Dear Editor,
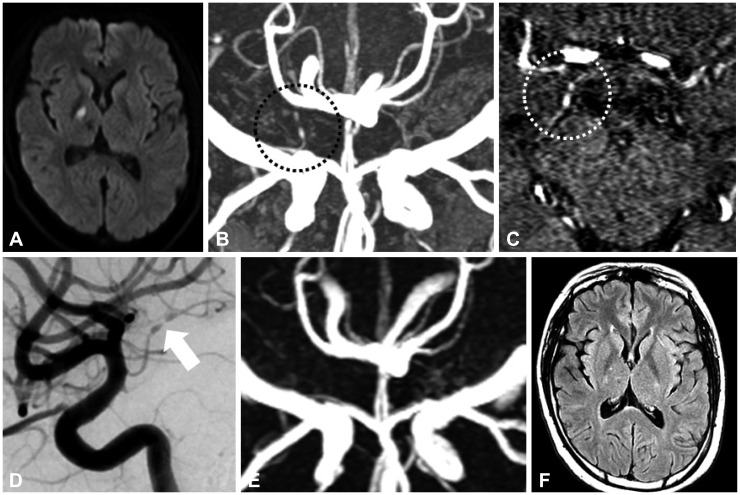
A 29-year-old female who had been treated in another hospital and who had a history of two stroke attacks was admitted with newly developed dysarthria. The two previous stroke attacks were lacunar syndromes caused by a right anterior thalamic infarction and a left lateral medullary infarction at 11 and 8 months prior to admission to our hospital, respectively. She denied having any conventional risk factors. On examination she was found to have moderately decreased sensation in the left side without any sequelae from the previous attacks. She was taking clopidogrel, warfarin, and rosuvastatin. Her initial international normalized ratio value for the prothrombin time was 2.38. Diffusion-weighted images obtained on her admission day showed an acute infarction in the right internal capsule (Fig. 1A). Her 3D and source images of time-of-flight magnetic resonance angiography (MRA) revealed abnormal dilatation and narrowing in a branch of the right distal internal carotid artery (Fig. 1B and C).
We performed a lumbar puncture on the fifth day after admission. The findings for the cerebrospinal fluid, including the cell count, were normal. Conventional angiography revealed a characteristic beading pattern, consistent with vasculitis in the right anterior choroidal artery (Fig. 1D). The results of the laboratory tests for vasculitis can be summarized as positivity for antinuclear antibody (ANA) at a dilution of 1:640 with a homogeneous and speckled pattern, and for anti-double-stranded DNA (anti-dsDNA) at a dilution of 1:80. She was diagnosed with systemic lupus erythematosus (SLE) based on oral ulcers, proteinuria of 3+, positive ANA, and positive anti-dsDNA in accordance with the 2015 revised criteria of the American College of Rheumatology/Systemic Lupus International Collaborating Clinics.
The immunosuppressant of hydroxychloroquine was added to her steroid therapy for treating the central nervous system (CNS) lupus for several weeks after admission. The abnormal findings for the right anterior choroidal artery had disappeared at follow-up MRA performed 1 year after starting steroid and immunosuppressive therapy (Fig. 1E). The follow-up fluid-attenuated inversion recovery image showed only a subtle old lesion in the right internal capsule (Fig. 1F).
Ischemic stroke caused by lupus vasculitis is rare. Although magnetic resonance (MR) imaging is sensitive for CNS vasculitis,1 the findings of MRA evaluating vasculitis caused by SLE may be mostly normal since mainly small vessels are affected by lupus.2 Our case of lupus vasculitis shows two rare features: 1) vasculitis with a beading pattern appearing as narrowing and ectasia in the anterior choroidal artery and 2) abnormal findings for the anterior choroidal artery were detected in 3D-reconstructed MRA images as well as in conventional angiography.
The main pathology of arteritis caused by collagen disease is fibrinoid degeneration in the arterial walls.3 While endothelial proliferations with destroyed muscular and elastic tissue are associated with arterial narrowing, weakening of the walls with smaller extents of endothelial hyperplasia may produce ectasias.3 This beading pattern of arteritis is easiest to detect using conventional angiography. However, developments in MR techniques mean that MRA can be used to reveal such findings in large intracranial arteries. A normal anterior choroidal artery can be identified partly on a 1.5-T MRA source image and completely in 3.0-T MRA.4 Moreover, an abnormal anterior choroidal artery affected by vasculitis can be seen on source and 3D-reconstructed images of 3.0-T MRA, as in the present case. Source images only provide subtle indications of narrowing and ectasia of the artery, while 3D images of brain MRA may show definite beading patterns of the anterior choroidal artery. The change of this abnormal finding can be also checked in follow-up MRA, as in our case.
Even though lupus vasculitis usually occurs in small arteries, MRA may be a clue to identify the pathogenesis of the intracranial arteries that are relevant to an infarcted lesion.
References
1. Pomper MG, Miller TJ, Stone JH, Tidmore WC, Hellmann DB. CNS vasculitis in autoimmune disease: MR imaging findings and correlation with angiography. AJNR Am J Neuroradiol. 1999; 20:75–85. PMID: 9974060.
2. Hess DC. Cerebral lupus vasculopathy. Mechanisms and clinical relevance. Ann N Y Acad Sci. 1997; 823:154–168. PMID: 9292042.
3. Ferris EJ, Levine HL. Cerebral arteritis: classification. Radiology. 1973; 109:327–341. PMID: 4147505.

4. Wiesmann M, Yousry I, Seelos KC, Yousry TA. Identification and anatomic description of the anterior choroidal artery by use of 3D-TOF source and 3D-CISS MR imaging. AJNR Am J Neuroradiol. 2001; 22:305–310. PMID: 11156774.
Fig. 1
Diffusion-weighted image of the 29-year-old female showing an acute infarction in the right internal capsule (A). Her 3D and source images of brain magnetic resonance angiography (MRA) reveal dilatation and narrowing in a branch of the right distal internal carotid artery as a distinct pattern of vasculitis (B and C, circled). The conventional angiography shows a definite beading pattern of the right anterior choroidal artery (D, white arrow). This finding had normalized in MRA at the 1-year follow-up (E). Only a subtle lesion in the right internal capsule related to this attack and an old lesion in the right anterior thalamus related to the first attack were seen in the 1-year follow-up fluid-attenuated inversion recovery image (F). All magnetic resonance imaging was performed using a 3.0-T Achieva TX scanner (Philips Healthcare, Best, the Netherlands).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download