Abstract
Background and Purpose
The objective of this study was to determine the prevalence of and risk factors for dementia in residents aged 65 years and older in a Chinese nursing home.
Methods
A cross-sectional study was carried out in a nursing home located in Hangzhou, Zhejiang Province, China. Cognitive status, including the presence of dementia and mild cognitive impairment (MCI), was measured using a combination of medical history and objective cognitive assessments. Logistic regression analysis was conducted to predict the associated risk factors.
Results
In total, 943 residents (334 males and 609 females) aged 84.00±6.67 years (mean±SD) were included. Dementia was diagnosed in 420 (44.5%) residents, and MCI was diagnosed in 195 (20.7%). Mild, moderate, and severe dementia were present in 20.3%, 14.0%, and 65.7% of those in the dementia group, respectively. Logistic regression analysis revealed that dementia was associated with a low education level (p=0.000), an advanced age (p=0.010), and a history of stroke (p=0.023).
Conclusions
Our study found a high prevalence of dementia in a Chinese nursing home, and a high prevalence of patients with severe dementia. Risk factors for dementia included a low educational level, an advanced age, and a history of stroke. Appropriate interventions need to be applied to this population.
The global elderly population is steadily increasing, including in China. In total, 131 million Chinese were aged over 65 years by the end of 2013, representing about 9.6% of the total population (http://data.stats.gov.cn). The Chinese Academy of Social Sciences has predicted that China will be the most-aged society in the world by 2030. An aging population alters disease spectrum and pension models, and dementia has become one of the most serious medical and societal problems in China. With the largest population experiencing this type of disease in the world, the number of dementia cases in China increased from 3.68 million in 1990 to 9.19 million in 2010.1
Family support was traditionally the main modality by which Chinese elderly people were cared for. However, this situation has recently changed significantly. Smaller family sizes and greater geographic mobility have reduced the availability of adult children to assist in caring for elderly family members.2 More and more Chinese families have accepted the idea of transferring their elders to institutional care in nursing homes and, according to one survey conducted in 2010, 11.3% of the elderly population living in urban areas was willing to receive care in institutions.3
Previous research has found that cognitive impairment is one of the most important risk factors leading to the transfer of elderly people to nursing homes,4 especially those with severe cognitive impairment, behavioral symptoms, and depression, and those unable to perform the basic activities of daily living.5 On the other hand, elderly subjects with normal cognition at admission are at increased risk of developing dementia during their stay in a nursing home. These characteristics result in the prevalence of dementia being higher in the nursing-home population than in the community population.6 Thus, it is important to recognize the presence of cognitive impairment in nursing-home residents, and provide effective treatment for these patients. However, there is a lack of comprehensive data on the cognitive status of individuals in nursing homes in China.
The purpose of this study was twofold: 1) to elucidate the cognitive status of elderly people and the prevalence of dementia in a single Chinese nursing home and 2) to identify possible risk factors associated with dementia in a nursing home.
A cross-sectional study was conducted in a Chinese nursing home in Hangzhou City, which is the capital and largest city of Zhejiang Province in southeastern China, with a residential population of about 8.84 million at the end of 2013. All residents aged 65 years and over were eligible to participate in the study. Family members provided informed consent and all participants provided written assent. The study was approved by the Ethics Committee of Zhejiang Hospital.
Information on cognitive status was obtained from both the subjects and their caregivers or relatives. Cognitive functions were assessed using the Mini Mental State Examination (MMSE). Diagnoses of dementia and mild cognitive impairment (MCI) were made using the 2011 National Institute of Aging and Alzheimer's Association criteria;78 while dementia severity was assessed using the Clinical Dementia Rating Scale (CDR). The CDR classifies dementia according to the following global scores: 0, normal; 0.5, very mild dementia; 1, mild dementia; 2, moderate dementia; and 3, severe dementia. The CDR sum-of-boxes (CDR-SB) score varies from 0 to 18, and enables a quantitative evaluation of cognitive impairment.
The participants were grouped into two categories for the analysis: dementia and nondementia; where the nondementia group included those with MCI or normal cognitive function. Distributions of qualitative variables are described as frequencies and percentages, and quantitative variables are presented as mean±SD values. Differences between categorical variables were compared with the chi-square test. The mean values were compared between two groups with the dependent-samples t-test or the Mann-Whitney U test. Bivariate correlations were calculated to determine which variables were associated with dementia, and the relationship between dementia and these independent variables was analyzed by developing logistic regression models. All statistical analyses were performed using SPSS software (version 19.0). Differences were considered statistically significant for p values of less than 0.05.
In total, 1,154 subjects aged 65 years and older were initially enrolled in the study, of whom 211 (18.3%) were excluded for the following reasons: refusal to participate, severe auditory or visual deficits, language problems, or loss to follow-up. Consequently, 943 subjects were included in the final analysis, comprising 609 (64.6%) females and 334 (35.4%) males. The subjects were aged 84.00±6.67 years, ranging from 65 to 103 years.
Most of the subjects had a poor educational background, with 28.2% classified as illiterate, 24.2% educated to primary school level, 31.0% to middle school level, and 16.6% to high school level. Over half of subjects (59.3%) were widowed. Comorbid conditions diagnosed in study participants, in order of decreasing frequency, were hypertension (55.9%), coronary disease (28.5%), diabetes (20.1%), and stroke (18.9%). Detailed information is presented in Table 1.
In total, 420 subjects (44.5%) were diagnosed with dementia, while 195 subjects (20.7%) were diagnosed with MCI. A scored of 0 points on the MMSE was present in 211 subjects (22.4%). The MMSE score was 6.00±7.75 for patients with dementia and 21.98±4.35 for patients with MCI. The CDR-SB score was 14.32±5.06 for patients with dementia and 2.13±1.14 for patients with MCI. Among the dementia subjects, the cognitive status on the CDR was distributed as follows: 11 (2.6%) had a CDR score of 0.5, 74 (17.7%) scored 1, 59 (14.0%) scored 2, and 276 (65.7%) scored 3.
To identify possible risk factors, we compared selected factors between dementia subjects and nondementia subjects (including MCI subjects). Table 1 indicates that a diagnosis of dementia is associated with patient age (p=0.040), and in a subgroup analysis of eight age groups, with each group covering 5 years, the statistical significance of the associating increased with age (p=0.001). There were also significant differences in the level of education attained (p=0.000) and marital status (p=0.000) with age. Dementia subjects were more likely to have had a stroke (p=0.004); however, there were no significant differences observed for other diseases such as hypertension, coronary artery disease, and diabetes. There were no significant differences with respect to sex.
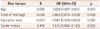
Logistic regression models were developed to analyze the relationships between dementia and the independent variables. The results showed that those with a lower education level (p=0.000), an advanced age (p=0.010), or a prior history of stroke (p=0.023) were more likely to have dementia (Table 2).
This was the first observational study to analyze the prevalence of dementia in a Chinese nursing home. Our study found the prevalence rates of dementia and MCI in this setting to be 44.5% and 20.7%, respectively, suggesting that more than half of nursing-home residents have some form of cognitive impairment. The prevalence of dementia has been reported to vary in different regions and countries: 48.2%9 in US nursing homes, 50.7%10 in Italian nursing homes, 47.6%11 to 51.8%6 in German nursing homes, and 59.1%12 in Hong Kong nursing homes. The small differences between these studies may be a consequence of the application of different diagnostic criteria and the inclusion of diverse study populations. In our study, we excluded some potential subjects for various reasons, including severe auditory and visual deficits; these conditions may be associated with dementia, and so their exclusion may have biased our results. However, one recent study found that the prevalence of dementia among Chinese people aged 60 years and older was 7.7%.13 Our data showed that the prevalence of dementia was significantly higher in a nursing home than in the community. Moreover, this difference may be even more marked in other parts of China, since the Hangzhou district has a strong economy and good health-care services relative to much of China.
Mild, moderate, and severe dementia were present in 20.3%, 14.0%, and 65.7% of the subjects in the dementia group, respectively. This indicates that nearly two-thirds of patients are at a late stage of dementia, and they will be entirely dependent on others for their survival. During the investigation, we found that only 8.81% (37/420) of the dementia patients received regular treatment with antidementia medication, and none of them received cognitive rehabilitation therapy. Antipsychotic drugs were the most common class of drugs used for controlling associated symptoms of dementia, being used in 10.95% (46/420) of the patients. Our findings are not dissimilar to those of an Italian study conducted in nursing homes, in which the proportion of dementia residents receiving drug treatment was only 5%.10
It is widely believed that dementia is influenced by many factors, including age, sex, education level, and the specific disease history. Consistent with a previous study,10 we found no effect of sex on the risk of dementia. However, other authors have reported different findings; for example, one study estimated that almost two-thirds of individuals diagnosed with Alzheimer disease are women.14 These conflicting findings may result from the inclusion of small samples at the upper range of the age distribution, the use of different diagnostic criteria, and differences due to specific social, culture, and historical factors.1516
The role of age as a risk factor for nursing-home dementia is also controversial. A study of nursing homes in Germany found that the prevalence of dementia was not affected by age.6 However, in our study the prevalence of dementia increased with age, ranging from 37% in those aged 70–75 years to 66.7% in those aged 95+ years. Although the prevalence in those aged 65–70 years was 55.6%, this group included a relatively small number of subjects, and so the statistical calculations may have unreliable. Future studies should include larger samples so that the effect of age can be determined more accurately. Moreover, the high prevalence of dementia among those aged 65–70 years may also explain the reason why these relatively young people were admitted to the nursing home.
A history of stroke increased the risk of dementia in the present nursing-home patients. Stroke is the main reason for vascular dementia, which is a common type of dementia. Unfortunately, we were unable to classify the dementia type in our subjects because of a lack of reliable information on their medical histories.
We found an inverse relationship between the prevalence of dementia and the highest educational level achieved, with the risk of dementia being lower in highly educated subjects. The access to a senior-high-school education has improved steadily in recent years in China, but the proportion of high-school-educated people in the population remains lower than that in developed countries. In order to prevent or delay dementia, the effect of education should be considered when formulating government policies.
In conclusion, this study was an initial trial investigating the cognitive status of individuals in a nursing home in China. The results indicate that the prevalence of dementia in the elderly inhabitants of nursing homes is high. Risk factors associated with dementia include an advanced age, a prior history of stroke, and a low education level. Despite the high prevalence of dementia, the awareness of and effective treatments for this disease remain woefully inadequate in China.
Figures and Tables
Table 1
Demographic profile of residents in the nursing home with dementia and without dementia

Acknowledgements
This study was supported by grants from the International Science & Technology Cooperation Program of China (No. 2014DFT30100), and Zhejiang Provincial Science and Technology Project (No. 2014C33242).
References
1. Chan KY, Wang W, Wu JJ, Liu L, Theodoratou E, Car J, et al. Epidemiology of Alzheimer's disease and other forms of dementia in China, 1990-2010: a systematic review and analysis. Lancet. 2013; 381:2016–2023.

2. Guan X, Zhan HJ, Liu G. Institutional and individual autonomy: investigating predictors of attitudes toward institutional care in China. Int J Aging Hum Dev. 2007; 64:83–107.

3. Wu YS, Guo P, Miao WS, Deng B. Data analysis of the sampling survey of the aged population in urban/rural China 2010. 2nd ed. Beijing: China Society Press;2014.
4. Dramé M, Lang PO, Jolly D, Narbey D, Mahmoudi R, Lanièce I. Nursing home admission in elderly subjects with dementia: predictive factors and future challenges. J Am Med Dir Assoc. 2012; 13:83.e17–83.e20.

5. Gaugler JE, Yu F, Krichbaum K, Wyman JF. Predictors of nursing home admission for persons with dementia. Med Care. 2009; 47:191–198.

6. Hoffmann F, Kaduszkiewicz H, Glaeske G, van den Bussche H, Koller D. Prevalence of dementia in nursing home and community-dwelling older adults in Germany. Aging Clin Exp Res. 2014; 26:555–559.

7. McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, et al. The diagnosis of dementia due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011; 7:263–269.

8. Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer's disease: recommendations from the National Institute on Aging-Alzheimer's Association workgroups on diagnostic guidelines for Alzheimer's disease. Alzheimers Dement. 2011; 7:270–279.

9. Magaziner J, German P, Zimmerman SI, Hebel JR, Burton L, Gruber-Baldini AL, et al. The prevalence of dementia in a statewide sample of new nursing home admissions aged 65 and older: diagnosis by expert panel. Epidemiology of Dementia in Nursing Homes Research Group. Gerontologist. 2000; 40:663–672.

10. Cherubini A, Ruggiero C, Dell'Aquila G, Eusebi P, Gasperini B, Zengarini E, et al. Underrecognition and undertreatment of dementia in Italian nursing homes. J Am Med Dir Assoc. 2012; 13:759.e7–759.e13.

11. Jakob A, Busse A, Riedel-Heller SG, Pavlicek M, Angermeyer MC. [Prevalence and incidence of dementia among nursing home residents and residents in homes for the aged in comparison to private homes]. Z Gerontol Geriatr. 2002; 35:474–481.
12. Cheng ST, Lam LC, Chow PK. Under-recognition of dementia in long-term care homes in Hong Kong. Aging Ment Health. 2012; 16:516–520.

13. Ji Y, Shi Z, Zhang Y, Liu S, Liu S, Yue W, et al. Prevalence of dementia and main subtypes in rural northern China. Dement Geriatr Cogn Disord. 2015; 39:294–302.

14. Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology. 2013; 80:1778–1783.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download