Dear Editor,
Surfer's myelopathy (SM) is a rare, acute spinal injury that is presumed to involve the major blood vessel supplying the thoracolumbar segment of the spinal cord. The injury typically follows prolonged hyperextension of the back. This condition was coined SM because it is seen most often in beginner surfers. Here we describe a case of a patient with SM that required differentiation from long extensive transverse myelitis and spinal cord infection.
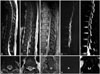
A previously healthy 34-year-old man was transferred to our institute from a hospital in Hawaii due to complete paraplegia and fever. About 90 minutes after his first surfing lesson ever in Hawaii, he experienced back pain radiating down to his lower limbs without any traumatic events. The back pain progressed to complete paraplegia and total sensory loss on both legs within 30 minutes. The next day he was transferred to our hospital by airplane. On admission day 1 his body temperature was 38.0℃. A neurologic examination revealed complete paraplegia of grade A on the American Spinal Injury Association Impairment Scale, with T10-level sensory deficit and the absence of rectal tone. His bladder was distended. Initial magnetic resonance imaging (MRI) performed 2 days after symptom onset showed a T2-weighted hyperintensity from T5 to the conus medullaris (Fig. 1A and B). Laboratory findings were within the normal ranges except for creatinine kinase (15,825 IU/L), myoglobin (1,582 ng/mL), and C-reactive protein (10.24 mg/L). Blood and urine cultures were negative. A cerebrospinal fluid (CSF) analysis revealed a white blood cell count of 280/µL, red blood cell count of 230/µL, protein concentration of 76.5 mg/dL, immunoglobulin G (IgG) index of 0.683, and the absence of oligoclonal bands. Brain MRI findings were normal. Immunologic profiling for various antibodies, including neuromyelitis optica-IgG antibody, produced negative results.
Due to the presence of fever and CSF pleocytosis, infectious myelitis was initially suspected. The patient was treated with intravenously administered broad-spectrum antibiotics, acyclovir, and high-dose steroids. Despite these treatments, which included high-dose steroid pulse therapy of two cycles for 2 weeks, no neurologic improvement was observed. Follow-up MRI at 2 weeks showed increased T2-weighted signal intensity of the previous hyperintensity and a new abnormal enhancement from levels T10 to T12 (Fig. 1C-F). Spine diffusion-weighted MRI (DWI) showed restricted diffusion at the affected level, suggesting spinal cord infarction (Fig. 1G-J). His clinical status had not changed significantly despite rehabilitation for 2 months since hospital discharge.
SM is an acute nontraumatic myelopathy that occurs due to prolonged hyperextension of the back in beginner surfers.1 Most patients experience acute back pain followed by bilateral motor weakness and variable sensory loss in the lower extremities.12 Since the first description by Thompson et al.1 in 2004, only a few cases have been reported in the literature. Although the exact mechanism of injury is poorly understood, prolonged spinal hyperextension while lying prone on a surfboard may produce spinal cord arterial insufficiency and subsequent ischemia.134
While there was some evidence of infection, the sudden onset of symptoms after surfing, restricted diffusion on DWI, and lack of any improvement in neurologic symptoms led us to a diagnosis of SM rather than infectious myelitis in the present case. Rhabdomyolysis, which might develop during a long airplane flight (due to prolonged sitting with complete paraplegia), may be the reason for fever.5 The CSF profile was also consistent with infarction of the cord, which can contain both blood and inflammatory cells as well as elevated protein levels, especially in cases with complete long-segment cord infarction.2
Surfing is a sport that is growing rapidly in popularity. The incidence of both traumatic and nontraumatic spinal cord injuries associated with this sport will therefore undoubtedly increase in the future. Increased awareness of this injury may enable physicians to recognize SM earlier.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download