Abstract
Background and Purpose
123I cardiac meta-iodobenzylguanidine (MIBG), an analogue of norepinephrine, has been used to estimate myocardial sympathetic nerve function. We investigate whether cardiac-MIBG SPECT is clinically applicable in the differentiation of Parkinson's disease (PD) from parkinsonian syndromes.
Methods
Cardiac-MIBG scintigraphy was performed in 27 controls, in 40 patients with PD and in 52 patients with other parkinsonian syndromes comprising 23 with multiple system atrophy (MSA), 26 with drug-induced parkinsonism (DIP), and 3 with corticobasal degeneration (CBD). The heart to mediastinum (H/M) uptake ratio was calculated for each subjects. Patients who either had medical conditions that confused the MIBG SPECT results or who took medications that interfere with MIBG accumulation were excluded from the study.
Results
Both early and delayed H/M ratios were in patients with PD significantly lower than in controls (early, 1.34±0.15 vs 1.79±0.19; delayed, 1.29±0.15 vs 2.06±0.29, p<0.001). In patients with PD, both early and delayed H/M ratios were significantly lower than those in patients with MSA (early, 1.68±0.23; delayed, 1.80±0.34, p<0.001), DIP (early, 1.83±0.24; delayed, 2.07±0.4, p<0.001), or CBD (early, 1.85±0.01; delayed, 1.99±0.19, p<0.001). Two patients with DIP, who were within the range of patients with PD, showed clinically similar courses of PD.
Although the diagnosis of Parkinson's disease (PD) appears simple, a recent clinicopathological study found that up to 25% diagnoses in patients with PD made by nonspecialists were incorrect according to the postmortem pathological results.1,2 Most misdiagnoses involved the differentiation between PD and atypical parkinsonism. In atypical parkinsonian syndrome, this disease generally progresses rapidly, responds poorly to dopaminergic agents, and has additional symptoms, such as autonomic symptoms, cerebellar ataxia, limited vertical eye movements, cortical sensory disturbances, and pyramidal symptoms. Atypical parkinsonism includes dementia with Lewy bodies, multiple system atrophy (MSA), progressive supranuclear palsy (PSP), and corticobasal degeneration (CBD). It is important to differentiate atypical parkinsonism from PD to make an accurate prognosis and devise a proper treatment plan without unnecessary costs or surgery.
The clinical manifestations of drug-induced parkinsonism (DIP), which constitutes 15-60% of parkinsonism cases, are very similar to those of PD. Usually, the parkinsonian symptoms resolve within a few weeks after the patient stops taking the offending drug. Since several irreversible cases of DIP have been reported,3,4 and Burn and Brooks showed that there was dysfunction of the nigrostriatal pathway in one-third of DIP cases using 18F-dopa PET,5 we believe that in these cases, the offending drug revealed PD at a preclinical stage.
Since 123I-meta-iodobenzylguanidine (MIBG) is a sympathomimetic, it is taken up by the norepinephrine transporter, stored in vesicles at postganglionic sympathetic nerve terminals, and released into the synapse by nerve stimuli. Whereas norepinephrine is degraded after release by monoamine oxidase or catechol-O-methyltransferase, MIBG is unaffected, allowing visualization of the function of sympathetic nerves noninvasively.6-9 The degree of MIBG uptake reflects whether the postganglionic sympathetic nerve is damaged. Several studies using this technique showed that 123I-MIBG is useful for differentiating PD from atypical parkinsonism, especially MSA.10-13
In this study, we compared the results of cardiac-MIBG imaging in patients with MSA, CBD, and DIP to demonstrate its usefulness in differentiating PD from atypical parkinsonism.
This study examined 119 patients and controls. PD, MSA, and CBD were diagnosed using both the United Kingdom Parkinson's Disease Society Brain Bank Clinical Diagnosis Criteria2 proposed by Gilman et al.14 and the criteria proposed by Boeve et al.15 DIP was diagnosed using the following three criteria: 1) the presence of least two of the four cardinal signs (tremor, rigidity, bradykinesia, and impaired postural reflexes), 2) the absence of a history of extrapyramidal disorders before treatment with the offending drug, and 3) the onset of symptoms in the course of treatment with the offending drug. The severity of symptoms was classified according to Hoehn and Yahr (H&Y).16 The clinical stage of DIP was assessed at the initial evaluation and 6 months after withdrawal of the offending drug.
The patients had no history of exposure to either neuroleptic drugs or any other cause of secondary parkinsonism. Other exclusion criteria were spondylotic or vascular myelopathy, infections, gammopathies, dysimmune or toxic neuropathies, alcoholism, diabetes mellitus, or other diseases that affect the autonomic nervous system. None of the patients had a history of ischemic heart disease, especially of myocardial infarction, thyroid disease, arterial hypertension, or evidence of myocardial ischemia on electrocardiogram. None of the patients received any of the substances that are known, expected, or expected to interfere with 123I-MIBG uptake.
The controls had no history of either ischemic heart disease or peripheral neuropathy, and no neurological symptoms. None of the controls received drugs that might affect the uptake of 123I-MIBG.
123I-MIBG (111 mBq) was injected intravenously into each subject. Three hours later, the image of cardiac uptake was taken using a dual-head γ-camera SPECT (MultiSPECT III; Siemens Medical Systems, Iselin, NJ, USA). The region of interest consisted of the entire heart and mediastinum in the frontal image. The ratio of 123I-MIBG uptake in the heart to that in the mediastinum (H/M ratio) was calculated (Fig. 1).
The results are expressed as the means±SD values. The chi-square test, analysis of variance (ANOVA), and receiver operating characteristic curve were used to examine the differences between groups using commercial software (SPSS, version 12.0 and MedCalc), and p values less than 0.05 were considered statistically significant.
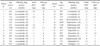
The patients included 40 indivisuals with PD (22 females, 18 males; mean age, 64.56 years; mean duration of disease, 46.78±30.37 months; H & Y stage, 2.25±0.95), 23 with MSA (10 females, 13 males; mean age, 57.13 years; mean duration of disease, 44.21±15.68 months; H & Y stage, 3.58±1.02), and 3 with CBD (1 female, 2 males; mean age, 68.8 years). There were 27 controls (15 females, 12 males; mean age, 66.11 years). The patients with MSA were significantly younger than those in the other groups (p<0.05) and the H&Y stage was significantly lower for MSA patients than for PD patients (p<0.01), although there was no significant difference in the proportion of males and females. Table 1 lists details of the offending drugs and information on the DIP patients.
Fig. 2-A and 2-B show the respective distributions of the early and delayed H/M ratios of the controls and those within each disease subgroup. The H/M ratio in the early and delayed images was significantly lower in PD thant in the controls (early PD, 1.34±0.15 vs. 1.79±0.19; delayed, 1.29±0.15 vs. 2.06±0.29; p<0.001). In addition, the H/M ratio was markedly lower in PD patients than in MSA patients (early, 1.68±0.23; delayed, 1.80±0.34; p<0.001), CBD patients (early, 1.85±0.04; delayed, 1.99±0.19; p<0.001), and DIP patients (early, 1.83±0.24; delayed, 2.07±0.4; p<0.001). The MIBG H/M ratios did not differ significantly among patients with MSA, CBD, DIP, and controls.
The threshold values of the early and delayed H/M ratios that distinguished PD patients from the controls were 1.57 (sensitivity, 95.0%; specificity, 88.9%) and 1.56 (sensitivity, 95.0%; specificity, 100%), respectively. There was no difference in the discriminating power of the early and delayed H/M ratios (p=0.188, 95% CI= -0.014 to 0.07; Fig. 3). The thresholds of the early and delayed H/M ratios that distinguished PD patients from MSA patients were 1.38 (sensitivity, 65.7%; specificity, 95.7%) and 1.36 (sensitivity, 80.0%; specificity, 100%), respectively. The delayed H/M ratio was statistically better than the early H/M ratio (p=0.068, 95% CI= -0.005 to 0.138; Fig. 3).
The degree of reduced cardiac-MIBG uptake (delayed H/M ratio minus early H/M ratio) was significantly higher in PD patients (-0.05±0.12) than in the controls (0.26±0.22; p<0.001) and MSA patients (0.12±0.21; p<0.025).
Twenty-four of the 26 patients with DIP had an H/M ratio within 2 standard deviations of the mean, while two patients had values below 1.57, which was the borderline value between the control and PD patients, and fell within the range of the PD patients. The 24 patients with DIP whose MIBG uptake was within the normal range showed dramatic improvement or complete resolution of their parkinsonism on clinical follow-up 6 months after withdrawal of the offending drug, whereas the 2 DIP patients (numbers 7 and 16) whose MIBG uptake was significantly reduced exhibited persistent parkinsonism. Both of these patients responded well to treatment with levodopa, exhibiting improvements of (54% and 76% on the motor Unified Parkinson's Disease Rating Scale, respectively).
In this study, the cardiac-MIBG H/M ratio of PD patients was reduced markedly compared with that of controls and was clearly different from the cardiac-MIBG H/M ratios in patients with MSA, CBC, and DIP. In addition, the two DIP patients whose H/M ratios were within the range of PD patients showed a clinical course similar to that of the PD patients, in contrast to the patients whose H/M ratios were normal.
When PD was defined as an early H/M ratio below 1.57 and a delayed H/M ratio below 1.56 to discriminate PD from controls, the sensitivity and specificity were 95% and 88.9% for the early H/M ratio and 95% and 100% for the delayed H/M ratio, respectively. Although the late H/M ratio was more sensitive and specific, difference between the two ratios was not statistically significant (p=0.201). Therefore, for convenience, a diagnosis can be made using the early H/M ratio when the early ratio is above 1.57, in order to save the patients from waiting for 3h. Moreover, the threshold that differentiates patients with PD from those with MSA was an early H/M ratio of 1.38 (sensitivity, 65.7%; specificity, 95.7) and a delay H/M ration of 1.36 (sensitivity, 80.0%; specificity, 100%). The delayed H/M ratio was marginally more sensitive and specific compared with the early H/M ratio (p=0.068).
MIBG is not metabolized by catechol-O-methyltransferase or monoamine oxidase.17 Two uptake systems for MIBG have been identified in adrenergic tissues. The first system involves diffusion in non-neuronal and neuronal tissues. Scanning during the first 15 min postinjection mainly reflects the greater influx of MIBG into the extraneural space in myocardial tissue, rather than into the neuronal component. The second system is uptake by neuronal tissue using the sodium and ATP-dependent transporter at low concentrations. The neuronal accumulation of MIBG reaches its maximum at 3-4 h after injection, so a delayed MIBG scan reflects the neuronal uptake of MIBG more specifically. Therefore, myocardial MIBG uptake was assessed 15 min and 3-4 h postinjection.18
A decreased MIBG uptake suggests the loss or destruction of cardiac sympathetic nerve endings.19 Lewy bodies are found in the hypothalamus, intermediolateral cell columns of the spinal cord, and sympathetic ganglia in patients with PD.20,21,22 It is known that central or preganglionic lesions, such as those in the cardiovascular autonomic center of the ventrolateral medullar or intermediolateral cell column of the spinal cord, contribute to the dysautonomia of MSA.23,24 Orimo et al. reported that tyrosine-hydroxylase-immunoreactive sympathetic nerve fibers in the myocardium are reduced markedly in PD patients in contrast to those in both MSA and normal controls, suggesting that the involvement of postganglionic sympathetic nerve fibers, including sympathetic nerves in the myocardium, explains the difference in the uptake of MIBG.25 Cohen et al. hypothesized that in MSA, dysfunction of the postganglionic sympathetic fibers is caused by the trans-synaptic effects of the preganglionic lesion,26 and we postulate that this mechanism explains the reduced cardiac uptake of MIBG.
In recent studies, the cardiac-MIBG H/M ratio in patients with CBD was found to be within the range of normal controls, and tyrosine-hydroxylase-reactive sympathetic nerves in the myocardium appeared normal.27,28 Although the number of CBD patients in our study was small, the cardiac-MIBG H/M ratio in CBD patients was within the control range.
Different drugs, such as neuroleptics, calcium channel blockers, and dopamine-depleting agents, have different effects on dopaminergic receptors, which influence the clinical outcome of patients with DIP. Tolosa et al.29 divided DIP patients into three subgroups: 1) full, longlasting recovery of DIP with no subsequent development of PD (i.e., DIP is unrelated to PD); 2) persistence and eventual worsening of parkinsonism after discontinuation of the offending drug (DIP unmasks PD); and 3) full remission of DIP after withdrawal of the offending drug with the subsequent reappearance of parkinsonism (DIP antedates PD). Since the treatment and prognosis of DIP antedating PD are clearly different from those of DIP unrelated to PD, the differentiation of these disorders is very important. In this study, DIP patients who had a cardiac-MIBG H/M ratio in the normal range improved markedly or had their symptoms resolve within several weeks of withdrawal of the offending drug. In these patients, the DIP was very probably unrelated to PD. The two patients whose cardiac-MIBG H/M ratios were within the range of PD patients still had parkinsonian symptoms after withdrawal of the offending drug and these symptoms were improved with levodopa treatment. We postulate that these two patients had subclinical PD. Unfortunately, we did not perform functional imaging on these patients to evaluate the nigrostriatal system, so we cannot conclude that these patients definitely had subclinical PD.
Various drugs have been reported to influence cardiac-MIBG uptake. Haloperidol decreases MIBG uptake at very highly concentrations, albeit at concentrations far above therapeutic doses.30 Cilnidipine, a third-generation dihydropyridine-based calcium antagonist, is reported to enhance cardiac-MIBG uptake, which would lead to a falsely elevated MIBG uptakes; however, this effect is likely minimal because the increase in the H/M ratio after cilnidipine treatment is very small (~0.1).31 Chlorpromazine and perphenazine are expected to interfere with cardiac-MIBG uptake, although there is no direct evidence of this effect.32 Finally, there are no reports of interactions between levosulpiride, metoclopramide, risperidone, and MIBG. Therefore, we believe that the influence of any such drugs on MIBG uptake was trivial in the present study.
This study is limited by the absence of pathological diagnoses and the absence of functional imaging to evaluate the presynaptic and postsynaptic dopaminergic neurons of the nigrostriatal dopaminergic system. Therefore, the threshold, sensitivity, and specificity values obtained in our study may be inaccurate. However, we suggest that cardiac-MIBG SPECT is a useful method for differentiating PD from atypical parkinsonism and for detecting subclinical PD within DIP patients.
Figures and Tables
Figure 1
Definition of regions of interest (ROI) on an anterior planar image of a control subject. Rectangular ROIs are drawn on the heart (1) and mediastinum (2) for early (A) and delayed (B) images. Cardiac meta-iodobenzylguanidine (MIBG) uptake is assessed using the heart-to-mediastinum (H/M) activity ratio that determines the average count per pixel in the ROI.

Figure 2
Scatter diagram of an individual H/M ratio of 123I-MIBG uptake in patients with Parkinson's disease (PD), multiple system atrophy (MSA), drug-induced parkinsonism (DIP), and corticobasal degeneration (CBD), compared with controls (Con). The thick line indicates the mean value of the H/M ratio. Panels 2A and 2B indicate early and delayed MIBG images, respectively.

References
1. Schrag A, Ben-Shlomo Y, Quinn N. How valid is the clinical diagnosis of Parkinson's disease in the community? J Neurol Neurosurg Psychiatry. 2002. 73:529–534.

2. Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992. 55:181–184.

4. Hardie RJ, Lees AJ. Neuroleptic-induced Parkinson's syndrome: clinical features and results of treatment with levodopa. J Neurol Neurosurg Psychiatry. 1988. 51:850–854.

5. Burn DJ, Brooks DJ. Nigral dysfunction in drug-induced parkinsonism: an 18F-dopa PET study. Neurology. 1993. 43:552–556.

6. Jaques S Jr, Tobes MC, Sisson JC, Baker JA, Wieland DM. Comparison of the sodium dependency of uptake of meta-lodobenzylguanidine and norepinephrine into cultured bovine adrenomedullary cells. Mol Pharmacol. 1984. 26:539–546.
7. Wieland DM, Brown LE, Tobes MC, Rogers WL, Marsh DD, Mangner TJ, et al. Imaging the primate adrenal medulla with [123I] and [131I] meta-iodobenzylguanidine: concise communication. J Nucl Med. 1981. 22:358–364.
8. Mangner TJ, Tobes MC, Wieland DW, Sisson JC, Shapiro B. Metabolism of iodine-131 metaiodobenzylguanidine in patients with metastatic pheochromocytoma. J Nucl Med. 1986. 27:37–44.
9. Sisson JC, Wieland DM, Sherman P, Mangner TJ, Tobes MC, Jacques S Jr. Metaiodobenzylguanidine as an index of the adrenergic nervous system integrity and function. J Nucl Med. 1987. 28:1620–1624.
10. Druschky A, Hilz MJ, Platsch G, Radespiel-Troger M, Druschky K, Kuwert T, et al. Differentiation of Parkinson's disease and multiple system atrophy in early disease stages by means of I-123-MIBG-SPECT. J Neurol Sci. 2000. 175:3–12.

11. Yoshita M. Differentiation of idiopathic Parkinson's disease from striatonigral degeneration and progressive supranuclear palsy using iodine-123 meta-iodobenzylguanidine myocardial scintigraphy. J Neurol Sci. 1998. 155:60–67.

12. Saiki S, Hirose G, Sakai K, Kataoka S, Hori A, Saiki M, et al. Cardiac 123I-MIBG scintigraphy can assess the disease severity and phenotype of PD. J Neurol Sci. 2004. 220:105–111.

13. Courbon F, Brefel-Courbon C, Thalamas C, Alibelli MJ, Berry I, Montastruc JL, et al. Cardiac-MIBG scintigraphy is a sensitive tool for detecting cardiac sympathetic denervation in Parkinson's disease. Mov Disord. 2003. 18:890–897.

14. Gilman S, Low PA, Quinn N, Albanese A, Ben-Shlomo Y, Fowler CJ, et al. Consensus statement on the diagnosis of multiple system atrophy. J Neurol Sci. 1999. 163:94–98.

15. Boeve BF, Lang AE, Litvan I. Corticobasal degeneration and its relationship to progressive supranuclear palsy and frontotemporal dementia. Ann Neurol. 2003. 54:suppl 5. S15–S19.

17. Wieland DM, Brown LE, Rogers WL, Worthington KC, Wu JL, Clinthorne NH, et al. Myocardial imaging with a radioiodinated norepinephrine storage analog. J Nucl Med. 1981. 22:22–31.
18. Sisson JC, Shapiro B, Meyers L, Mallette S, Mangner TJ, Wieland DM, et al. Metaiodobenzylguanidine to map scintigraphically the adrenergic nervous system in man. J Nucl Med. 1987. 28:1625–1636.
19. Ganguly PK, Beamish RE, Dhalla KS, Innes IR, Dhalla NS. Norepinephrine storage, distribution, and release in diabetic cardiomyopathy. Am J Physiol. 1987. 252:E734–E739.

21. den Hartog Jager W, Bethlem J. The distribution of Lewy bodies in the central and autonomic nervous systems in idiopathic paralysis agitans. J Neurol Neurosurg Psychiatry. 1960. 23:283–290.

22. Rajput AH, Rozdilsky B, Rajput A. Accuracy of clinical diagnosis in parkinsonism--a prospective study. Can J Neurol Sci. 1991. 18:275–278.
23. Spokes EG, Bannister R, Oppenheimer DR. Multiple system atrophy with autonomic failure: clinical, histological and neurochemical observations on four cases. J Neurol Sci. 1979. 43:59–82.
24. Matthews MR. Bannister R, Mathias C, editors. Autonomic ganglia in multiple system atrophy and pure autonomic failure. Autonomic Failure. 1992. 3rd edn. Oxford: Oxford University Press;593–621.
25. Orimo S, Oka T, Miura H, Tsuchiya K, Mori F, Wakabayashi K, et al. Sympathetic cardiac denervation in Parkinson's disease and pure autonomic failure but not in multiple system atrophy. J Neurol Neurosurg Psychiatry. 2002. 73:776–777.

26. Cohen J, Low P, Fealey R, Sheps S, Jiang NS. Somatic and autonomic function in progressive autonomic failure and multiple system atrophy. Ann Neurol. 1987. 22:692–699.

27. Orimo S, Ozawa E, Nakade S, Hattori H, Tsuchiya K, Taki K, et al. [123I] meta-iodobenzylguanidine myocardial scintigraphy differentiates corticobasal degeneration from Parkinson's disease. Intern Med. 2003. 42:127–128.

28. Taki J, Nakajima K, Hwang EH, Matsunari I, Komai K, Yoshita M, et al. Peripheral sympathetic dysfunction in patients with Parkinson's disease without autonomic failure is heart selective and disease specific. Eur J Nucl Med. 2000. 27:566–573.

29. Tolosa E, Coelho M, Gallardo M. DAT imaging in drug-induced and psychogenic parkinsonism. Mov Disord. 2003. 18:S28–S33.

30. Mayer S, Karanikas G, Rodrigues M, Sinzinger H. Influence of drugs on myocardial iodine-123 metaiodobenzylguanidine uptake in rabbit myocardium. Eur J Nucl Med. 2000. 27:340–345.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download