Abstract
The co-occurrence of multiple sclerosis and peripheral demyelinating neuropathy is rare. It has been disputed whether these are pathologically related or coincidental findings. We report a 36-year-old woman who presented with diplopia, right facial palsy and left-sided weakness. Brain magnetic resonance imaging showed a lesion indicative of central demyelinating disease. Nerve conduction studies revealed peripheral multifocal demyelinating neuropathies. We suggest that the central and the peripheral lesions may be continua of a demyelinating process.
Co-occurrence of multiple sclerosis (MS) and peripheral demyelinating neuropathy is rare, and there have been disputed whether these are pathogenetically related or coincidental findings.1-8 We report a combination of MS and peripheral multifocal demyelinating neuropathies in a Korean patient.
A 36-year-old woman presented in April, 2006 with one week history of sustained headache in the right temporal area associated with numbness of the right face, hearing impairment, and vertigo. Ten years before, she underwent a thyroid gland operation due to hyperthyroidism and had been under thyroid hormone replacement therapy. Four months before the admission, she underwent a Caesarean section and had been breast-feeding. She had never experienced dry mouth, xerophthalmia, skin or oral ulcer, spontaneous abortion, or arthritis. Family history and other medical history were unrevealing. On admission, she complained of diplopia, but extraocular movement dysfunction or nystagmus were not observed. Muscle weakness of right face and palate were recorded, but dysphagia and dysarthria were not definite. Mild weakness of left extremities was recorded and deep tendon reflexes of left side were hypoactive. Pathologic reflexes or abnormality of muscular tone were not recorded. Her cerebellar function test was insignificant.
Her chest and cardiologic evaluation results were normal. Laboratory test such as complete blood cell count, erythrocyte sedimentation rate, and serologic tests including C-reactive protein, anti-GQ1b antibody, syphilis serology, human immunodeficiency virus antibody, rheumatoid factor, autoimmune markers such as antinuclear antibody, serum immunoglobulin did not show any abnormality. Her urine analysis did not show hematuria or proteinuria. Cerebrospinal fluid (CSF) analysis showed a protein level of 63 mg/dL, a glucose level of 65 mg/dL, and 3 cells/mm3. An immunoglobulin G index (IgG index) was 0.564 and the CSF level of myelin basic protein (MBP) was 10 ng/mL (normal level <1 ng/mL). An oligoclonal band of CSF was not demonstrated. The motor nerve conduction velocities of both median and ulnar nerves were markedly decreased and multiple conduction blocks were recorded on left median and both ulnar nerves (Fig. 1). The F wave latencies of both median, ulnar, tibial, and left peroneal nerves were prolonged and H-reflexes were not demonstrated bilaterally. These nerve conduction studies (NCS) were indicative of multifocal demyelinating neuropathies (Table 1-A). Pattern reversal visual-evoked potentials (VEP) and brainstem auditory-evoked potentials (BAEP) fell within normal ranges.
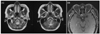
On hospital day 1, T2-weighted and fluid-attenuated inversion recovery magnetic resonance imaging (MRI) studies revealed an increased signal intensity in the right cerebellopontine angle with gadolinium-enhancement (Fig. 2). This lesion showed high signal intensity on diffusion MRI and apparent diffusion coefficient maps. She did not receive any treatment because her husband wanted her to be treated by oriental medicine. Five days later, she was admitted again because of left-sided numbness and ataxia with aggravated dizziness. A follow-up MRI did not reveal any newly developed lesion. She was diagnosed as having multifocal demyelinating neuropathies and probable demyelinating disorder of central nervous system (CNS). Intravenous immunoglobulin (0.4 g/kg per day) was administered for 5 days. On the fourth day of immunoglobulin treatment, most of left sided-weakness and ataxia disappeared. After 15 days, the NCS showed decreased F-wave latencies of all tested nerves compared with those of previous study (Table 1-B). For about 3 months after discharge, her gait disturbance and ataxia were resolved, but numbness of right extremities appeared transiently.
In August, 2006, she was admitted for the third time because of decreased visual acuity and color vision of right eye (0.2 OD; 1.0 OS). The swinging flashlight test showed the Marcus-Gunn pupillary sign on right eye. Other cranial nerves, motor, and sensory examinations were unrevealing. Reflexes of four extremities were hyperactive. On ophthalmoscopic examination, blurred margin of right optic disc was recorded. VEP showed prolonged P100 latency on right eye indicative of a prechiasmatic conduction defect of right visual pathway (Fig 3-A). Orbit MRI showed a gadolinium enhanced lesion on a prechiasmatic area of right optic nerve and a region of abnormally high signal intensity on left lateral medulla, which corresponded with right sided-numbness ( Fig 4). A follow-up CSF analysis showed a protein level of 59 mg/dL, a glucose level of 58 mg/dL, and 0 cells/mm3. An IgG index was 0.568 and MBP level was 2.2 ng/mL. An oligoclonal band of CSF was not demonstrated. Thus, she was diagnosed as having right optic neuritis and MS and intravenous high dose steroid pulse therapy (1000 mg/day) was done for 5 days, with gradual tapering with oral prednisolone (1 mg/kg). Her visual acuity of right eye showed marked improvement in 2 weeks after steroid pulse therapy.
MS is a chronic disorder characterized by recurrent and relapsing lesions occurring in the brain, optic nerves, and the spinal cord.9 The specific pathologic finding of MS is central demyelination which does not extend beyond the root entry zones of the cranial and spinal nerves.9 As several cases of MS combined with peripheral demyelinating neuropathy have been reported, questions have been arising whether MS lesions should not extend beyond the root entry zones.1-8 Pollock et al. found demyelination of peripheral nerves in sural nerve biopsy of 10 patients with MS and suggested that the peripheral myelin might be involved in MS.8 Furthermore, Mendell et al. detected white matter lesions indistinguishable from those seen in MS in 16 patients with inflammatory demyelinating polyradiculoneuropathy.10
In our case, weakness and ataxia of left extremities, weakness and hypoesthesia of right face, and vertigo developed as initial manifestations which were followed by transient numbness of right extremities. Four months later, right optic neuritis suddenly developed. Thus, the series of manifestations appear to be compatible with temporal dissemination of demyelination process. Her serial brain MRI showed spatially disseminated demyelinating lesions. She was diagnosed as having MS on the basis of current diagnostic criteria.11 On the first admission, her neurologic examination showed mild weakness and hyporeflexia of left extremities and the NCS revealed peripheral multifocal demyelinating neuropathies without past history of peripheral nervous system lesion. Without pathological study, it is difficult to confirm whether the two disorders occurred coincidentally or occurred as different manifestations of the same demyelinating process. MS is rare in Korea as compared to western countries. Demyelinating neuropathy is also an uncommon disorder. The clinical course of the patient as well as the co-occurrence of two rare diseases suggest that the central and the peripheral demyelination might be different manifestations of a broad spectrum of the same immunopathologic dysfunction.
Figures and Tables
Figure 1
Demyelinating pattern with conduction block and temporal dispersion in motor conduction studies of left median nerve (2006.04.24, before the treatment).

Figure 2
Brain MRI on first admission, (A) T2-weighted image showed a region of increased signal intensity in right cerebellopontine angle and (B) in gadolinium-enhanced image this lesion showed gadolinium-enhancement.

References
1. Rosenberg NL, Boudette D. Hypertrophic neuropathy and multiple sclerosis. Neurology (Cleveland). 1983. 33:1361–1364.

2. Ro YI, Alexander B, Oh SJ. Multiple sclerosis and hypertrophic demyelinating peripheral neuropathy. Muscle Nerve. 1983. 6:312–316.

3. Poser CM. The peripheral nervous system in multiple sclerosis. A review and pathogenetic hypothesis. J Neurol Sci. 1987. 79:83–90.
4. Naganuma M, Shima K, Matsumoto A, Tashiro K. Chronic multifocal demyelinating neuropathy associated with central nervous system demyelination. Muscle Nerve. 1991. 14:953–959.

5. Almsaddi M, Bertorini TE, Seltzer WK. Demyelinating neuropathy in a patient with multiple sclerosis and genotypical HMSN-1. Neuromuscul Disord. 1998. 8:87–89.

6. Lee CH, Kim BJ, Park KW, Koh SB, Kim HJ, Lee DH. Chronic inflammatory demeylinating polyneuropathy developed during interferon-β therapy in a patient with multiple sclerosis. J Korean Neurol Assoc. 2006. 24(5):486–490.
7. Matsuse D, Ochi H, Tashiro K, Nomura T, Murai H, Taniwaki T, et al. Exacerbation of chronic inflammatory demyelinating polyradiculoneuropathy during interferonβ-1b therapy in a patient with childhood-onset multiple sclerosis. Intern Med. 2005. 44(1):68–72.

8. Pollock M, Calder C, Allpress S. Peripheral nerve abnormality in multiple sclerosis. Ann Neurol. 1977. 2:41–48.

9. Ropper AH, Brown RH. Adams and Victor's Principles of neurology. 2005. 8th ed. New York: McGraw Hill;771–796.
10. Mendell JR, Kolkin S, Kissel JT, Weiss KL, Chakeres DW, Rammohan KW. Evidence for central nervous system demyelinating in chronic inflammatory demyelinating polyradiculoneuropathy. Neurology. 1987. 37:1291–1294.

11. Kim BJ, Lee KH. Diagnosis of multiple sclerosis. J Korean Neurol Assoc. 2005. 23:143–151.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download