This article has been
cited by other articles in ScienceCentral.
Abstract
Background and Purpose
Cervical radiculopathy is a pathological process involving a nerve root of the cervical spine. The most common causes of radiculopathy are cervical disc herniation followed by cervical spondylosis. The aim of this study was to determine the effect of dropped shoulder as a cause of lower cervical radiculopathy.
Methods
In total, 132 patients, comprising 105 women (79.5%) and 27 men (20.5%; female : male ratio of 4 : 1) and a mean age of 36.7 years (range 18-58 years), were included in this study. All of the patients presented with shoulder pain, and were investigated by cervical X-ray, cervical magnetic resonance imaging, serum muscle enzymes, and electromyography (EMG)/nerve-conduction studies.
Results
Ninety six patients (72.7%) exhibited visually detectable dropped shoulder. The lateral view X-ray of the cervical region revealed eight or more vertebrae. In 119 patients (90.2%), the EMG revealed a mild-to-moderate or moderate denervation patterns in the abductor digiti minimi, first dorsal interosseous, and flexor carpi ulnaris muscles, while the abductor pollicis brevis, extensor carpi radialis, and triceps brachii were denervated in 102 patients (77.3%). All of the patients had lower cervical paraspinal muscles with a denervation pattern.
Conclusions
Three criteria for diagnosing dropped shoulder syndrome have been suggested: pain with consistent anatomical distribution, X-ray abnormalities, and EMG abnormalities. Compression of the cervical roots by muscle spasm has been proposed as the cause of dropped shoulder syndrome; this possibility is discussed herein.
Keywords: lower cervical radiculopathy, dropped shoulder syndrome, electromyography/nerve-conduction study
Introduction
Cervical radiculopathy is a pathological process involving a nerve root of the cervical spine, whereby the seventh (C7; 60%) and sixth (C6; 25%) cervical nerve roots are the most commonly affected.
1-
7 Cervical radiculopathy secondary to intervertebral disc disease accounts for 36% of all spinal radiculopathies of intervertebral disc disease, second only to lumbar radiculopathy disease, which accounts for 62% of all spinal radiculopathies.
8 It has an annual incidence of 107.3 per 100,000 for men and 63.5 per 100,000 for women, with a peak at 50-54 years of age.
4,
9 The most common causes of radiculopathy are cervical disc herniation followed by cervical spondylosis.
1
The clinical presentations associated with cervical radiculopathy include neck pain with muscle spasm, mild-to-moderate peripheral numbness, shooting pain, and upper extremity weakness in the distribution of the entrapped nerve root. The sensory symptoms such as burning, tingling, or both typically follow a dermatomal distribution, while the pain is more com-monly referred in a myotomal pattern.
1,
9-
11 Physical examination findings vary depending on the level of the radiculopathy and on whether there is associated myelopathy. The nerve root that is most commonly affected is C7, followed by C6.
4,
9
Patients with cervical radiculopathy are usually investigated by one or more of the imaging techniques, with or without electrophysiological testing. Magnetic resonance imaging (MRI) is the imaging technique of choice in patients with cervical radiculopathy.
9,
12 Needle electromyography (EMG) and nerve-conduction studies (NCS) can be helpful when a patient's history and physical examination are inadequate to distinguish cervical radiculopathy from other neurologic causes of neck and arm pain.
9,
13
The author has noticed that a considerable number of Yemeni people have a small body build with visually detectable bilaterally dropped shoulders. They present with pain in one shoulder or both shoulders that radiates to the ipsilateral upper limb, and other adjacent anatomical regions. Since this is a common condition, people in Yemen rely on their traditional remedies to treat shoulder pain. This condition is called Metna or Asaba in the local terminology.
Dropped shoulder syndrome (DSS) is the suggested name for the condition presented by the patients involved in the present study. The patients present with symptoms of cervical radiculopathy involving the lower cervical roots, hence the use of the term lower cervical radiculopathy. The diagnosis is based on clinical, radiological, and electrophysiological criteria.
The aim of this study was to determine the role of dropped shoulder as a cause of lower cervical radiculopathy.
Methods
The study included 132 patients, comprising 105 (79.5%) females and 27 (20.5%) males, giving with a female : male ratio of 4 : 1. The study was conducted in Azal Hospital in Sana'a, Yemen between June 2008 and February 2010. After obtaining the approval of the Azal Hospital Ethical Standards Committee, each patient signed a special consent form, in accordance with international standards of investigations on human subjects. The patient's age ranged between 18 and 58 years, with an average age of 36.7 years.
The presenting symptom in all patients was shoulder pain. Of the 488 patients with shoulder pain that had been seen at the neurology clinic during the period of the study, 356 patients (79%) were excluded after it was shown that connective tissue, peripheral polyneuropathy (including diabetic neuropathic disorders), carpal tunnel syndrome, or other conventional detectable conditions were the cause of the shoulder and/or upper limb pain. All of the included patients were Qat chewers.
Each patient was thoroughly examined for signs of any neural, arterial, and/or venous compression (
Table 2). Plain cervical X-ray, muscle enzymes (creatine phosphokinase, lactate dehydrogenase, alanine aminotransferase, and aspartate aminotransferase), EMG, and NCS (using a Sapphire II, Medelec EMG machine and electrical stimulation) were performed for all of the patients. The EMG records were analyzed irrespective of the patients' clinical data to eliminate the bias of visual assessment. The number, amplitude, and duration of the motor unit potentials (MUPs) were measured for every record to obtain objective data for EMG record analysis. Cervical MRI/interscaline triangle MRI was also conducted for all of the patients prior to the diagnosis of DSS, using T1-weighted, T2-weighted, and protondensity image series.
After the diagnosis of DSS, all patients were advised to perform isotonic physiotherapeutic exercise. That exercise was aimed at strengthening the muscles that hold the shoulders upright (trapezius, sternocleidomastoid, and levator scapulae muscles). The prescribed exercise involves the application of moderate downward pressure on both shoulders by the therapist, who stands behind the patient, while the seated patient is asked to push maximally upward, then back to the neutral position. This exercise was repeated until the patient began to feel tiredness or pain in the shoulder(s). Physiotherapy exercise was performed twice daily for 12-18 weeks, with an average of 14 weeks.
A control group of 30 age-matched volunteer subjects (18 females and 12 males) was selected. They underwent the same physiotherapeutic exercises to compare the effectiveness of the shoulder exercises between normal and affected subjects.
Any improvement in pain after performing the physiotherapy was estimated fortnightly for each patient using a nume-rical rating scale14 that constituted a self-assessment pain sc-ore from 0 to 10. The patient was instructed to choose a number from 0 to 10 that best described the intensity of their pain, whereby "0" signifies "no pain" and "10" signifies "the worst possible pain." This pain score was recorded before, during, and after the completion of physiotherapeutic exercise.
Results
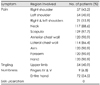
The presenting symptom in all of the patients was shoulder pain, on the right in 57 patients (43.2%), on the left in 54 patients (40.9%), and on both sides in 21 patients (15.9%). The pain radiated to the neck, ipsilateral scapular region, lateral chest wall, anterior chest wall, arm, and forearm, or to the hand. The pain was associated with numbness of the little and ring fingers in 9 patients (6.8%) and of the palm of the hand in 72 (54.5%). A tingling sensation was present in 54 of the patients (40.9%)(
Table 1). Other associated symptoms are presented in
Table 1. The shoulder pain was on the same side as the lateral bending assumed when sitting to chew Qat.
Table 2 presents the physical signs detected by clinical examination, and indicates that 96 patients (72.7%) had visibly dropped shoulders. Both arms were symmetrical, with no evident restriction of neck movement. Mild-to-moderate atrophy of the small muscles of the hand (of the affected side) was seen in 28 patients (21%). None of the patients showed any clinically detectable sign of proximal muscle weakness of the upper and lower limbs.
Cervical plain X-ray anteroposterior and lateral views revealed a long neck in all patients (100%), with seven visible cervical vertebrae, including the first, second, +/- third dorsal vertebrae in the lateral view (
Fig. 1). The anteroposterior view revealed no cervical rib or other detectable abnormality. Straightening of the normal lordosis was noted in the X-ray of 108 patients (81.2%) at the time of presentation.
Normal MRI findings were obtained for all of the patients, excluding any vertebral or cervical cord pathology as a cause of their shoulder pain. Furthermore, muscle enzymes were normal in all patients, which in addition to the normal clinical and EMG findings, excluded the possibility of muscle disease.
The following were recorded for all patients:
Lower normal values of sensory NCS of the ulnar, median, medial/lateral antebrachial, axillary, and musculocutaneous nerves, while the amplitude of the sensory nerve action potential was low in 114 patients.
Normal motor and sensory distal latencies and motor conduction velocities of the ulnar, median, medial/lateral ante-brachial, axillary, and musculocutaneous nerves.
Normal M-wave amplitudes of the axillary, musculocutaneous, ulnar and median nerves.
Normal F-wave latency.
NCS were performed for the right or left sural, tibial, and peroneal nerves in 62 patients (47%), yielding normal results. These studies were performed to exclude peripheral polyneuropathic disorder, although none of the patients showed any symptom or sign suggestive of the condition.
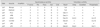
A mild-to-moderate or moderate denervation EMG pattern (
Table 3) was detected. The MUP analysis revealed a reduced number of MUPs of high amplitude and normal duration in 92 patients (69.7%), while in 40 patients (30.3%) there was an increase in the firing of single MUPs. Both EMG changes were noted in 19 patients (14.4%). A denervation EMG pattern was seen in the abductor digiti minimi, first dorsal interosseous, flexor carpi ulnaris, extensor carpi radialis, and triceps brachii muscles in 119 patients (90.2%), while the abductor pollicis brevis muscle was denervated in 102 patients (77.3%). All of the patients exhibited a denervation EMG pattern of the lower cervical paraspinal muscles.
Active neurogenic processes in the form of fibrillation and/or fasciculation potentials were detected while the examined muscle was at rest in 25 patients (19%). Upper cervical paraspinal, deltoid, biceps, and supraspinatus muscle EMG data were normal in all of the patients. The EMG findings were seen only in the muscles of the affected upper limb (which correlated with the clinical symptoms).
After completion of the physiotherapeutic exercise, EMG was performed for 37 patients, of which 14 showed normal EMG patterns of previously affected muscles (i.e., complete recovery of the EMG pattern), 18 exhibited partial improvement of the denervation EMG pattern, and 5 exhibited no EMG pattern of recovery of the affected muscles.
In the physiotherapy exercise, 84 patients (63.6%) were reported to have pain reduction of seven or more points; 33 patients (25%) showed pain improvement of 4 to 5 points, 12 (9%) patients has improved by 3 points, while 3 (2.3%) patients reported no improvement at the end of the physiotherapy.
After completion of the exercise, it was obvious by clinical examination that the neck muscles, and particularly the trapezius muscle, had increased in size, with visible partial correction of the dropped shoulder. The cervical X-ray was repeated after the 12-18 weeks of physiotherapeutic exercise in 60 patients, with satisfactory improvement. The straightening of the normal lordosis had disappeared in 49 of the patients (81.7%). The lateral view of 51 patients (85%) revealed 6 or 7 cervical vertebrae. In the remaining nine patients (15%), the cervical X-ray revealed no radiological improvement, although the patients themselves did report satisfactory improvements. Numbness and tingling sensations disappeared in 110 of the patients (81.5%) who had experienced these sensory symptoms before commencement of the exercise.
There was no shoulder pain in any of the control group patients; the results of a physical examination were normal with no visible shoulder drop. All of these subjects had normal plain cervical X-ray findings. EMG and NCS findings were normal in the 21 examined subjects (the remaining 9 subjects did not consent to EMG and NCS). In these normal subjects, the physiotherapy exercise caused no detectable effect (sensory, motor, or any other).
Discussion
In all of the patients in this study, a history of shooting pain and other related symptoms was associated with cervical radiculopathic disorder.
9,
10 A diagnosis of dropped shoulder causing lower cervical radiculopathy is based on a visually detectable dropped shoulder and is supported by two investigational findings. A lateral view X-ray of the cervical region showing eight or more vertebrae indicates a physical postural abnormality of the shoulder. Normally, the lateral view shows six or seven cervical vertebrae, with the first two thoracic vertebrae being overshadowed by the shoulder. Therefore, when the first thoracic vertebra or both the first and second thoracic vertebrae appear clearly on the lateral view of a plain X-ray of the cervical region, it means that the shoulder is physically dropped down. The prevalence of eight or more vertebrae visible on lateral view cervical X-ray in the general Yemeni population needs to be investigated to evaluate whether people with such an abnormal X-ray present with any physical symptoms.
The EMG changes noted in the patients reviewed in this article document the effect that postural abnormality of the shoulder has on the lower cervical roots (C7 and C8), and T1. This denervation EMG pattern proves the underlying neurogenic effect of DSS.
The EMG changes seen could suggest lower cervical radiculopathy or neurogenic thoracic outlet syndrome (TOS). Exclusion of neurogenic TOS was based upon the following factors:
The clinical presentation of shoulder pain and its radiation to the ipsilateral scapular region and lateral and anterior chest wall, which is not seen in neurogenic TOS.
The normal NCS, normal M-wave amplitude, and normal medial antebrachial response render neurogenic TOS highly unlikely.
Normal interscaline MRI with no sign of brachial plexus affection.
Three major criteria are used for diagnosing DSS:
Shoulder pain that radiates to the surrounding regions (the neck, the corresponding scapular region, lateral and anterior chest wall, and the corresponding upper limb down to the hand).
Lateral view of a plain cervical X-ray showing eight or more vertebrae (the first, second, and -rarely-the third dorsal vertebrae).
A denervation EMG pattern for the muscles supplied by the lower cervical roots (C7, C8, and T1 roots).
The presentation of unilateral shoulder pain in most cases of DSS could be attributable to postural reasons. Yemeni peo-ple usually spend 3-4 hours per day in the sitting position while bending laterally on the right or left elbow, while chewing Qat (the leaves of a plant that contain amphetamine-like substances). This prolonged abnormal postural position could trigger the suggested mechanism of DSS.
One suggested cause of DSS is weakness and/or long neck muscles that elevate the shoulder (trapezius, sternocleidomastoid, and levator scapulae muscles). The mechanical muscular traction of the longstanding dropped shoulder on the muscles of the neck will result in muscular stretching, which causes a compression of the lower cervical roots as they pass through the neck muscles before forming the brachial plexus. Simply put, the stretched neck muscles will compress the lower cervical roots, causing the described symptoms and physical signs.
The lower cervical roots (C5-C8) that form the brachial plexus are contained within the posterior triangle of the neck. The posterior triangle contains the anterior scalene, middle scalene, posterior scalene, and levator scapulae muscles.
15 Spasm of these muscles contributes to the compression effect imposed on the lower cervical roots. The upper cervical roots (C1-C4) are not significantly affected by neck muscle spasm, since these roots are not included in the posterior triangle and are situated higher in the neck in front of levator scapulae and middle scalene muscles.
15
This theory of DSS has been validated in the present study by the positive response of the patients to physiotherapeutic exercises. After performing the exercise for 12-18 weeks to st-rengthen the muscles that lift the shoulder upward, most of the patients (i.e., 117/132, 88.6%) demonstrated a satisfactory improvement. This indicates a physical correction of the dropped shoulder, thus helping to reduce the traction effect upon the cervical muscles. It is thought that DSS is a major cause of lower cervical radiculopathy in Yemeni patients who present with shoulder pain, and had been investigated, with negative results, for other causes of shoulder pain.
An epidemiological study is recommended to study the prevalence of DSS in the Yemeni population, and the female preponderance of DSS. A sex-linked genetic factor may be the cause of this preponderance. A genetic study of the affected patients is suggested to prove/disprove this hypothesis.
The question as to whether DSS also presents in non-Yemeni populations may be answered by conducting further studies comprising people of different nationalities.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download