Abstract
Background and Purpose
Frovatriptan is a selective 5-HT1B/1D agonist with a long duration of action and a low incidence of side effects. Although several placebo-controlled trials have documented the clinical efficacy and safety of frovatriptan in adults with migraine, this drug has not previously been studied in Asian including Korean patients.
Methods
In this double-blind multicenter trial, 229 patients with migraine were randomized to receive frovatriptan 2.5 mg or placebo upon the occurrence of a moderate-to-severe migraine. The primary outcome was the 2-hour headache response rate.
Results
Frovatriptan significantly increased the 2-hour headache response rate compared with placebo (52.9% vs. 34.0%, p=0.004). The headache response rates at 4, 6, and 12 hours were significantly higher in the frovatriptan group than in the placebo group, as was the pain-free rate at 2 hours (19.0% vs. 5.7%, p=0.004), 4 hours (40.7% vs. 23.0%, p=0.006), and 6 hours (56.1% vs. 34.0%, p=0.002). The median time to a headache response was significantly shorter in the frovatriptan group than in the placebo group (2.00 hours vs. 3.50 hours, p<0.001). The use of rescue medications was more common in the placebo group (p=0.005). Chest tightness associated with triptan was infrequent (2.5%), mild, and transient.
Sumatriptan, the first commercially available triptan drug, has had a significant clinical impact on the acute treatment of migraine. Although used for decades as a standard treatment for acute migraine, sumatriptan has several limitations, including unexpected low efficacy, recurrent headache caused by its short half-life, and intolerable adverse effects (AEs).1,2 The newer triptans, including frovatriptan, were developed to improve the clinical efficacy and reduce AEs. Compared with sumatriptan, frovatriptan has a fivefold greater affinity for serotonin 5-HT1B/1D receptors, a superior functional selectivity for cerebral arteries than coronary arteries,3 and an approximately tenfold longer half-life (25 hours),4 suggesting that frovatriptan offers greater efficacy, a lower recurrence rate, and more tolerability than other 5-HT1B/1D agonists.
Data regarding the efficacy and safety of triptans in Asian migraine patients are limited, but several clinical trials have shown that Asians exhibit different results for the mitochondrial polymorphism (A11084G), different pharmacokinetics and pharmacodynamic profiles, greater placebo effects, and higher incidences of AEs than Caucasian patients.5-9 These findings indicate that the relatively low preference for triptans in Asian populations may be partially related to their relative sensitivity to the AEs of these drugs.
Frovatriptan has been shown to be effective in the acute management of migraine4,10,11 and in the management of menstrual migraine.12 However, all previous trials of frovatriptan were conducted primarily in Western countries, with no systematic studies performed in Asian countries, including Korea. We therefore designed this clinical trial to assess the efficacy, tolerability, and safety of frovatriptan in Korean migraine patients.
The primary hypothesis was that frovatriptan would provide greater migraine relief than placebo. The secondary hypothesis was that the AE profile of frovatriptan would be similar to that of placebo.
Eligible patients were men and women, aged 18 to 65 years, with a history of migraine with or without aura for at least 12 months, as defined by the International Classification of Headache Disorders-II (ICHD-II) criteria.13 All patients had experienced one to eight moderate-to-severe migraine episodes per month for at least two consecutive months prior to enrollment.
Exclusion criteria were 1) a history of basilar, ophthalmoplegic, or hemiplegic migraine, 2) >15 headache days per month prior to screening, 3) cerebrovascular, cardiac, hepatic, or renal disease, 4) being pregnant or breast-feeding, 5) a history or current evidence of drug or alcohol abuse, 6) a history of exposure to frovatriptan, 7) treatment with any other investigational compound or device within 30 days of the start of this study, and 8) initial onset of migraine after the age of 50 years.
This double-blind, placebo-controlled, randomized trial was conducted in eight headache centers in Korea from November 2006 to November 2007. All participating investigators were neurologists specializing in headache throughout Korea. This study protocol was reviewed and approved by the Korean Food and Drug Administration (FDA) and the institutional review board of each center. Each patient provided written informed consent prior to study entry. The study was supervised by the Korean FDA in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines.
Treatments were allocated according to a predetermined computer-generated randomization program provided by Statistical Analysis System (SAS). Randomization was in a 1 : 1 ratio of frovatriptan (2.5 mg) to placebo. The block size used was four or six. Eligible patients were assigned sequential randomization numbers upon study entry. Both participants and investigators were blinded to treatment assignment.
After randomization, the patients were given the study medication, rescue medication (ibuprofen), and a diary to record their migraine attacks. Within 12 weeks after randomization, patients were asked to take the study medication when they had a migraine attack of moderate-to-severe intensity and record each such attack in their diary.
Rescue medication (200-mg ibuprofen) was permitted when patients suffered from sustained moderate-to-severe headache for at least 2 hours after taking the study medication or suffered a recurrent migraine headache of moderate-to-severe intensity within 24 hours. No other analgesics or antiemetics were allowed from 6 hours before to 2 hours after taking the study medication. Triptans or ergotamine-containing drugs were also not allowed within 24 hours. Use of the study medication and rescue medication was recorded in the headache diary. Within 48 hours of taking the study medication, patients were to contact their assigned investigators to review the efficacy and AEs of the study medication. Follow-up visits were scheduled within 5 days of the end of the study to allow the subjects to submit headache diaries and return unused medication. Patients who did not take the study medication within 12 weeks from randomization were not included in the analysis.
Patients recorded efficacy and tolerability data in their headache diaries at baseline and at 2, 4, 6, 12, and 24 hours after taking the study medication. Headache severity was assessed according to the International Headache Society (IHS) 4-point rating scale, where 0=absent, 1=mild, 2=moderate, and 3=severe. The primary efficacy outcome measure was the 2-hour headache response rate, defined as the proportion of patients experiencing a change in headache intensity: from moderate or severe at baseline to mild or no pain at 2 hours. The secondary efficacy outcome measures were the headache responses at 4, 6, 12, and 24 hours after taking the study medication, the proportion of patients who were pain free at 2, 4, and 6 hours after taking the study medication, and the time to the first headache response of a mild headache or no headache. Headache recurrence was also evaluated, which was defined as the proportion of patients who had headache relief at 4 hours and whose headache returned to a moderate-to-severe level within 24 hours. The proportion of patients who remained pain free at 24 hours and the use of rescue medication were also measured.
The safety and tolerability of frovatriptan were assessed by performing a full physical examination, laboratory assessments, vital signs, and a 12-lead effect of continuous electrocardiography (ECG) examination. All AEs occurring between dosing and follow-up were recorded on patient diary cards.
Sample size calculations were based on assumed treatment response rates of 27% for placebo and 46% for frovatriptan at the 5% significance level (two-sided) with 80% statistical power.11,14 We calculated that 200 subjects were required, and so based on an estimated 20% dropout rate, we planned to recruit 250 subjects. All efficacy data were analyzed on a full analysis set (FAS), which included all patients who took the study medication and completed at least one efficacy evaluation. Per protocol (PP) analysis was performed after excluding major protocol violators from the FAS population.
The observed data for each time point were used for analysis. Data not recorded in patients' diaries in a timely fashion were not included.
Logistic regression analysis was applied to the 2-hour response rate, and logistic regression models were used for the recurrence rate. The log-rank test was used to compare the time to a headache response and the time to recurrence between the two groups. All statistical tests had a two-sided significance level of 0.05.
A total of 298 patients were randomized to receive treatment with frovatriptan or placebo (Fig. 1). Of these, 229 patients who had taken the study medication at least once due to migraine headache were included in the FAS analysis.
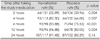
As indicated in Table 1, the baseline characteristics of the participants did not differ significantly between the frovatriptan and placebo groups. Most participants were women (90.39%), and about half (41.48%) had taken triptans for migraine treatment. The baseline headache severity and the median interval between onset and treatment with the study
medication also did not differ significantly between the two groups.
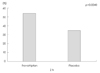
As shown in Fig. 2, the primary endpoint (headache relief at 2 hours after taking the study medication) was reported by 64 of 121 evaluable patients (52.89%) in the frovatriptan group, compared with 36 of 106 patients (33.96%) in the placebo group (p=0.004). Frovatriptan also showed significant superiority over placebo in almost all other outcome measures, including the headache responses at 4, 6, and 12 hours after taking the study medication, the percentage who were pain free for up to 6 hours, sustained headache relief after becoming pain free, time to first headache response, and use of rescue medication (Table 2 and 3). Similar results were seen in the PP population.
Among 159 patients who achieved headache relief after 4 hours, 29 experienced headache recurrence within 24 hours: 16.13% (15/93) in the frovatriptan group and 21.21% (14/66) in the placebo group (p=0.41). Rescue medications were used more frequently in the placebo group than in the frovatriptan group (p=0.005), and they were usually taken between 2 and 4 hours after taking the study medication; 55 of 73 patients (75.34%) took the rescue medication within this time period in the placebo group compared with 39 of 61 (63.93%) in the frovatriptan group.
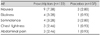
The overall rate of AEs did not differ significantly between the frovatriptan group (38 AEs in 27 subjects; 22.13%) and the placebo group (26 AEs in 14 subjects; 13.08%) (p=0.07). All AEs were transient and had a mild-to-moderate intensity. The most common AE in the frovatriptan group was nausea (7.38%) (Table 4). In contrast, AEs associated with triptan symptoms, including chest tightness, were infrequent (2.46%), mild, and resolved without intervention. No clinically meaningful changes in vital signs, laboratory values, or ECG outcomes were observed.
This was the first randomized, double-blind, placebo-controlled trial to evaluate the efficacy and tolerability of frovatriptan (2.5 mg) in Korean migraineurs. Frovatriptan was significantly more effective in relieving migraine headaches compared with placebo. The headache response rate at 2 hours was 52.89% in the frovatriptan group, which is similar to the findings of earlier trials of frovatriptan.11 The efficacy result in this study was similar to that found in a previous trial of zolmitriptan (2.5 mg) in Korean migraineurs, where the headache response rate at 2 hours was 52.2% in the zolmitriptan group and 30.7% in the placebo group.15 We found that the placebo-subtracted values of the headache response were maintained in about 20% of patients for up to 12 hours, which may be related to the long half-life of frovatriptan.
Frovatriptan has the longest half-life among the triptans, and hence it can be expected to be associated with a low migraine recurrence rate and a long duration of action. Previous trials of frovatriptan have found low 24-hour headache recurrence rates (7% to 19%).7 In contrast, clinical trials of sumatriptan, zolmitriptan, and rizatriptan have all found 24-hour headache recurrence rates of around 30%.16,17 In the present study, the 24-hour headache recurrence was lower in the frovatriptan group (16.13%) than in the placebo group (21.21%), but did not reach significance. A significantly higher proportion of patients in the placebo group took additional analgesics as rescue medications, which may have led to the recurrence rate being an underestimated. More accurate data for the 24-hour headache recurrence requires prohibition of rescue medication during the first 24 hours. However, ethically it is difficult to restrict the use of rescue medications.
Overall, 41.48% of the patients in this trial had previously been exposed to triptans. This high proportion of previous triptan users may be attributed to our strict inclusion criteria, including a history of typical moderate-to-severe migraines of least 12 months. The efficacy of frovatriptan was measured as the headache response rate to single attacks, and the participants were expected to be sufficiently experienced in differentiating typical migraine attacks from other headache syndromes within 2 hours of headache onset. This did not appear to affect the efficacy and tolerability results because there were no differences between triptan-experienced and triptan-naïve patients.
AEs were reported by 22.13% of patients in the frovatriptan group, which is a lower percentage than in previous trials of frovatriptan,10 and lower than in trials of sumatriptan (100 mg) (39.0%)18 and naratriptan (2.5 mg) (38.31%)19 in Korean migraineurs. In particular, the incidence of chest tightness was 2.46% in the frovatriptan group, which is lower than reported for other triptans, including sumatriptan,20 zolmitriptan,21 and rizatriptan.22
Our efficacy outcomes and safety profiles were similar to those found in previous trials in Western countries. Because there is a paucity of data regarding the efficacy of triptans in Asian populations, previous such results may have been attributed to racial differences. Unlike other Asian studies,6,7,23 we did not observe a high placebo effect that could have negatively influenced the relative benefit of triptans. Our application of strict inclusion criteria and the supervision of study coordinators in selecting migraine attack for study medication may have increased the clinical accuracy. Moreover, this study was ultimately subject to approval by the Korean FDA, and the results were stringently evaluated and monitored under its supervision.
This study had several limitations. First, the intraindividual response consistency could not be estimated because efficacy results were based on single doses for single migraine attacks. This limitation may not be problematic due to the consistent results observed among the participating centers and the finding of similar results in previous Western trials of frovatriptan. Second, interindividual variations could not be accessed because this study did not use a crossover design.
In summary, this study demonstrated that frovatriptan (2.5 mg) is a generally effective and well-tolerated treatment for Korean patients with moderate-to-severe migraine.
Figures and Tables
References
1. Ferrari MD, Saxena PR. On serotonin and migraine: a clinical and pharmacological review. Cephalalgia. 1993. 13:151–165.

2. Tfelt-Hansen P, De Vries P, Saxena PR. Triptans in migraine: a comparative review of pharmacology, pharmacokinetics and efficacy. Drugs. 2000. 60:1259–1287.
3. Brown AM, Parsons AA, Raval P, Porter R, Tilford NS, Gager TL, et al. SB 209509 (VML 251), a potent constrictor of rabbit basilar artery with high affinity and selectivity for human 5-HT1D receptors. Br J Pharmacol. 1996. 119:110P.
4. Goldstein J, Keywood C. 251/96/14 Study Group. Frovatriptan for the acute treatment of migraine: a dose-finding study. Headache. 2002. 42:41–48.

5. Kang L, Lee ST, Im W, Kim SC, Hun KS, Kim BK, et al. Screening of the A11084G polymorphism and scanning of a mitochondrial genome SNP in Korean migraineurs. J Clin Neurol. 2007. 3:127–132.

6. Sakai F, Iwata M, Tashiro K, Itoyama Y, Tsuji S, Fukuuchi Y, et al. Zolmitriptan is effective and well tolerated in Japanese patients with migraine: a dose-response study. Cephalalgia. 2002. 22:376–383.

7. Sakai F, Diener HC, Ryan R, Poole P. Eletriptan for the acute treatment of migraine: results of bridging a Japanese study to Western clinical trials. Curr Med Res Opin. 2004. 20:269–277.

8. Shimazawa R, Ando Y, Hidaka S, Saito K, Toyoshima S, Kobayashi F. Development of triptans in Japan: bridging strategy based on the ICH-E5 guideline. J Health Sci. 2006. 52:443–449.

9. Yates RA, Tateno M, Nairn K, Ikegami A, Dane A, Kemp J. The pharmacokinetics of the antimigraine compound zolmitriptan in Japanese and Caucasian subjects. Eur J Clin Pharmacol. 2002. 58:247–252.

10. Rapoport A, Ryan R, Goldstein J, Keywood C. Dose range-finding studies with frovatriptan in the acute treatment of migraine. Headache. 2002. 42:Suppl 2. S74–S83.

11. Ryan R, Géraud G, Goldstein J, Cady R, Keywood C. Clinical efficacy of frovatriptan: placebo-controlled studies. Headache. 2002. 42:Suppl 2. S84–S92.

12. Silberstein SD, Elkind AH, Schreiber C, Keywood C. A randomized trial of frovatriptan for the intermittent prevention of menstrual migraine. Neurology. 2004. 63:261–269.

13. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 2nd edition. Cephalalgia. 2004. 24:Suppl 1. 1–160.
14. Protocol No. 251/96/07 Clinical Study Report. 2002. Vernalis.
15. Lee SB, Kim YI, Choi YB, Chung SW, Yang DW, Lee KS, et al. Double-blind placebo-controlled randomized clinical trial of zolmitriptan in acute treatment of migraine. J Korean Neurol Assoc. 2001. 19:29–35.
16. Havanka H, Dahlöf C, Pop PH, Diener HC, Winter P, Whitehouse H, et al. Naratriptan S2WB2004 Study Group. Efficacy of naratriptan tablets in the acute treatment of migraine: a dose-ranging study. Clin Ther. 2000. 22:970–980.

17. Ferrari MD, Roon KI, Lipton RB, Goadsby PJ. Oral triptans (serotonin 5-HT(1B/1D) agonists) in acute migraine treatment: a meta-analysis of 53 trials. Lancet. 2001. 358:1668–1675.

18. Jo KD, Lee MC. Oral sumatriptan for acute treatment of migraine A single-blind placebo-controlled study. J Korean Neurol Assoc. 1995. 13:77–83.
19. Noh YW, Lee TG, Park KH, Kim SM, Chung KC. A double-blinded, placebo-controlled, multicenter cross-over study of 2.5mg naratriptan in acute migraineurs. Korean J Headache. 2001. 2:53–60.
20. Pfaffenrath V, Cunin G, Sjonell G, Prendergast S. Efficacy and safety of sumatriptan tablets (25 mg, 50 mg, and 100 mg) in the acute treatment of migraine: defining the optimum doses of oral sumatriptan. Headache. 1998. 38:184–190.

21. Rapoport AM, Ramadan NM, Adelman JU, Mathew NT, Elkind AH, Kudrow DB, et al. The 017 Clinical Trial Study Group. Optimizing the dose of zolmitriptan (Zomig, 311C 90) for the acute treatment of migraine. A multicenter, double-blind, placebo-controlled, dose range-finding study. Neurology. 1997. 49:1210–1218.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download