.17 reported that the distribution of the TNF-β gene G252A polymorphism in Japanese healthy controls was as follows: G/G in 12.5%, G/A in 50.0%, and A/A in 37.5%. The genotype distribution did not differ between the MO patients in the present study and the healthy controls in the study of Hagiwara et al. (G/G vs. G/A+A/A, p=0.122). Moreover, we found that the genotype distribution did not differ significantly between MOH patients who had MO and healthy controls (G/G vs. G/A+A/A, p=0.097). Since a significant difference was observed between MO and MOH groups, it appears that the TNF-β gene G252A polymorphism is involved in the aggravation of MO by overuse of medications.
Among the 22 patients with MOH, 64% overused a combination analgesic, a finding that is similar to those of Imai et al.4 and Kanki et al.5 It is known that a high percentage of MOH patients initially have MO.3 In the present study, although the difference was not significant, we observed that MOH patients who had MO as a primary headache tended to be more common than MO patients in the migraine group. The frequency of comorbidity with depression was higher among MOH patients than among migraine patients.5,6 We also confirmed that the experience of depression is significantly more frequent in MOH patients than in migraine patients. Although the sample was small in this study, the background of the subjects appears to be coincident with those of subjects in previous studies. Moreover, although the migraine patient has the potential to develop the complication of MOH in the future, the frequency of the TNF-β gene G252A polymorphism differed significantly between the migraine and MOH groups in this study.
In conclusion, we have demonstrated that the TNF-β gene G252A polymorphism may be one of the factors contributing to the aggravation of migraine by overuse of medications. Since the sample size is the biggest limitation of this study, future studies with larger samples must be undertaken to elucidate the relationship between the TNF-β gene G252A polymorphism and MOH.
Figures and Tables
 | Fig. 1Genotyping of the TNF-β gene G252A polymorphism. PCR products were digested with Nco I under optimized conditions. The 173-bp fragment indicates the presence of the A allele (no Nco I restriction site) and the 102- and 71-bp fragments indicate the presence of the G allele (presence of Nco I restriction site). Digestion products were analyzed using 3% agarose gel. PCR: polymerase chain reaction, TNF: tumor necrosis factor. |
Acknowledgements
We are gratefully to all of the volunteers for their participation. This study was supported in part by a grant from the Private University High Technology Research Center Project, matching a fund subsidy from the Ministry of Education, Culture, Sport, Science, and Technology, Japan (MEXT).
References
1. Sakai F, Igarashi H. Prevalence of migraine in Japan: a nationwide survey. Cephalalgia. 1997. 17:15–22.
2. Bahra A, Walsh M, Menon S, Goadsby PJ. Does chronic daily headache arise de novo in association with regular use of analgesics? Headache. 2003. 43:179–190.

3. Headache Classification Committee. Olesen J, Bousser MG, Diener HC, Dodick D, First M, et al. New appendix criteria open for a broader concept of chronic migraine. Cephalalgia. 2006. 26:742–746.

4. Imai N, Kitamura E, Konishi T, Suzuki Y, Serizawa M, Okabe T. Clinical features of probable medication-overuse headache: a retrospective study in Japan. Cephalalgia. 2007. 27:1020–1023.

5. Kanki R, Nagaseki Y, Sakai F. Medication-overuse headache in Japan. Cephalalgia. 2008. 28:1227–1228.

6. Kaji Y, Hirata K. Characteristics of mood disorders in Japanese patients with medication-overuse headache. Intern Med. 2009. 48:981–986.

9. Perini F, D'Andrea G, Galloni E, Pignatelli F, Billo G, Alba S, et al. Plasma cytokine levels in migraineurs and controls. Headache. 2005. 45:926–931.

10. Trabace S, Brioli G, Lulli P, Morellini M, Giacovazzo M, Cicciarelli G, et al. Tumor necrosis factor gene polymorphism in migraine. Headache. 2002. 42:341–345.

11. Asuni C, Stochino ME, Cherchi A, Manchia M, Congiu D, Manconi F, et al. Migraine and tumour necrosis factor gene polymorphism. An association study in a Sardinian sample. J Neurol. 2009. 256:194–197.

12. Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004. 24:Suppl 1. 9–160.
13. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. 2000. 4th ed, text revision. Washington, D.C.: American Psychiatric Association.
14. Grimble RF, Howell WM, O'Reilly G, Turner SJ, Markovic O, Hirrell S, et al. The ability of fish oil to suppress tumor necrosis factor α production by peripheral blood mononuclear cells in healthy men is associated with polymorphisms in genes that influence tumor necrosis factor α production. Am J Clin Nutr. 2002. 76:454–459.

15. Abraham LJ, French MA, Dawkins RL. Polymorphic MHC ancestral haplotypes affect the activity of tumour necrosis factor-alpha. Clin Exp Immunol. 1993. 92:14–18.

16. Messer G, Spengler U, Jung MC, Honold G, Blömer K, Pape GR, et al. Polymorphic structure of the tumor necrosis factor (TNF) locus: an NcoI polymorphism in the first intron of the human TNF-β gene correlates with a variant amino acid in position 26 and a reduced level of TNF-β production. J Exp Med. 1991. 173:209–219.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download