Abstract
Background and purpose
Percutaneous transluminal angioplasty (PTA) is being increasingly used in the treatment of symptomatic middle cerebral artery (MCA) stenosis. We evaluated the long-term durability after PTA for symptomatic MCA stenosis.
Methods
We analyzed consecutive patients included in our stroke database who were treated with angioplasty alone. The subjects without major periprocedural complications were followed up for at least 42 months. Recurrent ischemic symptoms were defined as newly developed episodes of transient ischemic attack or ischemic stroke in the territory of the treated vessel. Stroke was defined as ischemic stroke in any vessel.
Results
PTA was technically successful in 37 of the 40 included patients. Thirty-two of the 37 patients were followed up at regular intervals of 1 to 6 months in the outpatient clinic of our institution for at least 42 months. Restenosis occurred in 3 of the 32 patients (9.4%) within 2 years of PTA, and no restenosis was identified thereafter. Two of the three patients with restenosis had asymptomatic complications such as dissection and vasospasm during the intervention. The ischemic area was in the treated vessel in 1 of the 32 patients and in other vessels in 3 of the 32 patients (9.4%).
Intracranial atherosclerosis is a major cause of ischemic stroke (IS) in Asian populations. Previous studies found annual incidences of stroke recurrence in patients with symptomatic middle cerebral artery (MCA) stenosis of 8-15%.1-5 Medical treatment has been widely and empircally used, but there is still a high rate of failures that result in recurrent transient ischemic attack (TIA), stroke, and death in symptomatic patients.4 Consequently, there is ongoing controversy on the optimal therapeutic strategies for these patients. Nowadays endovascular therapy has emerged as an alternative potential therapeutic option for patients with symptomatic MCA stenosis. With recent imrovements in microcatheter technology, percutaneous transminal angioplasty (PTA) is now being increasingly used in the treatment of symptomatic MCA stenosis. There are several reports of fair results of PTA in selected patients with intracranial arterial disease,3,6,7 but there are few reports on the long-term durability of PTA for MCA stenosis.8 Restenosis after endovascular treatment has emerged as a significant complication, with a reported rate as high as 32%.3 Therefore, the present study evaluated the long-term durability of PTA for symptomatic MCA stenosis.
We analyzed consecutive patients included in our stroke database who were treated with angioplasty alone. Between February 1996 and December 2004, 56 patients underwent 57 PTA procedures for the treatment of symptomatic MCA stenosis at our institution. Exclusion criteria comprised acute intervention performed within 3 days of symptom onset (n=2), undergoing MCA angioplasty for the treatment of acute cardiogenic embolic occlusion (n=11) or vasospasm after subarachnoid hemorrhage (n=2), and atherosclerotic stenosis in the M2 segment of the MCA (n=1).9 All patients and their family members provided informed consents before the procedure. All patients had severe MCA stenosis (>50% luminal narrowing) with ischemic symptoms despite medical treatment. Briefly, the stenosis percentage was quantified as the diameter of maximal narrowing (D narrow) relative to the diameter of the normal (D normal) symptomatic MCA just distal or proximal to the stenosis: {1-(D narrow/D normal)}×100%.10 The normal portion of the MCA was defined as where the MCA walls appeared parallel on angiography.
PTA was performed by two experienced radiologists. The detailed method for PTA has been reported previously.9 A 6-F guiding catheter was inserted into the cervical portion of the internal carotid artery over an exchange wire. The first 30 patients were treated with Stealth angioplasty balloons (Target Therapeutics, Fremont, CA), and the last 10 patients were treated with coronary balloons (HayatePro, Terumo, Tokyo, Japan). The balloon was inflated slowly with a screw-type pressure inflation device at 2-4 atm for 30-60 seconds either once or twice. Follow-up angiography was performed using a guiding catheter after the procedure, and the degree of residual stenosis was recorded. We defined technical success as a residual stenosis of less than 50% on follow-up angiograms without any serious complications. After the procedure, heparin was infused intravenously for 24 hours, and antiplatelet medication (a daily dose of 325 mg of aspirin plus 250 mg ticlopidine or 75 mg clopidogrel) was maintained continuously during the follow-up period.
Imaging follow-up was performed with CT angiograms at 6 months, 12 months, and yearly or biannually thereafter. Regular transcranial Doppler (TCD) follow-up was performed on 32 patients for first 6 months. After these, 19 patients underwent regular TCD follow-ups. A single-channel 2-MHz Doppler device was used for TCD examinations. M1 MCA was defined as an insonation depth of 45-65 mm.11,12 All recordings were performed by an experienced sonographer who was not involved in the other aspects of the study. Patients regularly underwent TCD examinations on day 1 and at months 1 and 6 after PTA. We evaluated several parameters, including the mean flow velocity (MFV) and peak systolic velocity (PSV), in order to assess flow velocity changes after PTA.
Major complications were defined as symptomatic and severe neurological deficits related to procedures, and minor periprocedural complications were defined as asymptomatic or transient neurological deficits. Restenosis was defined as an increase in the MFV of >30 cm/sec between two consecutive TCD examinations or as >50% stenosis measured on follow-up CT angiograms. If velocity changes remained below this threshold, the stenosis was considered to be stable. When a decrease of >30 cm/s was observed, we considered MCA stenosis to have regressed. This threshold value of 30 cm/s for sonographic progression and regression was based on previously described criteria.13 Recurrent ischemic symptoms were defined as newly developed episodes of TIA or ischemic stroke in the territory of the treated vessel. Stroke was defined as ischemic stroke in any vessel.
Except where stated otherwise, data are presented as median values for continuous variables and as percentages for categorical variables. We compared baseline demographics and clinical risk factors using the chi-square test for categorical variables and Student's t-test for continuous risk factors between the TIA and ischemic stroke groups. We also used the Wilcoxon signed-rank test to compare baseline and follow-up TCD values. The Kaplan-Meyer method was used to estimate event-free survival rates. The data were analyzed using SPSS version 14.0.
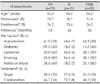
PTA was technically successful in 37 of the 40 patients, with major complications (subarachnoid hemorrhage and cerebral infarction) in 2 cases and 1 case of technical failure. Other periprocedural complications were asymptomatic or no neurological sequelae (2 TIAs, 3 intimal dissections, and 1 vasospasm). The rate of minor periprocedural complications was 16.2% (6 of 37 patients). Thirty-two of the 37 patients were followed up at regular intervals of 1 to 6 months in the outpatient clinic of our institution for at least 42 months. Therefore, the 32 subjects included in this study underwent successful PTA without any major periprocedural complications and were followed up for at least 42 months. They comprised 18 men and 14 women with a mean age of 56.5 years. Presenting symptoms were TIA in 21 patients (65.6%) and ischemic stroke in 11 patients (34.4%). The degree of stenosis before the procedure ranged from 50% to 95% (median, 75.5%), whereas the degree of residual stenosis after the procedure ranged from 9% to 48% (median, 21%). The general characteristics of the subjects (including risk factors and treatment) did not differ significantly between the two groups (Table 1). During the median follow-up period of 56 months (range, 42 to 115 months), restenosis occurred in 3 of the 32 patients (9.4%) within 2 years of PTA, and no restenosis was identified thereafter (Fig. 1). Two of the 3 patients with restenosis had asymptomatic complications such as dissection and vasospasm during the intervention (Table 2). The ischemic area was in the treated vessel in 1 of the 32 patients and in other vessels in 3 of the 32 patients (9.4%)(Fig. 2).
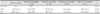
TCD examinations showed a preprocedural MFV of 165.9±47.6 cm/s (mean±SD) and a preprocedural PSV of 208.7±61.2 cm/s (n=32), which declined to 146.2±53.9 and 186.4±68.7 cm/s, respectively, immediately after the procedure (p<0.05). In patients with serial TCD evaluations, the MFV and PSV gradually declined during 6 months of follow-up (n=19, p<0.05)(Table 3).
In this study, the rates of restenosis and recurrent ischemic events were lower for successful PTA for MCA stenosis, with there being no patients with restenosis 2 years after PTA. Compared with previous data on the risk of medically treated MCA stenosis, the long-term durability and outcomes of successful PTA appear favorable.1,4 Recurrent ischemic events in the distribution of the treated vessel occurred in 3.1% of the patients within a median follow-up period of 56 months. In addition, major procedural complications after PTA that caused residual deficits or death were uncommon.9 Subjects with major procedural complications after PTA were excluded from the present study in order to assess the durability of successful PTA in patients with symptomatic MCA stenosis. Our results indicate that successful PTA can maintain the patency of the treated artery for up to 115 months. Wojak et al. attributed a decrease in the rate of ischemic symptoms after angioplasty to multiple factors such as an increase in vessel lumen, which increases blood flow, and remodeling of the endothelial surface to a smoother surface, which theoretically is less thrombogenic.14 In our study, the TCD data showed that the MFV at the stenotic artery did not decrease from normal values until 12 months after PTA. This result indicates that the remodeling of the vessel surface and the widening of vessel lumen can take several months after PTA, and also suggests that restenosis is more likely to develop in the early period after PTA. However, Fiorella et al. reported that the preprocedural velocity of 127.7 cm/s declined to 54.0 cm/s immediately after the procedure.15 This difference might have been due to technical differences. Although our results differ from previous reports, TCD appears to be a favorable modality for follow-up after PTA.11,13-15 Future studies should investigate this difference. In addition, long-term durability of PTA could be favorable despite the possibility of complications or restenosis in the early period. The reported restenosis rate after angioplasty has ranged from 15% to 50%.7,8,14,16,17 Mazighi et al. recently reported that restenosis after treatment was associated with a vessel size of <2.5 mm or interventions that were performed in the setting of an acute stroke.8 Two of our three restenosis subjects were associated with asymptomatic procedural problems such as vasospasm and dissection. However, factors associated with restenosis were not found in this study, and restenosis was not related to clinical recurrence. Therefore, we consider restenosis to be a slowly progressing event after PTA. Recurrent stroke occurred in four patients during the follow-up period. However, recurrent stroke in the territory of the treated artery did not occur with the exception of one occurrence of TIA, which demonstrates that PTA reduces the rate of recurrent events in the territory of the treated artery.
The results of this study are subject to at least two limitations: 1) the use of a small sample with single-center results and 2) the use of imperfect follow-up imaging studies for evaluating restenosis, since conventional angiography (which is the reference standard) was performed in only a few patients. Although TCD was performed on some patients during the follow-up, it has several disadvantages in the diagnosis of MCA stenosis.
From the results of this study, it is concluded that successful PTA in patients with symptomatic MCA stenosis is associated with a low long-term rate of recurrent ischemic symptoms and that restenosis after the procedure is more frequent in the early period. However, restenosis does not appear to be associated with ischemic symptoms. Further studies are needed to evaluate the long-term efficacy and safety of PTA.
Figures and Tables
 | Fig. 1Arterial patency after angioplasty excluding patients with significant postprocedural complications. The restenosis rate was 9.37% (3 of the 32 patients) within 2 years of PTA, and no restenosis was identified thereafter. PTA: percutaneous transminal angioplasty. |
 | Fig. 2Ischemic events occurring after successful PTA. The ischemic area was in the treated vessel in 1 of the 32 patients and in other vessels in 3 of the 32 patients. PTA: percutaneous transminal angioplasty. |
References
1. Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005. 352:1305–1316.

2. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The northern Manhattan stroke study. Stroke. 1995. 26:14–20.

3. SSYLVIA Study Investigators. Stenting of symptomatic atherosclerotic lesions in the vertebral or intracranial arteries (SSYLVIA): study results. Stroke. 2004. 35:1388–1392.
4. Chimowitz MI, Kokkinos J, Strong J, Brown MB, Levine SR, Silliman S, et al. The warfarin-aspirin symptomatic intracranial disease study. Neurology. 1995. 45:1488–1493.

5. Thijs VN, Albers GW. Symptomatic intracranial atherosclerosis: outcome of patients who fail antithrombotic therapy. Neurology. 2000. 55:490–497.

6. Mori T, Mori K, Fukuoka M, Arisawa M, Honda S. Percutaneous transluminal cerebral angioplasty: serial angiographic follow-up after successful dilatation. Neuroradiology. 1997. 39:111–116.

7. Alazzaz A, Thornton J, Aletich VA, Debrun GM, Ausman JI, Charbel F. Intracranial percutaneous transluminal angioplasty for arteriosclerotic stenosis. Arch Neurol. 2000. 57:1625–1630.

8. Mazighi M, Yadav JS, Abou-Chebl A. Durability of endovascular therapy for symptomatic intracranial atherosclerosis. Stroke. 2008. 39:1766–1769.

9. Yoon W, Seo JJ, Cho KH, Kim MK, Kim BC, Park MS, et al. Symptomatic middle cerebral artery stenosis treated with intracranial angioplasty: experience in 32 patients. Radiology. 2005. 237:620–626.

10. Kappelle LJ, Eliasziw M, Fox AJ, Sharpe BL, Barnett HJ. Importance of intracranial atherosclerotic disease in patients with symptomatic stenosis of the internal carotid artery. The north American symptomatic carotid endarterectomy trail. Stroke. 1999. 30:282–286.

11. Demchuk AM, Christou I, Wein TH, Felberg RA, Malkoff M, Grotta JC, et al. Specific transcranial Doppler flow findings related to the presence and site of arterial occlusion. Stroke. 2000. 31:140–146.

12. Demchuk AM, Christou I, Wein TH, Felberg RA, Malkoff M, Grotta JC, et al. Accuracy and criteria for localizing arterial occlusion with transcranial Doppler. J Neuroimaging. 2000. 10:1–12.

13. Arenillas JF, Molina CA, Montaner J, Abilleira S, González-Sánchez MA, Alvarez-Sabín J. Progression and clinical recurrence of symptomatic middle cerebral artery stenosis: a long-term follow-up transcranial Doppler ultrasound study. Stroke. 2001. 32:2898–2904.

14. Wojak JC, Dunlap DC, Hargrave KR, DeAlvare LA, Culbertson HS, Connors JJ 3rd. Intracranial angioplasty and stenting: long-term results from a single center. AJNR Am J Neuroradiol. 2006. 27:1882–1892.
15. Fiorella D, Chow MM, Anderson M, Woo H, Rasmussen PA, Masaryk TJ. A 7-year experience with balloon-mounted coronary stents for the treatment of symptomatic vertebrobasilar intracranial atheromatous disease. Neurosurgery. 2007. 61:236–242. discussion 242-233.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download