Abstract
Background
An orbital pseudotumor typically presents with periorbital pain, cranial nerve palsies and proptosis. Although visual deterioration is not unexpected in this pathology, its presentation solely with visual loss is unusual.
Case Report
In this short report, we summarize a case of orbital pseudotumor which presented solely with a decrease in visual acuity, and discuss the clinical and radiological findings.
Conclusions
This atypical presentation likely resulted from the orbital pseudotumor originating in the optic foramen, leaving the neurovascular structures of the superior orbital fissure untouched initially. In the early clinical period, an orbital pseudotumor may manifest itself solely by visual loss. It should therefore be included in the differential diagnosis of visual pathologies-even in the absence of orbital pain and symptoms related to ocular movements.
The term orbital pseudotumor has been used to describe a set of orbital lesions composed of benign nonspecific idiopathic inflammatory infiltrates, characterized by an accumulation of heterogeneous cellular constituents, and with varying degrees of fibrosis.1
Extra-orbital extension through orbital fissures and optic foramina is not unknown.2,3 In the absence of other systemic causes such as sarcoidosis, infectious diseases and hyperthyroidism, inflammatory infiltration with various cellular components and fibrous proliferation is the main feature of this localized pathology. Orbital pain with or without restrictive external ophthalmoplegia is generally an earlier clinical finding than proptosis and visual loss. Even though visual deterioration is not unexpected in this pathology, to the authors' knowledge, presentation solely with visual loss is unusual. This report gives an account of an orbital pseudotumor originating in the optic foramen with an initial symptom of visual loss manifesting itself before the typical clinical presentation of ophthalmoplegia.
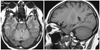
A 62-year old female was admitted to the clinic with a history of a slight decrease in visual acuity in the right eye over the previous four months. The patient had been diagnosed with bilateral cataracts in an ophthalmologic center. Fundus examination and radiological investigations, including cranial magnetic resonance imaging (MRI) without contrast media and fundus fluorescein angiography, were evaluated as normal. For the previous five days, the patient had been experiencing right orbital pain and rapid deterioration in visual acuity in the right eye. Physical examination yielded ptosis, proptosis, failure of ocular movement and only slight light perception in the right orbit. When the previous cranial MRI scans without contrast media were carefully re-analyzed, a small mass lesion in the right optic foramen was noticed (Fig. 1). The mass was iso-intense in fluid attenuated inversion recovery and T1-weighted MRI scans. Orbital MRI scans were immediately performed and a significantly larger retrobulbar orbital mass was observed as being iso-intense on T1-weighted MRI scans and strongly enhanced after contrast injection (Fig. 2). Corticosteroid therapy was started immediately and fine needle aspiration biopsy was performed. Histopathological examination yielded areas of polymorphous infiltration with inflammatory cells and perivascular infiltration with plasma cells in fibrous stroma. No systemic inflammatory or malignant disease was found in a clinical evaluation of the patient. Within the first week of corticosteroid therapy, ptosis in the right eye disappeared and proptosis diminished. At one-month follow-up, globe movement was normal but there was no perception of light. Corticosteroid therapy was continued for 3 months. MRI scans at the ninth month revealed that the mass had decreased in size and, interestingly, did not enhance after contrast injection. The patient is still free of additional symptoms at follow-up in the fifth year.
In contrast to the first description of this pathology by Birch-Hirschfield in 19054 as including all orbital masses apart from neoplasm, the term orbital pseudotumor is currently used to refer to non-specific idiopathic inflammation of the orbit without known systemic etiology. This definition does not, however, summarize common clinical, therapeutical and anatomical characteristics. Clinical course (insidious, acute, relapsing), response to different therapeutic approaches (corticosteroids, immunosuppressive agents, radiation therapy, surgery) and intraorbital locations (any orbital structure or multifocal) vary from case to case in the literature.2,3,5,6
Our patient had two notable characteristics. The first was the insidious onset of visual loss in the right eye before the major attack, which was most probably due to the mass originating in the vicinity of the optic foramen, leaving the neurovascular structures of the superior orbital fissure initially untouched. This is supported by normal fundus fluorescein angiography and a small mass lesion in the right optic foramen seen in the cranial MRI done several months before the acute onset of the disease. Cataract was not likely the reason of the patient's visual complaint in the right eye since there were bilateral cataracts in this patient. Although the posterior location of an orbital pseudotumor has previously been mentioned as more likely to be related to optic nerve involvement,7 visual disturbance has not to our knowledge previously been mentioned as a sole initial finding in this pathology.
The second was the significant decrease in the lesion's uptake contrast material at the nine-month check-up MRI, which meant a tumoral mass lesion was unlikely. A satisfactory therapeutic consensus is lacking for this pathology. The use of different therapeutic measures, with varying degrees of success, have been reported, including surgery, corticosteroid therapy, immunosuppressive agents, and radiotherapy. Some authors have noted that symptom relief should be the therapeutic goal despite incomplete resolution of disease radiologically.8,9
Idiopathic inflammatory pseudotumors of the orbit and idiopathic cavernous sinus inflammation or Tolosa-Hunt syndrome (THS) resemble each other. We have previously reported that periorbital pain, cranial nerve palsies, identical signal intensity in neuroimaging, and dramatic response to corticosteroid therapy are common features of pseudotumors of the orbit and THS.10 The only difference seems to be the exact original site of these lesions, which occur in adjacent neuroanatomical structures. In agreement with some other authors, we are of the opinion that orbital pseudotumors and idiopathic cavernous sinus inflammation (THS) may develop from the same pathological origin.3,10
Figures and Tables
References
1. Hogan RN. Levin LA, Arnold AC, editors. Orbital inflammation and infection. Neuro-ophthalmology the Practical Guide. 2005. New York: Thieme Medical Publishers Inc;356–386.
2. Mahr MA, Salomao DR, Garrity JA. Inflammatory orbital pseudotumor with extension beyond the orbit. Am J Ophthalmol. 2004. 138:396–400.

3. Wasmeier C, Pfadenhauer K, Rösler A. Idiopathic inflammatory pseudotumor of the orbit and Tolosa-Hunt syndrome--are they the same disease? J Neurol. 2002. 249:1237–1241.

4. Birch-Hirschfeld A. Zur Diagnostik und Pathologie der Orbitaltumoren. Ber Dtsch Ophthal Ges. 1905. 32:127–135.
5. Abramovitz JN, Kasdon DL, Sutula F, Post KD, Chong FK. Sclerosing orbital pseudotumor. Neurosurgery. 1983. 12:463–468.

6. Reittner P, Riepl T, Goritschnig T, Preidler KW, Koele W, Szolar DH. Bilateral orbital pseudotumour due to Ormond's disease: MR imaging and CT findings. Neuroradiology. 2002. 44:272–274.

7. Nugent RA, Rootman J, Robertson WD, Lapointe JS, Harrison PB. Acute orbital pseudotumors: classification and CT features. AJR Am J Roentgenol. 1981. 137:957–962.

8. McNicholas MM, Power WJ, Griffin JF. Idiopathic inflammatory pseudotumour of the orbit: CT features correlated with clinical outcome. Clin Radiol. 1991. 44:3–7.

9. Hurwitz BS, Citrin CM. Use of computerized axial tomography (CAT scan) in evaluating therapy of orbital pseudotumor. Ann Ophthalmol. 1979. 11:217–221.
10. Turkoglu R, Balak N, Tireli H. Surgery With Cavernous Sinus Syndrome. A Clinical Study and Review of the Tolosa-Hunt Syndrome. Neurosurg Q. 2008. 18:230–238.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download