Abstract
Background and Purpose
Intracranial atherosclerosis (ICAS) is one of the major risk factors for ischemic stroke, particularly in Asian populations. We investigated the prevalence and risk factors of ICAS in asymptomatic subjects.
Methods
We prospectively evaluated 835 asymptomatic Korean adults who voluntarily visited a tertiary referral hospital for a health screening examination that included brain magnetic resonance angiography. The subjects had no history of stroke or transient ischemic attacks; those who had potential cardiac sources of emboli were excluded. ICAS and extracranial atherosclerosis were defined as a reduction in luminal diameter of at least 50%. Vascular risk factors were screened through questionnaires, interviews, and examinations.
Results
ICAS was found in 25 subjects (3.0%) and extracranial atherosclerosis was found in 4 patients (0.5%). No patient had combined lesions. ICAS was distributed in 31 arteries in 25 subjects: anterior cerebral arteries (5 subjects, 16%), middle cerebral arteries (16 subjects, 52%), posterior cerebral arteries (8 subjects, 26%), and distal internal carotid arteries (2 subjects, 7%). The ratio of ICAS of the anterior circulation (23 of 31 arteries with ICAS, 74%) to that of the posterior circulation (8 of 31 arteries with ICAS, 26%) was 3:1. The ratio of ICAS (23 of 27 arteries with atherosclerosis in the anterior circulation, 85%) to extracranial atherosclerosis (4 of 27 arteries with therosclerosis in the anterior circulation, 15%) was 6:1. An older age [odds ratio (OR)=1.05, 95% confidence interval (CI)=1.00-1.10] and hypertension (OR=2.41, 95% CI=1.01-5.72) were independent risk factors for ICAS.
Intracranial atherosclerosis (ICAS) is reportedly more frequent in Asians, blacks, and Hispanics than in whites,1-8 and increases the risk of subsequent vascular events, such as cerebral ischemic stroke, transient ischemic attack, and death from vascular causes.9-13 ICAS reportedly causes 33% of ischemic strokes in Chinese patients, but is responsible for only 8% of ischemic strokes in whites.6,8 These racial or ethnic differences in cerebral atherosclerotic distribution are partially explained by the differences in vascular risk factors between these ethnic groups.3,6 Diabetes, age, sex, blood lipid levels, hypertension, and smoking have been proposed as risk factors for ICAS.1-6,14-16 However, most of the studies on the association between vascular risk factors and ICAS were performed in symptomatic patients,1-4,6,14-16 and studies in asymptomatic subjects are rare.
Although there has been recent remarkable progress in the treatment of acute ischemic stroke, the importance of developing a better strategy for stroke prevention cannot be overestimated. The knowledge of asymptomatic vascular stenosis can offer patients an opportunity to prevent subsequent vascular events.
The purpose of this study was to elucidate the prevalence and associated vascular risk factors of ICAS in asymptomatic subjects.
Between January 1996 and July 2001, 900 Korean adults (690 men and 210 women) who consecutively visited our hospital for a health screening examination were initially included in the study. A brain health-screening program was started in the mid-1990s to detect disease before the onset of symptoms. Under this program, anyone is able to request the screening at his or her own expense.
Sixty-five subjects were excluded from the analysis due to one of the following criteria: (1) the presence of previous cerebrovascular stroke (n=42), (2) the presence of atrial fibrillation (n=6), and (3) subjects in whom magnetic resonance angiography (MRA) was not performed (n=17). Therefore, 835 Koreans were analyzed.
Brain MRA was performed with a 1.5-T magnetic resonance imaging (MRI) unit (Signa Horizon Echospeed, General Electric Medical Systems). MRA consisted of a protocol of three-dimensional time-of-flight sequences. ICAS was defined as a reduction in luminal diameter of at least 50% using the method described in the Warfarin-Aspirin for Symptomatic Intracranial Disease Study.17 Extracranial atherosclerosis in the carotid artery was evaluated at the bifurcation level and was diagnosed if the reduction in luminal diameter was at least 50% as measured by the North American Symptomatic Carotid Endarterectomy Trial method.18 The extracranial vertebral artery was not included in the data analysis since a normal variant of congenital hypoplasia cannot be clearly differentiated from acquired stenosis by MRA.
Each subject completed a questionnaire that consisted of their demographics, smoking habits, and medical history that included hypertension, diabetes mellitus, ischemic heart disease, and family history of cerebrovascular disease (CVD). Each participant had an interview with a board-certified stroke specialist.
Patients were diagnosed with hypertension if they were either currently undergoing treatment with antihypertensive drugs, or if their systolic blood pressure was greater than 140 mmHg or their diastolic blood pressure was greater than 90 mmHg on two separate examinations. Patients were diagnosed with diabetes mellitus if they were currently undergoing treatment with insulin or oral hypoglycemic agents, or if their fasting blood glucose level was greater than 140 mg/dl. A smoking habit was defined as either smoking or nonsmoking. The smoking category was defined as either a current smoker or an ex-smoker who had stopped smoking less than 5 years previously. All others were included in the nonsmoking category. Ischemic heart disease was defined as a history of either angina pectoris or myocardial infarction. A family history of CVD was defined as a history of either cerebral infarction or nontraumatic hemorrhage in a parent, brother, sister, grandparent, uncle, aunt, or first cousin.
Laboratory evaluation included hematocrit, total serum cholesterol, triglycerides, HDL-cholesterol, and LDL-cholesterol levels after at least 8 hours of fasting. Electrocardiography (EKG) was performed and left ventricular hypertrophy (LVH) on EKG was defined as an S wave in V1 plus an R wave in V5 or V6 of at least 3.5 mV. Atrial fibrillation on EKG was defined as an irregularly spaced QRS complex without a discrete P wave.
Univariate analysis was performed by means of either the χ2 test or Fisher's exact test, which was used when at least one cell had an expected count less than 5, for categorical data. The Mann-Whitney U test was used to compare group means of continuous data. Multiple logistic regression was used to identify independent vascular risk factors for ICAS. Any variable with a p value no greater than 0.2 on univariate analysis was included in the logistic regression model. ICAS was a dependent variable. A p value of less than 0.05 was considered significant. Results are expressed as odds ratios (ORs) together with their 95% confidence intervals (CIs).
The ages of the 835 subjects ranged from 29 to 85 years (mean, 53 years), and comprised 639 men (76.5%) and 196 women (23.5%). ICAS was found in 25 subjects (3.0%) and extracranial atherosclerosis was found in 4 subjects (0.48%). No subject had both ICAS and extracranial atherosclerosis lesions.
ICAS was distributed in 31 arteries in 25 subjects: anterior cerebral arteries (5 of 31 arteries with ICAS, 16%), middle cerebral arteries (16 of 31 arteries with ICAS, 52%), posterior cerebral arteries (8 of 31 arteries with ICAS, 26%), and distal internal carotid arteries (2 of 31 arteries with ICAS, 6.5%). The middle cerebral arteries were the most frequently affected vessels followed by the posterior cerebral arteries. The ratio of ICAS that involved the anterior circulation (23 of 31 arteries with ICAS, 74%) to that involving the posterior circulation (8 of 31 arteries with ICAS, 26%) was 3:1. The ratio of ICAS (23 of 27 arteries with atherosclerosis in the anterior circulation, 85%) to extracranial atherosclerosis (4 of 27 arteries with atherosclerosis in the anterior circulation, 15%) was 6:1.
On univariate analysis of the cerebrovascular risk factors, the subjects with ICAS were older than those without atherosclerotic vascular stenosis (57±11 years vs. 53±7.9 years, p<0.05) and had higher levels of LDL-cholesterol (141±30.7 mg/dl vs. 128±32.3 mg/dl, p<0.05) (Table 1). Hypertension was found in 16 (64.0%) of 25 subjects with ICAS and in 303 (37.6%) of 806 subjects without atherosclerotic vascular stenosis (p<0.01). Diabetes mellitus, LVH on EKG, smoking, and a family history of CVD were more prevalent in the ICAS group, but the difference was not statistically significant. Mean total cholesterol levels were higher in the ICAS group but were not statistically significant. Hematocrit levels and the sex ratio were similar between the two groups. Mean triglyceride and HDL-cholesterol levels were lower in the ICAS group, but this was not statistically significant.
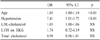
We performed multiple logistic regression analysis to identify independent vascular risk factors for ICAS (Table 2). The entered variables were age, hypertension, LDL-cholesterol, LVH on EKG, and total cholesterol, all of which had p values of no greater than 0.2 on univariate analysis. Multiple logistic regression revealed that an older age (OR=1.05, 95% CI=1.00-1.10, p<0.05) and hypertension (OR=2.40, 95% CI=1.01-5.69, p<0.05) were independent risk factors for ICAS.
ICAS was more frequent than extracranial atherosclerosis in this consecutively enrolled series of 835 neurologically asymptomatic Korean subjects, with asymptomatic atherosclerotic stenosis affecting predominantly the intracranial vessels in the anterior circulation (intracranial artery vs. extracranial artery, 6:1). The preponderance of intracranial vascular stenosis demonstrated in our study was consistent with the results of previous studies performed in symptomatic Asian, black, and Hispanic populations.1-3,6-8,16
However, the vascular risk factors associated with ICAS were different between symptomatic and asymptomatic populations. In this study, significant risk factors for ICAS were an older age (OR=1.05, 95% CI=1.00-1.10) and hypertension (OR=2.40, 95% CI=1.01-5.69), which did not show a significant association with ICAS in the stroke population.1-4,6,16
We speculate that the different proportions of symptomatic stroke patients between studies could explain the discrepancy in the association of hypertension with ICAS. Even in studies whose study population included some symptomatic stroke patients (24-53%), hypertension was also an independent risk factor for ICAS.5,15 However, this significant association between hypertension and ICAS was not observed in studies performed solely in stroke patients.1,3,4,6,16 In the studies performed in symptomatic stroke patients, the presence of patients with lacunar infarction in the control group could cause hypertension to be underestimated due to selection bias which we avoided in the present study.
Like hypertension, the association between an older age and ICAS was also underestimated in studies performed in stroke populations. Previous studies showed conflicting data on the association between ICAS and age in stroke populations.2-4,6,14,16 A younger age was significantly associated with ICAS in some stroke population studies,2,6 but this association was not significant in other studies that were also carried out in stroke populations.3,4,14,16 Furthermore, those results were not consistent with the conventional concept that an older age is one of the major risk factors for atherosclerosis.5,19 In studies whose study populations included fewer patients with stroke, an older age was a significant predictor for ICAS.5,15 Our study, which included no symptomatic stroke patients, also showed the same results.
The present study is subject to some limitations. First, the prevalence and associated vascular risk factors could not be directly applied to the general population. The present study was based on subjects who voluntarily underwent a health-screening examination, not on the general population. Therefore, these results are subject to a similar limitation in interpretation as those of previous studies that were performed in symptomatic patients. Second, although MRA is a convenient and noninvasive method for assessing vascular stenosis in asymptomatic subjects, there are technical difficulties in the evaluation of certain arteries, such as the siphon portion of the internal carotid arteries. Third, embolic lesions may resemble vascular stenosis on MRA, although we defined vascular stenosis on MRA as an atherosclerotic lesion. However, we presumed that the possibility of embolism was low since we included only asymptomatic subjects in this study and excluded those with potential cardiac sources of embolism.
In conclusion, ICAS is more prevalent than extracranial atherosclerosis in neurologically asymptomatic Korean subjects. Patients with ICAS are significantly older and have an increased frequency of hypertension compared with those subjects without atherosclerotic stenosis.
References
1. Feldmann E, Daneault N, Kwan E, Ho KJ, Pessin MS, Langenberg P, et al. Chinese-white differences in the distribution of occlusive cerebrovascular disease. Neurology. 1990. 40:1541–1545.

2. Gorelick PB, Caplan LR, Langenberg P, Hier DB, Pessin M, Patel D, et al. Clinical and angiographic comparison of asymptomatic occlusive cerebrovascular disease. Neurology. 1988. 38:852–858.

3. Inzitari D, Hachinski VC, Taylor DW, Barnett HJ. Racial differences in the anterior circulation in cerebrovascular disease. How much can be explained by risk factors? Arch Neurol. 1990. 47:1080–1084.

4. Lee SJ, Cho SJ, Moon HS, Shon YM, Lee KH, Kim DI, et al. Combined extracranial and intracranial atherosclerosis in Korean patients. Arch Neurol. 2003. 60:1561–1564.

5. Leung SY, Ng TH, Yuen ST, Lauder IJ, Ho FC. Pattern of cerebral atherosclerosis in Hong Kong Chinese. Severity in intracranial and extracranial vessels. Stroke. 1993. 24:779–786.

6. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction. The Northern Manhattan Stroke Study. Stroke. 1995. 26:14–20.

7. Suh DC, Lee SH, Kim KR, Park ST, Lim SM, Kim SJ, et al. Pattern of atherosclerotic carotid stenosis in Korean patients with stroke: different involvement of intracranial versus extracranial vessels. AJNR Am J Neuroradiol. 2003. 24:239–244.
8. Wong KS, Huang YN, Gao S, Lam WW, Chan YL, Kay R. Intracranial stenosis in Chinese patients with acute stroke. Neurology. 1998. 50:812–813.

9. Akins PT, Pilgram TK, Cross DT 3rd, Moran CJ. Natural history of stenosis from intracranial atherosclerosis by serial angiography. Stroke. 1998. 29:433–438.

10. Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005. 352:1305–1316.

11. Kappelle LJ, Eliasziw M, Fox AJ, Sharpe BL, Barnett HJ. Importance of intracranial atherosclerotic disease in patients with symptomatic stenosis of the internal carotid artery. The North American Symptomatic Carotid Endarterectomy Trial. Stroke. 1999. 30:282–286.

12. Uehara T, Tabuchi M, Mori E, Yamadori A. Evolving atherosclerosis at carotid and intracranial arteries in Japanese patients with ischemic heart disease: a 5-year longitudinal study with MR angiography. Eur J Neurol. 2003. 10:507–512.

13. Wong KS, Li H. Long-term mortality and recurrent stroke risk among Chinese stroke patients with predominant intracranial atherosclerosis. Stroke. 2003. 34:2361–2366.

14. Arenillas JF, Molina CA, Chacon P, Rovira A, Montaner J, Coscojuela P, et al. High lipoprotein (a), diabetes, and the extent of symptomatic intracranial atherosclerosis. Neurology. 2004. 63:27–32.

15. Ingall TJ, Homer D, Baker HL Jr, Kottke BA, O'Fallon WM, Whisnant JP. Predictors of intracranial carotid artery atherosclerosis. Duration of cigarette smoking and hypertension are more powerful than serum lipid levels. Arch Neurol. 1991. 48:687–691.

16. Wityk RJ, Lehman D, Klag M, Coresh J, Ahn H, Litt B. Race and sex differences in the distribution of cerebral atherosclerosis. Stroke. 1996. 27:1974–1980.

17. Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol. 2000. 21:643–646.
18. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. North American Symptomatic Carotid Endarterectomy Trial collaborators. N Engl J Med. 1991. 325:445–453.
19. Smith SC Jr, Milani RV, Arnett DK, Crouse JR 3rd, McDermott MM, Ridker PM, et al. Atherosclerotic Vascular Disease Conference: Writing Group II: risk factors. Circulation. 2004. 109:2613–2616.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download