Abstract
Background and Purpose
Five single-nucleotide polymorphisms (SNPs) (rs4379368, rs10504861, rs10915437, rs12134493 and rs13208321) were recently identified in a Western population with migraine. These migraine-associated SNPs have not been evaluated in a Han Chinese population. This study investigated the associations of specific SNPs with migraine in a Han population.
Methods
This was a case-control study of Han Chinese residing in Fujian Province. Polymerase chain reaction—restriction-fragment-length polymorphism analysis and direct sequencing were used to characterize the relationships of SNPs in a control group of 200 subjects and in a migraine group of 201 patients.
Results
The frequencies of the five SNPs did not differ between patients with migraine and healthy non migraine controls. However, subgroup analysis indicated certain SNPs were more strongly associated with migraine with aura or migraine without aura than with controls. The CT genotype of rs4379368 was more common in migraine patients with aura (75%) than in migraine patients without aura (47.9%) and controls (48.5%) (p<0.05), and the TT genotype of rs10504861 was more common in migraine patients with aura than in controls (8.3% vs. 0.5%) (p<0.05). Meanwhile, the CC genotype of rs12134493 was less common in migraine patients without aura than in controls (80.6% vs. 88%) (p<0.05).
Migraine is a common disorder that affects about 14% of the adult population worldwide,12 but its etiology and pathogenesis remain poorly understood.3 Epidemiological studies have confirmed that migraine is significantly related to genetic factors and has familial susceptibility, suggesting that pathogenic genes play important roles.45 Linkage studies of family pedigrees have identified regions of the genome and potential genes that may play a role in migraine susceptibility.6 In addition, the increasing knowledge about the underlying pathophysiology of migraines has resulted in the identification of candidate genes in case-control populations, and other potential migraine susceptibility genes have been identified in genome-wide association studies in large case-control cohorts.6
In 2013, Anttila et al.7 performed a meta-analysis using data from 29 clinic- and population-based studies involving 23,285 patients with migraine and 95,425 controls. Twelve single-nucleotide polymorphisms (SNPs) were identified that were associated with migraine susceptibility, of which the following five had not been previously been found to be associated with migraine: rs4379368 [in the succinic HMG coenzyme A transferase gene (C7orf10)], rs10504861 (near the matrix metallopeptidase 16 gene), rs10915437 (near the adherens junction-associated protein 1 gene), rs12134493 [upstream of thetetraspanin 2 gene (TSPAN2)], and rs13208321 (in the four and a half LIM domains protein 5 gene).
Two previous studies have assessed the association of these five SNPs with migraine susceptibility and/or pathogenesis: one involving a Spanish population8 and the other a She Chinese population from Fujian Province, China.9 She people are genetically distinct from other Chinese ethnic populations and have their own lifestyle and cultural heritage.
It is unclear if genetic differences among ethnic groups may impact migraine susceptibility. The present study analyzed the association of these five SNPs with migraine in a Han Chinese population with the aim of determining if genetic differences between ethnic groups affect migraine susceptibility.
This case-controlled study was performed at Ningde Municipal Hospital, Affiliated Hospital of Fujian Medical University. The study was performed in accordance with the Declaration of Helsinki and the principles of the International Conference on Harmonization Guidelines for Good Clinical Practice. This study was approved by the Ethics Committee of our hospital, and all patients provided written informed consents.
Eligible patients with migraine and healthy controls who received a physical examination at Ningde Municipal Hospital were recruited. Eligible patients were older than 15 years and were diagnosed with migraine according to the International Classification of Headache Disorders.10 The healthy controls were also older than 15 years and they had no personal or family history of chronic headache.
The SNPs were characterized using either polymerase chain reaction—restriction-fragment-length polymorphism (PCR-RFLP) analysis (for rs4379368 and rs10915437) or direct sequencing (for rs10504861, rs12134493, and rs13208321). The sequencing primers and PCR-RFLP analysis were performed as described previously.9 The PCR-RFLP products were digested with Hph1 for rs4379368 and MspA1 for rs10915437, and separated by agarose gel electrophoresis. The three genotypes for rs4379368 were CC (two fragments: 179 bp and 79 bp), CT (three fragments: 258 bp, 179 bp, and 79 bp), and TT (one fragment: 258 bp), and those for rs10915437 were AA (two fragments: 280 bp and 130 bp), AG (three fragments: 410 bp, 280 bp, and 130 bp), and GG (1 fragment: 410 bp). The sensitivity and specificity of the PCR-RFLP analysis were evaluated initially in several randomly selected patients.
The rs10504861, rs12134493, and rs13208321PCR products were directly sequenced using capillary gel electrophoresis, which produced PCR products of sizes 166 bp, 381 bp, and 364 bp, respectively. The genotypes identified for rs10504861 were CC, CT, and TT, for rs12134493 they were CC, CA, and AA, and for rs13208321 they were GG, GA, and AA.
Continuous variables were expressed as mean and standard deviation (SD) values, with independent t-tests performed to assess differences between the control and migraine groups. Categorical variables were expressed as counts and percentages, with chi-square or Fisher's exact tests used for group comparisons, as appropriate. Conformity with Hardy-Weinberg equilibrium was evaluated by chi-square goodness-of-fit tests to compare the observed and expected values of the three genotypes for each polymorphism. Univariate and multivariate logistic regressions were performed to detect associations among SNP genotypes and the migraine status, with the multivariate logistic regressions adjusted for age and sex. Since the migraine group was further divided into subgroups of with and without aura, the genotype frequencies were compared between the SNPs and migraine status. Statistical analyses were performed using SPSS statistical software (version 22 for Windows, IBM Corporation, Armonk, NY, USA), with the significance level defined as p<0.05.
The 401 subjects included in this study comprised 200 in the control group and 201 in the migraine group. The demographics of the subjects did not differ significantly between the control and migraine groups (p=0.057) (Table 1). The mean age was about 51 years and most of the subjects were female (the control and migraine groups comprised 72% and 80.1% females, respectively).
All SNPs were found to conform with Hardy-Weinberg equilibrium (Table 2). The frequencies of the genotypes of the different SNPs did not differ between the control and migraine groups (p=0.056) (Table 3). The univariate and multivariate analyses indicated that none of the SNPs in this study were associated with migraine (p=0.067) (Table 3).
We evaluated whether the distribution of SNPs varied between migraine patients with and without aura. Thirty-six patients had migraine with aura (25% males and 75% females) and 165 had migraine without aura (18.8% males and 81.2% females) (p=0.398). The migraine patients with aura were aged 51.47±14.74 years (mean±SD) and those without aura were aged 51.15±12.03 years (p=0.902). The frequencies of three of the five SNPs analyzed (i.e., rs4379368, rs10504861, and rs12134493) differed between control subjects, migraine patients with aura, and migraine patients without aura (Table 4). Most of the patients had migraine without aura (n=165 without aura and n=36 with aura). Subgroup analysis revealed that the distribution of rs4379368 genotypes differed significantly between the control group and the migraine with aura group (p=0.012) (Table 4). The frequency of the different genotypes also differed between the migraine with and without aura groups (p=0.011). The CT genotype was more common in migraine patients with aura (75%) than in controls (48.5%) or migraine patients without aura (47.9%). The frequencies of the rs4379368 genotypes did not differ between the control and migraine without aura groups.
The distributions of the rs10504861 genotypes differed significantly between the control and migraine with aura groups (p=0.016). The CT genotype was less common in the migraine with aura group than in the control group (16.7% vs. 23%), while the TT genotype was more common in the former group (8.3% vs. 0.5%). The frequency of the rs10504861 genotypes did not differ significantly between the migraine with and without aura groups (p>0.05) or between the control and migraine without aura groups (p>0.05).
The CC genotype of rs12134493 was significantly less common in migraine patients without aura than in the control group (80.6% vs. 88%) (p=0.047) (Table 4).
Anttila et al.7 identified 12 SNPs that were associated with migraine susceptibility. The current study evaluated the relationship of 5 of these 12SNPs (rs4379368, rs10504861, rs10915437, rs12134493, and rs13208321) with migraine in a Han population. In contrast to Anttila et al., our multivariate analysis found no associations between any of the five SNPs and migraine. However, subgroup analysis indicated the certain SNPs were more strongly associated with migraine with aura or migraine without aura. The CT genotype of rs4379368 was more common in migraine patients with aura (75%) than in migraine patients without aura (47.9%) or controls (48.5%) (p>0.05). The TT genotype of rs10504861 was more common in migraine patients with aura than in controls (8.3% vs. 0.5%), while the CC genotype of rs12134493 was less common in migraine patients without aura than in controls (80.6% vs. 88%). Our findings suggest that the rs4379368 and rs10504861 SNPs are linked or closely associated with migraine susceptibility genes that influence (either directly or indirectly) the development of migraines with aura, and that rs12134493 is a marker of susceptibility to developing migraine without aura. Additional studies are needed to clarify these findings further.
Our findings differ from those of our previous study that examined the association of these same five SNPs in a She population.9 In contrast to the current study, that previous study found that the rs4379368 SNP did not conform with Hardy-Weinberg equilibrium in the migraine group and that the T allele was more common than the C allele in the She population, possibly indicating the presence of positive genetic selection for the T allele in the She population for migraine. This idea is supported by the observation that the CT and TT genotypes were more common in the She migraine group than the control group (p=0.019). In addition, the presence of the CC genotype was associated with a lower risk of migraine. The CT and TT genotypes were more common in females with migraine than in those without migraine. These findings suggest that being female and carrying the CT or TT genotype increases the risk of having migraines among the She population.
While the frequency of rs4379368 in this study did not differ between migraine patients and control subjects, our data do support the finding that this SNP is associated with migraine susceptibility, in that the CC genotype was less common in migraine patients with aura than in controls or in migraine patients without aura. Our previous study also found that the CC genotype of rs12134493 was more frequent in She males with migraine than in those without migraine. The current study did not evaluate the influence of sex on the migraine associations.
Another difference between the two studies was that the genotypes of rs10504861 did not conform with Hardy-Weinberg equilibrium in both the migraine and control groups in the previous study, while all five SNPs conformed with Hardy-Weinberg equilibrium in the current one. Also, in contrast to our current study, the previous study found no association of rs10504861 with migraine with aura. It also found no difference for rs12134493 between migraine patients without aura and controls. The multivariate analysis performed in the previous study found that the AA and AG genotypes of rs13208321 were associated with a reduced risk of migraine (p=0.039), while no such association of rs13208321 with migraine was found in the present study. Together these findings of our previous and current studies indicate that the genetic susceptibility to migraine may differ between the She and Han populations.
The rs12134493 SNP is located upstream of TSPAN2. TSPAN encodes four transmembrane proteins and is involved in a signal transduction pathway that modulates the development, activation, growth, and movement of cells.11 The possible role of TSPAN in migraine is supported by Esserlind et al.12 finding that the rs2078371SNP located near TSPAN exhibited a significance genome-wide association with migraine in Danish and Icelandic populations. The set of SNPs studied by Esserlind et al. differed from those investigated in our studies, and so additional genetic and molecular studies are needed to further explore the role of TSPAN in migraine.
Our results are similar to those of Sintas et al.8 who evaluated the association of the 12 SNPs analyzed by Anttilaet al. in Spanish migraine patients with aura. Similar to our findings, they found that rs10504861 was associated with migraine with aura. However, they also found rs12134493 to be associated with migraine with aura, whereas we found that this SNP was only associated with migraine without aura. Despite this difference, both studies support rs12134493asa marker of susceptibility to migraine in these two populations. Sintas et al. also found a nominal association of the rs2651899 (within PRDM16) and rs10166942 (near TRPM8) SNPs with migraine with aura. We did not evaluate these two SNPs in either our previous or the present study.
One limitation of this study is the smallness of the sample for migraine patients with aura, and so larger samples are needed to confirm these findings. In addition, several factors are known to influence migraine, such as family history, frequency, duration, pulsing pain, laterality, photophobia, nausea, and aggravation by physical activity.13 We did not assess the relationships of the SNPs evaluated in this study with these migraine-associated characteristics. Also, our previous analysis of a She population identified differences in specific genotypes between sexes.9 In the present study the sex ratio differed between the control (28% males and 72% females) and migraine (19.9% males and 80.1% females) groups (p=0.057). Although this difference did not reach statistical significance, a marginal difference in the sex ratio between the migraine and control groups may have impacted our results. The small number of migraine patients with aura (n=36) also limits the generalizability of the findings. Future studies with larger populations are needed to further evaluate the associations of these SNPs with migraine with aura.
Several large genome-wide association studies have identified genetic loci that could be associated with migraine susceptibility. 71415161718 We found that the CC genotype of rs4379368 and the TT genotype of rs10504861 may increase the risk of experiencing migraine with aura, and that the CC genotype of rs12134493 may reduce the susceptibility to migraine without aura. These findings and those of our previous study suggest that there are genetic differences in migraine susceptibility between the She and Han populations, and they raise the possibility that ethnicity differences across other populations can impact migraine.
Figures and Tables
Table 1
Demographics distribution of the study subjects

| Control (n=200) | Migraine (n=201) | p | |
|---|---|---|---|
| Sex | 0.057 | ||
| Male | 56 (28%) | 40 (19.9%) | |
| Female | 144 (72%) | 161 (80.1%) | |
| Age (years) | 50.84±12.11 | 51.2±12.52 | 0.764 |
Table 2
Hardy-Weinberg equilibrium and genotype frequencies
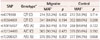
Table 3
Comparison of SNP genotypes between the control and migraine groups and associations with migraine status

Table 4
Comparison of SNP genotypes between migraine with aura, migraine without aura, and controls

Acknowledgements
This work was supported by grant 2014-CXB-26 from the Fujian Medical Innovating Program, Research Foundations for Young Scholars, Health Department of Fujian Province (Grant No.2014-1-99) and The Ningde Planning Project of Science and Technology (Grant No.20140113)
We would like to extend our thanks to all participants of this study.
References
1. Stovner LJ, Hagen K. Prevalence, burden, and cost of headache disorders. Curr Opin Neurol. 2006; 19:281–285.

2. Bigal ME, Lipton RB. The epidemiology, burden, and comorbidities of migraine. Neurol Clin. 2009; 27:321–334.

3. Paemeleire K, Louis P, Magis D, Vandenheede M, Versijpt J, Vandersmissen B, et al. Diagnosis, pathophysiology and management of chronic migraine: a proposal of the Belgian Headache Society. Acta Neurol Belg. 2015; 115:1–17.

4. Ulrich V, Gervil M, Kyvik KO, Olesen J, Russell MB. Evidence of a genetic factor in migraine with aura: a population-based Danish twin study. Ann Neurol. 1999; 45:242–246.

5. Lemos C, Castro MJ, Barros J, Sequeiros J, Pereira-Monteiro J, Mendon-a D, et al. Familial clustering of migraine: further evidence from a Portuguese study. Headache. 2009; 49:404–411.

6. Gasparini CF, Sutherland HG, Griffiths LR. Studies on the pathophysiology and genetic basis of migraine. Curr Genomics. 2013; 14:300–315.

7. Anttila V, Winsvold BS, Gormley P, Kurth T, Bettella F, McMahon G, et al. Genome-wide meta-analysis identifies new susceptibility loci for migraine. Nat Genet. 2013; 45:912–917.
8. Sintas C, Fernández-Morales J, Vila-Pueyo M, Narberhaus B, Arenas C, Pozo-Rosich P, et al. Replication study of previous migraine genome-wide association study findings in a Spanish sample of migraine with aura. Cephalalgia. 2015; 35:776–782.

9. Lin QF, Fu XG, Yao LT, Yang J, Cao LY, Xin YT, et al. Association of genetic loci for migraine susceptibility in the she people of China. J Headache Pain. 2015; 16:553.

10. Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders: 2nd edition. Cephalalgia. 2004; 24:Suppl 1. 9–160.
11. Lafleur MA, Xu D, Hemler ME. Tetraspanin proteins regulate membrane type-1 matrix metalloproteinase-dependent pericellular proteolysis. Mol Biol Cell. 2009; 20:2030–2040.

12. Esserlind AL, Christensen AF, Le H, Kirchmann M, Hauge AW, Toyserkani NM, et al. Replication and meta-analysis of common variants identifies a genome-wide significant locus in migraine. Eur J Neurol. 2013; 20:765–772.

13. Chasman DI, Anttila V, Buring JE, Ridker PM, Schürks M, Kurth T, et al. Selectivity in genetic association with sub-classified migraine in women. PLoS Genet. 2014; 10:e1004366.

14. Chasman DI, Schürks M, Anttila V, de Vries B, Schminke U, Launer LJ, et al. Genome-wide association study reveals three susceptibility loci for common migraine in the general population. Nat Genet. 2011; 43:695–698.

15. Ghosh J, Pradhan S, Mittal B. Genome-wide-associated variants in migraine susceptibility: a replication study from North India. Headache. 2013; 53:1583–1594.

16. Iizuka T, Takahashi Y, Sato M, Yonekura J, Miyakawa S, Endo M, et al. Neurovascular changes in prolonged migraine aura in FHM with a novel ATP1A2 gene mutation. J Neurol Neurosurg Psychiatry. 2012; 83:205–212.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download