Abstract
Background and Purpose
Multiple sclerosis (MS) in Asians is characterized by frequent involvement of the spinal cord and optic nerve and low prevalence rates, but even the most fundamental epidemiologic findings and unique clinical features of MS patients in Korea have not been studied extensively. We performed this study to establish the clinical spectrum of MS patients in Korea.
Methods
Sixty-two MS patients (25 men and 37 women) who satisfied the diagnostic criteria for definite MS were reviewed retrospectively using medical records from two university hospitals and one general hospital. The MS patients were classified into the three clinical subtypes according to the involved site (opticospinal, spinal, and conventional MS).
Results
The age at MS onset was 35.2±13.3 (mean±SD) years, and the predominant initial clinical manifestations were myelopathy (54.8%) and optic neuropathy (33.9%). The single most common involved lesion site was the spinal cord (35.5%). Spinal (35.5%) and opticospinal (25.8%) MS were the most common type, and they had a frequent relapsing-remitting course and long lesions extending over two vertebral segments (as assessed using spinal cord MRI). The interval between the first symptom and relapse was 35.6±71.1 months, and the number of relapses was 3.8±2.6. The spinal form of MS was associated with a higher age at onset and a higher male-to-female ratio than the other types. Positive rates of CSF oligoclonal bands and IgG index and the number of patients with characteristic brain MRI lesions were low. However, the abnormal rate of visual evoked potentials was relatively high (64.4%).
Multiple sclerosis (MS) is considered to be clinically heterogeneous. The prevalence of MS varies considerably both geographically and ethnically worldwide: it is 30-80 per 100,000 in Canada, northern Europe, and the northern United States; 6-14 per 100,000 in the southern United States and southern Europe; and less than 1 per 100,000 in equatorial areas.1,2 Many studies into MS have thus been carried out in Western countries. In Asians, MS is characterized by a lower prevalence, more frequent involvement of the optic nerve and spinal cord, and rare familial occurrence.3-6 However, as a result of the low prevalence and high migration rate, not even the most fundamental epidemiologic and large clinical studies have been performed in Korea.6 Furthermore, there are no specific pathognomic clinical findings or highly sensitive and specific laboratory tools for the diagnosis of MS. In many cases, a long-term follow-up period is needed to confirm the diagnosis. The aim of this study was to establish whether there are any distinctive features of MS among Korean patients that distinguish it from those observed in Western and other Asian countries.
We included all patients with definite MS who were diagnosed by the criteria of either Poser et al.7 or McDonald et al.8 They were recruited between January 1987 and December 2004 from two tertiary referral university hospitals and one general hospital located in Chungcheong province, which is situated in the central area of South Korea. Patients with "possible" MS according to the criteria of McDonald et al.,8 and those with "probable" MS according to the criteria of Poser et al.7 were excluded from the study. The data from 62 consecutive and unrelated patients (25 men and 37 women) were included in the final analysis. The hospital records regarding their clinical symptoms, disease courses, neurological examinations, laboratory findings, and imaging studies were reviewed retrospectively.
The MS patients were classified into the three clinical subtypes according to the involved site. Those patients whose clinically estimated lesions were confined to the optic nerves and spinal cord were classified as having opticospinal MS. These patients could have minor brainstem signs, such as transient diplopia, nystagmus, and vertigo. Those who showed only spinal cord involvement at different levels and different times were classified as having the spinal form of MS. Patients with lesions at classical multiple sites in the CNS, including the cerebrum, cerebellum, and brainstem, were regarded as having conventional MS.
Descriptive analysis was performed for all variables in the data set. Qualitative variables are described by counts and percentages, while quantitative variables are described by means and standard deviations. Statistical analyses of the clinical and laboratory parameters among the subtypes of MS were performed using ANOVA and the chi-square test. A probability value of p<0.05 was considered statistically significant.
The patients comprised 25 men and 37 women whose age at disease onset was 35.2±13.3 years. The age distribution of symptom onset showed that MS occurs mainly in relatively young adults (Table 1). Familial occurrence of MS was not reported in all patients. Out of 62 patients, 57 (91.9%) had clinically definite MS, and the remaining five patients (8.1%) had laboratory-supported definite MS, as assessed using the criteria of Poser et al.7 Among the 57 patients with clinically definite MS, 55 had experienced more than 2 attacks and had clinical evidence of 2 separate lesions (A1). Five patients with laboratory-supported definite MS had one attack, clinical evidence of one lesion, paraclinical evidence of another, separate lesion, and positive CSF oligoclonal band/IgG (B3). The 62 patients could also be classified into first category patients (n=57, 91.9%) and patients with monosymptomatic presentation (n=5, 8.1%) according to the criteria of McDonald et al.8
The dominant first clinical manifestations originated as a result of myelopathy (54.8%) and optic neuropathy (33.9%; Table 2). Other symptoms or signs were related to brainstem involvement. Symptoms suggestive of lesions in the cerebral white matter or the cerebellum were absent in the first manifestation.
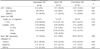
Among the various involved sites, the most common was the spinal cord (n=22, 35.5%), followed by combined involvement of the optic nerve and spinal cord (n=16, 25.8%; Table 3). Table 4 compares the clinical features of the three MS subtypes. The frequency of female patients tended to be higher for those with opticospinal MS than for those with the spinal form of MS, but not higher than for those with the conventional form of MS. There were more male patients than female patients with spinal MS. The age at onset was significantly higher in spinal MS than in opticospinal and conventional MS; however, the age at onset was similar for opticospinal MS and conventional MS. The number of exacerbations among the 62 patients was 3.8±2.6. The number of exacerbations tended to be higher for opticospinal MS than for spinal and conventional MS, but the difference did not reach statistical significance. The interval from the first symptom to the second event or first exacerbation was 35.6±71.1 months (median 9.0 months, range 1-360 months). Opticospinal MS was associated with the shortest interval from the first symptom to the first exacerbation among the three subtypes.
Patients could be subdivided into four groups according to the clinical course of their disease: relapsing-remitting MS (n=46, 74.2%), secondary progressive MS (n=9, 14.5%), progressive-relapsing MS (n=2, 3.2%), and nonprogressing and nonrelapsing (monophasic) MS (n=5, 8.1%; Fig. 1). A situation where relapsing-remitting MS evolves into the course progressing slowly between discrete attacks or instead of the attack is known as secondary progressive MS. The follow-up period was 100.7±96.6 months for relapsing-remitting MS and 49.2±27.6 months for secondary progressive MS (p=0.12).
Bain MRI scans exhibited high-signal-intensity lesions in T2-weighted images in 20 out of 37 patients (54.1%), but only 1 patient exhibited characteristic numerous and confluent multiple white-matter lesions, even some time after the onset of MS. Furthermore, on MRI the cerebellar hemispheric lesions were only seen in one patient. Regarding the MRI characteristics of myelopathy, this study revealed a relatively longer spinalsegment involvement than the two vertebral segments (72.5% vs 27.5%; Table 5). The segments that exhibited an abnormal intensity tended to be longer in spinal MS than in opticospinal and conventional MS, although the difference did not reach statistical significance. The thoracic cord was more frequently involved than the cervical cord.
Only 3 out of 28 patients had a pleocytosis of more than 50 cells/µl in the CSF. The frequency of the presence of oligoclonal IgG bands during the entire clinical follow-up period in patients with any form of MS was very low (11 out of 48 patients, 22.9%; Table 5). The IgG index was obtained in 25 patients by measuring albumin and gamma globulin in both the serum and CSF.2 IgG indices of more than 0.7 were found in 13 patients (52.0%), and a positive response for myelin basic protein was detected in only 5 patients (Table 5).
Abnormal visual evoked potentials, consisting of delayed but well-preserved P100 waves, were recorded in 29 patients (64.4%), whereas the frequency of abnormal brain stem evoked potentials was extremely low (n=5, 12.2%). The rate of abnormalities in somatosensory evoked potentials in the patients with myelopathy was relatively high (n=28, 60.9%; Table 5).
This is the first multiple-hospital-based data analysis of MS patients in central Korea. There are some reports on the various characteristics in Asian- and Western-type MS.3-5 We found several typical clinical features of MS among our Korean patients: (1) a frequent relapsing-remitting course, (2) selective clinical involvement of both the optic nerve and the spinal cord, and (3) fewer lesions on T2-weighted brain MRI images.
Considering the involved site, the most outstanding finding regarding Korean MS is that involvement of the optic nerve or spinal cord there is more common than that of the cerebrum or cerebellum. The most frequent site of single lesions was the spinal cord. Accordingly, the most common first symptoms were related to myelopathy. The symptoms of myelopathy were noted over the entire clinical follow-up period in 84% of our patients. Although the motor weakness and sensory disturbances observed were not attributable entirely to myelopathy, symptoms of conditions other than optic neuropathy and myelopathy were uncommon.9 The proportion of patients with opticospinal MS (16 patients, 25.8%) is similar to that reported for other Asian countries.4,5 The sex ratio (females/males) of our patients was 1.48, which is lower than those in other reported studies involving other Asians and Westerners. A higher female to male ratio and a higher age at onset was observed for the opticospinal form compared with the conventional form among Japanese MS patients.4,5 However, these unique findings were not found in our patients. The frequency of male patients was higher for spinal MS than for the other types (p=0.02). One of the three hospitals from which we gathered data has a center for spinal cord disease. The patients recruited from that hospital had more spinal or opticospinal MS than those from the other two hospitals. In addition, more male patients were recruited from that hospital. This will have affected the sex ratio and age at onset.
The age at onset was higher for spinal MS than for the other two types. The few old patients with conventional MS in our cohort might also have skewed the mean age at onset in that group and for the entire cohort. Given the long-term course of MS, it is sometimes difficult to determine when the first symptom appears. In cases for which there were no medical records, we had to rely upon the memory of patients. These factors need to be taken into consideration when evaluating symptom onset and relapse. The number of exacerbations tended to be higher for opticospinal MS than for spinal and conventional MS. However, the difference regarding the number of exacerbations among the three MS forms did not reach statistical significance.
Regarding the clinical course, the majority of our patients had relapsing-remitting MS. It appears likely that patients with relapsing disease visited a hospital more frequently than those with progressive forms of MS. We assume that a longer observation period in relapsing-remitting MS could exclude the possibility of developing the secondary progressive form in later stages. The interval from first symptom to the first relapse was 35.6±71.1 months, and ranged greatly from 1 month to 30 years; the median value was just 9 months. The very long interval observed for a few patients makes the mean value longer than expected. Therefore, it appears unlikely that some patients in the spinal MS group will develop involvement of either the optic nerve or other CNS sites. The majority of Western patients with relapsing disease exhibit Expanded Disability Status Scale (EDSS) scores of 4.0 or less (self-sustained and fully ambulatory), whereas the majority of patients with progressive disease types have EDSS scores of 6.0 or greater (at least unilateral assistance for walking).10 These findings emphasize the importance of early diagnosis and intervention in patients with relapsing disease to slow or prevent the accumulation of physical disability associated with frequent relapsing or progressive types of this disease.
Regarding the MRI characteristic of myelopathy, this study revealed a relatively longer spinal segment involvement than the two vertebral segments (72.5% vs 27.5%). The thoracic spinal cord was more frequently involved than the cervical cord. These observations have also been made in other Asian and Korean MS patients,4,6,11 but they are uncommon in white people.12 Consensus criteria are needed for defining myelopathy in MS patients, because many Korean MS patients with myelopathy exhibit no compatible MRI lesion in the spinal cord (according to the diagnostic criteria of McDonald et al.)8,11
One of the clinically definite MS criteria put forward by Poser et al. requires evidence from a history of two episodes, signs of one lesion on examination, and evidence from evoked responses or MRI of other lesions (A2). Although 20 out of 37 patients who underwent a brain MRI exhibited the high-signal-intensity lesions on T2 weighted images (54.1%), it is not always easy to differentiate true MS-specific lesions from these findings. Furthermore, the strict criteria of McDonald et al. for positive MRI results are seldom satisfied. Clinicians use evoked potentials in MS suspects to identify clinically unsuspected lesions. However, only three MS suspects in our study were reclassified into the definite MS category as a result of identification of clinically silent lesions based on evoked potentials. In this regard, brain MRI and evoked potentials are useful in only a few cases for identifying patients at risk of developing clinically definite MS. Otherwise, the rate of abnormal visual evoked potentials or somatosensory evoked potentials was relatively high in the patients with optic neuropathy or myelopathy. As a result, the diagnostic value of evoked potentials and MRI for detecting unsuspected MS lesions was very limited in Korean patients. This might be one of the reasons why in this study there were very few patients with clinically definite MS (A2) as defined by the criteria of Poser et al. A MS study involving Japanese patients also found a small number of laboratory-supported definite MS patients compared with a large number of clinically definite MS patients.9
Only 3 out of 28 patients had a pleocytosis of more than 50 cells/µl in the CSF. Although the pleocytosis was noted in more than 10% of our patients, as for the Japanese patients,4 there were too few such patients to allow statistical analysis. The frequency of the presence of IgG oligoclonal bands was lower for opticospinal MS than for conventional or spinal MS. The proportion of elevated IgG indices did not differ among opticospinal, spinal, and conventional MS. Moreover, there was no statistically significant difference in the frequency of either an increased IgG index or the presence of oligoclonal bands among the three types of MS. We could not compare the value of IgG index with those of other studies, because the criteria for elevated IgG index have varied between studies. However, the frequency of an increased IgG index or the presence of oligoclonal bands in any type of MS was lower among Korean patients than among white people. These findings might be strongly associated with the low rates of periventricular and callosal MRI lesions in our patients.13 However, there has been a report of Korean MS patients with a high frequency of the presence of CSF oligoclonal bands.6 Low positive rates of CSF oligoclonal bands in MS could explain why there are fewer patients with laboratory-supported definite MS than with clinically definite MS. Given the strict positive criteria for brain MRI abnormalities defined by McDonald et al.,8 the paucity of typical multiple cerebral and cerebellar white matter lesions on brain MRI in Korean MS patients would reduce further the usefulness of brain MRI as a diagnostic tool for detecting asymptomatic lesions. Cerebellar symptoms are also described only rarely in Japanese patients.9 These limitations of brain MRI and CSF studies hinder the ability of Korean neurologists to make early diagnoses of definite MS.
Whilst we did not perform a genetic study, another unique finding in our Korean patients was the absence of the familial aggregation of MS, which in contrast is well established in white people.2
A serum autoantibody marker of neuromyelitis optica (NMO-IgG) was recently found to be useful for differentiating neuromyelitis optica from MS. It was asserted that neuromyelitis optica is not MS, and that Asian opticospinal MS is the same as neuromyelitis optica.14 However, it is too early to conclude whether or not opticospinal MS is MS or a variant of MS, at least in Asians.15 Further strict diagnostic criteria for each subtype and serological studies involving more Asian MS patients are needed to resolve this issue.
In summary, the results of this study strongly suggest that the clinical features of MS in Korea are in part similar to those in other Asian countries, where MS has a low prevalence. Future studies are needed, including an examination of immunogenetic characteristics and a long-term clinical follow-up based on the objective disability scoring system in Korean MS patients. It will remain difficult to perform a cross-sectional epidemiologic study in the near future because of the high migration rate and low prevalence of MS in Korea.
Figures and Tables
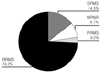 | Figure 1Clinical courses of MS: RRMS; relapsing-remitting MS, SPMS; secondary progressive MS, PRMS; progressive relapsing MS, NPNR; nonprogressing and nonrelapsing MS |
Table 4
Comparison of the clinical findings between opticospinal, spinal and conventional forms of MS

References
1. Mayr WT, Pittock SJ, McClelland RL, Jorgensen NW, Noseworthy JH, Rodriguez M. Incidence and prevalence of multiple sclerosis in Olmsted County, Minnesota, 1985-2000. Neurology. 2003. 61:1373–1377.

2. Ropper AH, Brown RH. Adams and Victor's principles of neurology. 2005. 8th ed. New York: McGraw-Hill;771–796.
3. Kuroiwa Y, Igata A, Itahara K, Koshijima S, Tsubaki T. Nationwide survey of multiple sclerosis in Japan. Clinical analysis of 1,084 cases. Neurology. 1975. 25:845–851.

4. Yamasaki K, Horiuchi I, Minohara M, Kawano Y, Ohyagi Y, Yamada T, et al. HLA-DPB10531-associated opticospinal multiple sclerosis. Clinical, neuroimaging and immunogenetic studies. Brain. 1999. 122:1689–1696.

6. Cho YJ, Jeon BS, Kim YH, Chang KH. Clinical features and outcomes from diagnostic work-up in definite multiple sclerosis. J Korean Neurol Assoc. 1999. 17:823–828.
7. Poser CM, Paty DW, Scheinberg L, McDonald WI, Davis FA, Ebers GC, et al. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol. 1983. 13:227–231.

8. McDonald WI, Compston A, Edan G, Goodkin D, Hartnung H, Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: guidelines from the international panel on the diagnosis of multiple sclerosis. Ann Neurol. 2001. 50:121–127.

9. Houzen H, Niino M, Kikuchi S, Fukazawa T, Nogoshi S, Matsumoto H, et al. The prevalence and clinical characteristics of MS in northern Japan. J Neurol Sci. 2003. 211:49–53.

10. Jacobs LD, Wende KE, Brownscheidle CM, Apatoff B, Coyle PK, Goodman A, et al. A profile of multiple sclerosis: the New York State Multiple Sclerosis Consortium. Mult Scler. 1999. 5:369–376.

11. Kim YH, Chang KH, Kim SS, Park BK, Seong CK, Han MH, et al. Multiple sclerosis of the spinal cord: MR imaging findings. J Korean Radiol Soc. 1988. 39:427–433.

12. Thielen KR, Miller GM. Multiple sclerosis of the spinal cord: Magnetic resonance appearance. J Comput Assist Tomogr. 1996. 20:434–438.

13. Nakashima I, Fujihara K, Miyazawa H, Misu T, Fujimori J, Sato S, et al. Relevance of callosal and periventricular MRI lesions to oligoclonal bands in multiple sclerosis. Acta Neurol Scand. 2006. 113:125–131.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download