Abstract
Background and Purpose
The progression of migraine into chronic daily headache involves multiple risk factors, but the main contributor is not known. Glutamate is the major excitatory neurotransmitter in central sensitization, which is an important process in the pathogenesis of migraine transformation. The glutamate transporter protein excitatory amino acid transporter 2 (EAAT2) is the primary modulator of glutamatergic neurotransmission, and genetic polymorphisms of its gene, EEAT2, have been identified. The aim of this study was to determine the effect of EAAT2 polymorphisms on migraine transformation into chronic daily headache.
Methods
We included 74 migraine patients with episodic attack (M-E) and 59 migraine patients with chronic daily headache (M-CDH). After amplifying EAAT2 by polymerase chain reaction, we assessed its genotype frequencies based on restriction fragment length polymorphisms. We reclassified all migraine patients into two groups according to their EAAT2 genotype, either with the A allele (n=62) or without it (n=71), and compared the clinical variables between the two groups.
Results
The genotype frequencies of EAAT2 polymorphisms did not differ between the M-E and M-CDH groups. Comparison between EEAT2 genotypes revealed that the frequency of analgesic usage was significantly higher among migraine patients with the A allele (12.9±1.6 days/month) than in those without the A allele (8.1±1.2 days/month; p=0.019). The other clinical variables of migraine did not differ between the two groups.
Most patients with chronic daily headache have a history of episodic migraine that has gradually evolved into the chronic form. This gradual transformation during the most productive years of adulthood leads to profound disability, which is costly to the public health system.1,2 The process of migraine transformation is complex and involves multiple risk factors, but the main contributor is not known.3,4 Previous studies have found that genetic factors and familial clustering affect the development of chronic tension-type headache; however, few studies have analyzed in detail the role of genetic factors in the transformation of migraine into chronic daily headache.5-7
The progression of migraine is postulated to result from changes in nociceptive thresholds and the ensuing central sensitization caused by recurrent migraine in susceptible individuals.8 It is well known that glutamate is released from the trigeminal ganglion along with calcitonin gene-related peptide, activating the central nervous system structure involved in migraine pathophysiology.9,10 Central sensitization following peripheral sensory stimulation is mediated by glutamate receptor activation.11 There is evidence from animal studies that increased glutamate levels parallel enlargement in the sensory thresholds of facial receptive fields,12 thus further supporting the involvement of glutamate in the development of cutaneous allodynia, as observed in migraineurs. Glutamate levels in the cerebrospinal fluid are significantly elevated in patients with chronic migraine as compared to those in control subjects.13,14
Excitatory amino acid transporters (EAATs) play a key role in the regulation of glutamate levels in the central nervous system.15 EAATs transport glutamate into astrocytes for conversion into glutamine, which is then released and recycled by neurons to generate glutamate.16 Thus far, five human EAATs have been cloned,15,17 among which excitatory amino acid transporter 2 (EAAT2) is responsible for up to 90% of all glutamate transport.18 The human EAAT2 gene is located on 11q13-13, and polymorphisms in the EAAT2 promoter affect the putative regulatory site for activator protein-2 and create different transcriptional efficiencies.19,20 Therefore, differences in genotype could be associated with differential glutamate neurotransmission. The potential roles of the functional polymorphisms of the glutamate transporter protein in various neurological disorders, such as multiple sclerosis, amyotrophic lateral sclerosis, and epilepsy, have been the subject of several studies.21-23 A mutation of EAAT1 reportedly causes a decline in glutamate uptake in patients with hemiplegic migraine and episodic ataxia.24 However, no studies have examined the association between EAAT2 polymorphisms and migraine.
The aim of the present study was to elucidate the contribution of glutamate transporter protein polymorphism in the transformation of migraine into chronic daily headache.
All of the subjects included in this study were identified from a larger pool of subjects taking part in an ongoing prospective study of the genetic basis of headache at the Headache Clinic of the Catholic University of Korea. We recruited 133 consecutive patients with migraine from the Headache Clinic. None of the participants were from the same family. Given the known effects of gender on the gene system, only women were included in this study. The subjects were patients diagnosed with migraine or chronic migraine who had not taken preventive medications for headache. This study was approved by the institutional ethical committee of our institute, and written informed consent to participate was obtained from all included subjects.
All of the participants were clinically assessed and examined physically and neurologically by an experienced neurologist. During the interview, detailed data were obtained regarding their clinical symptoms, headache variables and analgesics that were taken for abortive treatment for their headaches using a diary composed of structured questionnaires. We classified migraine patients who suffer from headaches for less than 15 days/month as having episodic migraine (M-E; n=74), and those who suffer from headaches for 15 days/month or more as having migraine with chronic daily headache (M-CDH; n=59). The M-CDH group included patients with chronic migraine, probable chronic migraine with medication overuse, and migraine combined with other types of headache. Migraine was diagnosed according to the International Classification of Headache Disorders, 2nd edition.25
Blood samples were collected into heparinized tubes and stored at -80℃ before isolation of DNA. Genomic DNA was isolated and amplified by polymerase chain reaction (PCR) using the specific oligonucleotide primers 5'-GAG CGG CGG GGC CTC TTT TC-3' and 5'-TGC AGC CGC TGC CAC CTG TG-3'. PCR reaction mixtures contained 50 ng of genomic DNA, 20 pmol of each primer, 10 mM Tris-HCl, 50 mM KCl, 1.5 mM MgCl2, each of dATP, dCTP, dGTP, and dTTP at 200 µM, and 1.25 units of Taq polymerase in a total volume of 50 µL (Promega, Wisconsin, USA). The following cycling conditions were used: 1) an initial denaturation at 95℃ for 5 min; 2) 35 cycles of denaturation at 95℃ for 1 min, annealing at 57℃ for 1 min, and extension at 72℃ for 1 min; and 3) a final extension at 72℃ for 3 min. PCR was conducted in a thermal cycler (Bio-Rad, California, USA). The resulting PCR products were subjected to restriction digestion overnight at 37℃ using 5 units of BcnI (Takara Bio, Shiga, Japan). The digested products were separated at 100 V for 40 min on a 2% agarose gel (Bio-Rad) containing 10 mg/mL ethidium bromide. The gel was visualized under ultraviolet light using a gel electrophoresis visualization system (Spectroline, New York, USA). The A allele gave 381-bp fragments and the C allele gave 262- and 119-bp fragments. Genotyping was based on the independent scoring of the results by two reviewers who were blinded to the case/control status.
We classified all migraine patients according to their EAAT2 genotype: individuals with the A allele (n=62; A/A and A/C genotypes) or individuals without the A allele (n=71; C/C genotype). The following clinical variables of headache were compared between the two groups: pain index of headache intensity, as measured on a visual analog scale; headache frequency (days/month); duration of each headache attack (hours per attack); and frequency of analgesic use for headache (days/month) during the previous 6 months.
Comparisons of genotype distribution between the M-E and M-CDH groups were performed on raw frequencies using the χ2 test. A χ2 analysis of the Hardy-Weinberg equilibrium for the genotypes was conducted to determine whether the allele frequencies were stable. For the comparisons of clinical variables of migraine headache according to EAAT2 polymorphism, we used a t-test for parametric continuous variables. SPSS statistical software (version 10.0; SSPS, IL, USA) was used in all analyses, and the level of statistical significance was set at p<0.05.
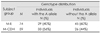
The genotype distributions in patients with migraine did not deviate from that expected based on Hardy-Weinberg equilibrium. The genotype frequencies for the EAAT2 promoter polymorphism did not differ significantly between the M-E and M-CDH groups (Table 1). The frequency of analgesics usage was higher among migraine patients with the A allele (Table 2): 12.9 and 8.1 days/month in migraine patients with and without the A allele, respectively (p=0.019). The clinical variables of migraine including headache frequency, duration of headache attack, and headache intensity did not differ significantly between the two groups (Table 2).
Recent advances have shed light on the pathogenic mechanisms of migraine transformation, and glutamate-mediated excitatory pathways are one of the putative candidates in the development and maintenance of chronic headache through the action of glutamate on ionotropic and metabotropic receptors.26,27 The transformation of episodic migraine into chronic daily headache changes characteristics such as the frequency and intensity of the headaches.
The present study was initially designed to evaluate the role of polymorphism of EAAT2, a genetic component related to glutamate metabolism, in the transformation of migraine into chronic daily headache. However, the genotype distribution of EAAT2 polymorphisms did not differ between M-E and M-CDH. Moreover, we found no difference in the frequency of headache attack, which is one of the most important requisites for the diagnosis of chronic migraine. The pain intensity and duration of migraine attack also did not differ between the two EAAT2 genotypes. On the basis of these results, we could not confirm whether the genetic factor associated with EAAT2 polymorphism plays a contributory role in the transformation of migraine into chronic daily headache through the enhancement of pain generation or a perception mechanism. The glutamatergic system is regulated in a complicated manner, and so it is possible that factors other than EAAT2 polymorphism play a role in this process of transformation. Further studies are needed to investigate the potential function of these factors in migraine transformation.
The present study identified differences in the pattern of analgesic usage for migraine attack according to EAAT2 polymorphism. It is well known that frequent use of analgesics results in medication overuse in primary headache, which has been regarded as a causative factor for the transformation into chronic daily headache.28,29 In the pathophysiology of medication-overuse and transformed migraines, there is considerable overlap in the mechanisms mediating migraine headache pain and analgesic-induced paradoxical pain. The chronic administration of morphine has been found to increase the expression of calcitonin gene-related peptide and central changes in primary afferent neurons, enhance descending facilitation, and increase excitatory neurotransmission.30,31 Results from studies using specialized magnetic resonance imaging techniques showed high iron levels due to analgesic overuse in the midbrain periaqueductal gray of patients with chronic daily headache. The degree of iron load was correlated with the duration of analgesic use. Dysfunction in the periaqueductal gray due to frequent analgesic use results in medication-overuse headache in migraine patients, as this region is the center of a descending antinociceptive neuronal network.32
While medication overuse and chronic migraine are linked, the actual causal path-that is whether analgesics overuse is a cause or consequence of pain progression-is still a matter of debate. In the present study, EAAT2 polymorphism influenced the pattern of analgesic usage without affecting the headache characteristics, which suggests an independent role of analgesics overuse in migraine transformation.
Analgesics overuse has long been considered a "biobehavioral" disorder, in which the biological predisposition to develop a chronic daily headache interacts with the behavior of an individual who is prone to develop a dependence disorder.33,34 A genetic association study found that about one-third of patients with analgesic-overuse headache had a family history of drug or substance abuse.6 Likewise, Ferrari et al.35 found that drug abuse was significantly higher among the first-degree relatives of chronic migraine patients than among those of episodic migraine patients. A genetic predisposition to drug abuse has been traced to polymorphisms in neurotransmitter, which is implicated in migraine pathogenesis.6,7 Although no study has shown a direct relationship between analgesic overuse and EAAT2 polymorphism, a few genetic association studies have found that it might be associated with predisposition to alcohol dependence and the personality trait related to compulsive substance-seeking behavior.36
Inadequately treated headache or pain remains a major challenge in pain therapy, and it can lead patients to further analgesic use. It has been reported that the variable success rates of pharmacologic therapy may be related to the different polymorphisms of various genetic dispositions in patients who respond to analgesics.37,38 Genetic variants may alter the pharmacodynamic mechanisms controlling the interaction between the analgesic molecules and their target structures.39 In chronic migraine, analysis of the association between genetic polymorphism and grade of response to triptan administration showed a significant correlation.40,41 These results could be part of an integrated platform for evaluating genetic influences in drug metabolism and medication overuse in chronic migraine patients.
In summary, the results of the present study have revealed that EAAT2 polymorphism (a genetic component related to glutamate metabolism) influences analgesic overuse in patients with migraine. Although our results do not indicate a direct association between this genetic factor and chronic migraine, we suggest a genetic influence on migraine transformation throughout the development of medication-overuse headache. Familial aggregation studies and large genetic epidemiological surveys are needed to confirm these results.
References
1. Mathew NT, Stubits E, Nigam MP. Transformation of episodic migraine into daily headache: analysis of factors. Headache. 1982. 22:66–68.

3. Zwart JA, Dyb G, Hagen K, Svebak S, Holmen J. Analgesic use: a predictor of chronic pain and medication overuse headache: the Head-HUNT Study. Neurology. 2003. 61:160–164.

4. Lipton RB, Bigal ME. Chronic daily headache: is analgesic overuse a cause or a consequence? Neurology. 2003. 61:154–155.

5. Russell MB, Ostergaard S, Bendtsen L, Olesen J. Familial occurrence of chronic tension-type headache. Cephalalgia. 1999. 19:207–210.

6. Cevoli S, Mochi M, Scapoli C, Marzocchi N, Pierangeli G, Pini LA, et al. A genetic association study of dopamine metabolism-related genes and chronic headache with drug abuse. Eur J Neurol. 2006. 13:1009–1013.

7. Park JW, Kim JS, Kim YI, Lee KS. Serotonergic activity contributes to analgesic overuse in chronic tension-type headache. Headache. 2005. 45:1229–1235.

8. Aurora SK. Spectrum of illness: understanding biological patterns and relationships in chronic migraine. Neurology. 2009. 72:S8–S13.

9. Hill RG, Salt TE. An ionophoretic study of the responses of rat caudal trigeminal nucleus neurones to non-noxious mechanical sensory stimuli. J Physiol. 1982. 327:65–78.

10. Xiao Y, Richter JA, Hurley JH. Release of glutamate and CGRP from trigeminal ganglion neurons: role of calcium channels and 5-HT1 receptor signaling. Mol Pain. 2008. 4:12.

11. Vikelis M, Mitsikostas DD. The role of glutamate and its receptors in migraine. CNS Neurol Disord Drug Targets. 2007. 6:251–257.

12. Oshinsky ML, Luo J. Neurochemistry of trigeminal activation in an animal model of migraine. Headache. 2006. 46:Suppl 1. S39–S44.

13. Vieira DS, Naffah-Mazzacoratti Mda G, Zukerman E, Senne Soares CA, Cavalheiro EA, Peres MF. Glutamate levels in cerebrospinal fluid and triptans overuse in chronic migraine. Headache. 2007. 47:842–847.

14. Peres MF, Zukerman E, Senne Soares CA, Alonso EO, Santos BF, Faulhaber MH. Cerebrospinal fluid glutamate levels in chronic migraine. Cephalalgia. 2004. 24:735–739.

16. Lauriat TL, McInnes LA. EAAT2 regulation and splicing: relevance to psychiatric and neurological disorders. Mol Psychiatry. 2007. 12:1065–1078.

17. Arriza JL, Fairman WA, Wadiche JI, Murdoch GH, Kavanaugh MP, Amara SG. Functional comparisons of three glutamate transporter subtypes cloned from human motor cortex. J Neurosci. 1994. 14:5559–5569.

18. Lizasoain I, Cárdenas A, Hurtado O, Romera C, Mallolas J, Lorenzo P, et al. Targets of cytoprotection in acute ischemic stroke: present and future. Cerebrovasc Dis. 2006. 21:Suppl 2. 1–8.

19. Meyer T, Ludolph AC, Morkel M, Hagemeier C, Speer A. Genomic organization of the human excitatory amino acid transporter gene GLT-1. Neuroreport. 1997. 8:775–777.

20. Mallolas J, Hurtado O, Castellanos M, Blanco M, Sobrino T, Serena J, et al. A polymorphism in the EAAT2 promoter is associated with higher glutamate concentrations and higher frequency of progressing stroke. J Exp Med. 2006. 203:711–717.

21. Pampliega O, Domercq M, Villoslada P, Sepulcre J, Rodríguez-Antigüedad A, Matute C. Association of an EAAT2 polymorphism with higher glutamate concentration in relapsing multiple sclerosis. J Neuroimmunol. 2008. 195:194–198.

22. Jackson M, Steers G, Leigh PN, Morrison KE. Polymorphisms in the glutamate transporter gene EAAT2 in European ALS patients. J Neurol. 1999. 246:1140–1144.

23. Sander T, Berlin W, Ostapowicz A, Samochowiec J, Gscheidel N, Hoehe MR. Variation of the genes encoding the human glutamate EAAT2, serotonin and dopamine transporters and Susceptibility to idiopathic generalized epilepsy. Epilepsy Res. 2000. 41:75–81.

24. Jen JC, Wan J, Palos TP, Howard BD, Baloh RW. Mutation in the glutamate transporter EAAT1 causes episodic ataxia, hemiplegia, and seizures. Neurology. 2005. 65:529–534.

25. [The International Classification of Headache Disorders: 2nd edition]. Neurol Neurochir Pol. 2006. 40:S7–S41.
26. Baranauskas G, Nistri A. Sensitization of pain pathways in the spinal cord: cellular mechanisms. Prog Neurobiol. 1998. 54:349–365.

28. Dodick DW. Review of comorbidities and risk factors for the development of migraine complications (infarct and chronic migraine). Cephalalgia. 2009. 29:Suppl 3. 7–14.

29. Bigal ME, Lipton RB. Modifiable risk factors for migraine progression. Headache. 2006. 46:1334–1343.

30. Filatova E, Latysheva N, Kurenkov A. Evidence of persistent central sensitization in chronic headaches: a multi-method study. J Headache Pain. 2008. 9:295–300.

31. Boes CJ, Black DF, Dodick DW. Pathophysiology and management of transformed migraine and medication overuse headache. Semin Neurol. 2006. 26:232–241.

32. Heinricher MM, Tavares I, Leith JL, Lumb BM. Descending control of nociception: specificity, recruitment and plasticity. Brain Res Rev. 2009. 60:214–225.

33. Lake AE 3rd. Medication overuse headache: biobehavioral issues and solutions. Headache. 2006. 46:Suppl 3. S88–S97.

34. Saper JR, Hamel RL, Lake AE 3rd. Medication overuse headache (MOH) is a biobehavioural disorder. Cephalalgia. 2005. 25:545–546.

35. Ferrari A, Leone S, Vergoni AV, Bertolini A, Sances G, Coccia CP, et al. Similarities and differences between chronic migraine and episodic migraine. Headache. 2007. 47:65–72.

36. Matsumoto Y, Suzuki A, Ishii G, Oshino S, Otani K, Goto K. The -181 A/C polymorphism in the excitatory amino acid transporter-2 gene promoter affects the personality trait of reward dependence in healthy subjects. Neurosci Lett. 2007. 427:99–102.

37. Lötsch J, Geisslinger G, Tegeder I. Genetic modulation of the pharmacological treatment of pain. Pharmacol Ther. 2009. 124:168–184.

38. Kosek E, Jensen KB, Lonsdorf TB, Schalling M, Ingvar M. Genetic variation in the serotonin transporter gene (5-HTTLPR, rs25531) influences the analgesic response to the short acting opioid Remifentanil in humans. Mol Pain. 2009. 5:37.

39. Oertel B, Lötsch J. Genetic mutations that prevent pain: implications for future pain medication. Pharmacogenomics. 2008. 9:179–194.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download